Long covid and the brain
Introduction
Overview of long COVID
Long COVID or Post COVID conditions, also known as post-acute sequelae of SARS-CoV-2 infection(PASC),refers to a range of symptoms that continue for weeks, months, or even years after the patient initially recovering from the coronavirus disease(COVID-19). The condition can affect anyone who was infected by COVID-19, regardless of the severity of their initial infection. The symptoms of long term COVID can various between each individual and be very complicated because it sometimes impact multiple organism systems. The complexity of the symptoms often leads to post-COVID conditions being diagnosed as other diseases.
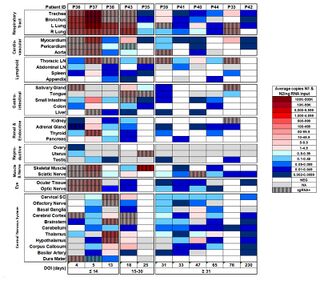
Although COVID is primarily target to respiration systems, there is growing evidence that COVID-19 can have long-term effects on the brain, including potential links to increased risks of neurological diseases like Parkinson's and Alzheimer's disease in the future. Corona virus was unusual because it had been found the virus across blood-brain barrier. The dissecting samples shows the virus is preserved in brain tissue over months and it is still active[1].
Neurological Symptoms
Diagnosis and Evaluation
Diagnose Long COVID is an exclusion process, indicating that it is only diagnosed after doctor excluding all the possible disease or causes that lead the symptoms. It is a tricky process that for sometimes doctors will reveal some hidden diseases that even the patient doesn't know before. In order to make precise diagnose, it always need to go through a comprehensive diagnose process including physical examination, laboratory test and imaging such as blood test, chest X-rays, cardiac testing, pulmonary function test, multidisciplinary approaches such as psychiatric diagnose if necessary. Due to the various symptoms patient experienced, there is no standard treatment for long COVID.
Common Symptoms
Brain Fog: Brain fog a range of neuron-cognitive symptoms that including forgetfulness, problem of focusing, concentrating, and paying attentions. These symptoms can last for weeks and months after the patient get initial infections[2].
Sleep Disturbance: Approximately 40% of people with long COVID reported major changes of their sleep after COVID-19. People have experienced COVID-19-associated sleep disorders including insomnia and restless leg syndrome[3][4].
Anxiety,depression, and stress:People who have had COVID-19 may experience mood disorders including constantly feeling anxiety, depression, and stress.
Post-exertional malaise:Post-exertional malaise is one of the most common symptoms patient experience after recovered from COVID-19. People described they feeling very tired after only a little bit cognitive, physical, social, and emotional activity. Persistent fatigue is also accompanied by a decrease in physical stamina, leading to increased sleepiness.
Sensitivity and Pain:People with Long COVID may experience new pain or loss of sensitivity to touch. The gain of pain also known as post-COVID pain They also may experience tingling or burning sensations. These changes tend to be worse in the limbs, particularly in the hands, and/or feet. This is because COVID-19 is thought to affect the nerves that send signals like touch, pressure, heat/cold, and pain to the brain.[5]
Headache: Headache is one of the most common neuropsychiatric symptoms patient reported. There are about 44% patients report headache after get infected. [6]
Dizziness and Fainting:After recover from COVID-19, the part of the nervous system that regulates involuntary functions such as blood transportation and blood pressure might not completely recover. This is also known as dysautonomia and can lead to increase heart rate and fainting when standing up from a lying down or sitting position. According NIH, this type of dizziness and fainting also called postural orthostatic tachycardia syndrome (POTS).
Movement issue:
Pathophysiology
Nasal Infections
Breathing Pathway
COVID and the Nervous System
Alzheimer's disease
Parkinson's disease
Treatment and Management
- ↑ Chertow, D., Stein, S., Ramelli, S., Grazioli, A., Chung, J.-Y., Singh, M., Yinda, C.K., Winkler, C., Dickey, J., Ylaya, K., Ko, S.H., Platt, A., Burbelo, P., Quezado, M., Pittaluga, S., Purcell, M., Munster, V., Belinky, F., Ramos-Benitez, M. and Boritz, E. (2021). SARS-CoV-2 infection and persistence throughout the human body and brai. [online] Europe PMC. Available at: https://europepmc.org/article/ppr/ppr434451.
- ↑ covid19.nih.gov. (n.d.). Shining a Light on Long COVID Brain Fog | NIH COVID-19 Research. [online] Available at: https://covid19.nih.gov/news-and-stories/shining-light-long-covid-brain-fog#:~:text=%E2%80%9CBrain%20fog%E2%80%9D%20is%20a%20range.
- ↑ Tony, A.A., Tony, E.AE., Ali, S.B., Ezzeldin, A.M. and Mahmoud, A.A. (2020). COVID-19-associated sleep disorders: A case report. Neurobiology of Sleep and Circadian Rhythms, 9, p.100057. doi:https://doi.org/10.1016/j.nbscr.2020.100057.
- ↑ www.ninds.nih.gov. (n.d.). COVID-19 and the Nervous System | National Institute of Neurological Disorders and Stroke. [online] Available at: https://www.ninds.nih.gov/current-research/coronavirus-and-ninds/covid-19-and-nervous-system#:~:text=Since%20COVID%2D19%20can%20affect.
- ↑ Fernández-de-las-Peñas, C., Herrero-Montes, M., Cancela-Cilleruelo, I., Rodríguez-Jiménez, J., Parás-Bravo, P., Varol, U., del-Valle-Loarte, P., Flox-Benítez, G., Arendt-Nielsen, L. and Valera-Calero, J.A. (2022). Understanding Sensitization, Cognitive and Neuropathic Associated Mechanisms behind Post-COVID Pain: A Network Analysis. Diagnostics, 12(7), p.1538. doi:https://doi.org/10.3390/diagnostics12071538.
- ↑ Lopez-Leon, S., Wegman-Ostrosky, T., Perelman, C., Sepulveda, R., Rebolledo, P.A., Cuapio, A. and Villapol, S. (2021). More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Scientific Reports, [online] 11(1), p.16144. doi:https://doi.org/10.1038/s41598-021-95565-8.