Bordetella pertussis and the Importance of Vaccination
Introduction and History

By Alexandra White
At right is a sample image insertion. It works for any image uploaded anywhere to MicrobeWiki.
The insertion code consists of:
Double brackets: [[
Filename: download.jpg
Thumbnail status: |thumb|
Pixel size: |300px|
Placement on page: |right|
Legend/credit:
Closed double brackets: ]]
Other examples:
Bold
Italic
Subscript: H2O
Superscript: Fe3+
Vaccination is a widely used practice to help prevent infectious disease and commonly spread illnesses. A widely known and common vaccine is used to prevent infection of Bordetella pertussis, the causative agent of Whooping cough. Whooping cough is known as one of the most common infectious disease deaths in the world[1]. The disease results in over 50 million cases worldwide per year, with the majority being unvaccinated individuals present in Third World Countries[1].
B. pertussis is spread through coughing and sneezing and symptoms first appear seven to ten days after infection[2]. These symptoms include: fever, runny nose, coughing which develops into a whooping cough, and phenomena[2]. Those infected with pertussis are contagious for around three weeks once coughing is displayed as a symptom yet symptoms can last up to eight weeks[2].
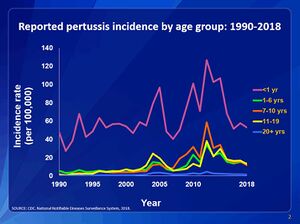
B. pertussis was first discovered and isolated to be the cause of whooping cough in 1906 [1].Compared to human infectious diseases pertussis is a relatively recent human infectious disease that first appeared in France in 1414[3].The disease was identified in Paris, France in 1900 by Jules Bordet and Octave Gengou who obtained the sample from a 5-month-old child[3]. The bacteria was finally isolated in 1906 from Jules Bordet’s own son[1]. A vaccine for B. pertussis was developed in the early 1940s [4]. Before the development of the vaccine there were over 200,000 cases in the United States reported annually and with widespread use incidence has decreased 75% compared to the pre-vaccination era[4].
Bordetella pertussis and Infection Stages
Italic
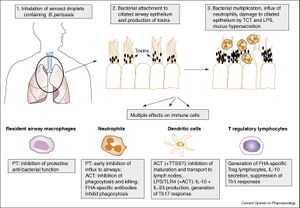
B. pertussis is a gram-negative, aerobic coccobacillus bacteria a part of the genus Bordetella[3]. Pertussis is a human-specific pathogen causing severe respiratory disease that cannot survive outside of its host[3]. Infection occurs with B. pertussis entering through the host airway via respiratory droplets from an already infected individual, usually from coughing [5]. B. pertussis then proceeds down the respiratory tract and adheres to ciliated epithelial cells in the trachea and nasopharynx [5]. Once the bacteria is attached it begins to replicate and colonies with-in the host cells [5]. Toxins are secreted by micro-organism which inflict damage to the epithelial lining, resulting in loss of ciliated cells which induces the coughing most commonly associated with whooping cough [5]. The pertussis toxins released also allow the bacteria to avoid host immune response by interfering with clearance mechanisms [5]. The damage caused by the toxins released by the replicating bacteria also halts ciliary function, short-circuiting host G proteins signaling apparatus, and also inhibits immune cell functions by up regulating cAMP levels [5].
B. Pertussis Vaccine History
Include some current research, with at least one figure showing data.
Italic
Soon after B. pertussis was isolated as the causative agent of whooping cough, Pertussis whole-cell (Pw) vaccines were implemented using heat-killed bacteria [3]. Pw vaccines became used for wholesale distribution starting in the 1940’s [6]. Since B. pertussis in human host resrictive, there is a very low display of genetic diversity [3]. Recent analyses have concluded that there were several different types of isolates circulating in the prevaccine era that produce various proteins [3]. Only one or two types predominated with no significant difference in an associated pattern to which was the dominant isolate [3]. This allowed for the Pw vacine to be composed of 1-3 strains selected from the predominant isolate types [3]. Pw vaccines were given to infants and toddlers extensively due to the majority of infections occuring in younger children [3]. Where vaccine distribution was effective, vaccine strains of B. pertussis were low and in areas with low vaccination rates the pre-vaccine era isolated were still circulating [3]. Pw vaccines were shown to create immunity for some isolates of B. pertussis but not all isolates [3].
Vaccine Virulence
Include some current research, with at least one figure showing data.
Why Vaccination?
Conclusion
References
- ↑ 1.0 1.1 1.2 1.3 Kerr, J.R. and Matthews, R.C."Bordetella pertussis Infection: Pathogenesis, Diagnosis, Management, and the Role of Protective Immunity." 2000. European Journal of Clinical Microbiology and Infectious Disease 19:77-88.
- ↑ 2.0 2.1 2.2 World Health Organization: Pertussis 2018
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 Guiso, N. "Bordetella pertussis and Pertussis Vaccines." 2009. Clinical infectious Diseases 49:1565-1569.
- ↑ 4.0 4.1 Havers et al. "Pertussis." 2021. Center for Disease Control and Prevention. 1-16.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 Smith, A.M et al. "The virulence factors of Bordetella pertussis: a matter of control" 2001. FEMS Microbiology Reviews 25:309-333.
- ↑ Mattoo, S. Cherry, J.D. "Molecular Pathogenesis, Epidemiology, and Clinical Manifestations of Respiratory Infections Due to Bordetella pertussis and Other Bordetella Subspecies" 2005. Clinical Microbiology Reviews
Authored for BIOL 238 Microbiology, taught by Joan Slonczewski, 2022, Kenyon College
