Staphylococcus in United States
Classification
Higher order taxa:
Bacteria; Firmicutes; Bacilli; Bacillales; Staphylococcaceae; Staphylococcus
Species:
Staphylococcus 9IX/A01/138, S. arlettae, S. aureus, S. auricularis, S. capitis, S. caprae, S. carnosus, S. chromogenes, S. cohnii, S. condimenti, S. croceolyticus, S. delphini, S. epidermidis, S. equorum, S. faecalis, S. felis, S. fleurettii, S. gallinarum, S. haemolyticus, S. hominis, S. hyicus, S. intermedius, S. kloosii, S. lentus, S. lugdunensis, S. lutrae, S. lyticans, S. muscae, S. nepalensis, S. pasteuri, S. pettenkoferi, S. piscifermentans, S. pseudintermedius, S. roseus, S. saccharolyticus, S. saprophyticus, S. schleiferi, S. sciuri, S. simiae, S. simulans, S. succinus, S. vitulinus, S. warneri, S. xylosus
Introduction
Staphylococcus is classified as a genus of gram-positive bacteria responsible for a disease known as “Staph.” The disease is commonly observed as skin infections; however it is not limited to other conditions such as food poisoning, bronchopneumonia, and meningitis. The most prevailing form of Staphylococcus is Staphylococcus aureus, which is usually found in the nose and on the skin of most warm-blooded species like humans. A common “Staph” infection on the skin may appear pus-like and red. The infection is likely to seen near wounds, or individuals with weakened immune systems. Through the use of antibiotics (both in humans and in livestock), Staphylococcus aureus has developed resistances to certain drug therapies. For example, Methicillin-resistant Staphylococcus aureus, or MRSA, is resistant to the Penicillin Class of antibiotics. Today, many precautious measures are taking place to prevent the spread of the bacteria, especially resistive ones like MRSA. In addition, there are many effective methods (and also developing ways) to treat the current condition of Staphylococcus.
Description of Staphylococcus
Staphylococcus, more commonly known as Staph, is a type of bacteria that causes various diseases including skin infection, food poisoning, blood poisoning, pneumonia, and even death in rare cases. Although there are more than 30 different types of Staphylococcus, the majority of these diseases is caused by Staphylococcus Aureus. Of all infections caused by these bacteria, skin infections are the most commonly observed (7).
Staphylococcus can be found in the nose and on the skin of approximately 30% of healthy people. Most of the time, this bacteria does not cause any harm to the body. However, in the presence of a skin wound or injury, it becomes more resistant to the body’s natural protective mechanisms, in which case the bacteria will gain the opportunity to cause numerous diseases (8).
Anyone with a weakened immune system is susceptible to developing a Staph infection. Likewise, people who have skin wounds, diabetes, cancer, or are breastfeeding women are also at greater risk of developing an infection. In addition, athletes who come in physical contact with other people or objects that carry this bacteria on the skin or surface are more likely to get infected as well (8).
Staph diseases on the skin are typically easily distinguished because of their distinctive appearance. Boils can develop where the bacteria gains access to the hair follicle beneath the skin. They may appear red, swollen, and painful due to the pus inside. If left untreated, boils can progress to other diseases such as impetigo and cellulitis (8).
Although most skin infections are easily treated with topical, oral, or intravenous antibiotics, strains like MRSA are resistant to many antibiotics used to treat Staph infections, including methicillin, penicillin, amoxicillin, and oxacillin. MRSA is usually transferred via physical contact with the bacteria itself and not through the air. MRSA can also be transferred through indirect contact by touching towels, equipments, or workout areas that have been contaminated by a person infected by MRSA (9).
Description of the microbe
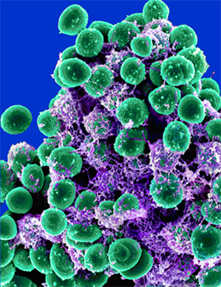
Staphylococcus, the genus name of a specific group of Gram-Positive Bacteria, is characterized by its round “cocci” shape, named after the Greek term for “grape bunches”. This grapelike structure is caused by the two-planar division mechanisms (or branching) of Staphylococcus. The Staphylococcus genus consists of forty-two known species and subspecies, and the most commonly found type is Staphylococcus aureus(3). Staphylococcus is mainly found in mucosal membranes and epidermal tissues. Many exist in the nose and skin of warm-blooded animals like humans. These gram-positive bacteria (thick cell-walled bacteria) are non-sporulating, are immobile (no flagella), and are facultative anaerobes(1) (meaning they do not require oxygen for their metabolism).
Techniques such as Pulsed-field Gel Electrophoresis (PFGE) and Multi-locus Sequence Typing (MLST) are commonly used to study the molecular epidemiology of Staphylococci(4).
Staphylococcus aureus and Staphylococcus epidermis are the two most present and infectious forms of Staphylococcus. Both usually coexist and are present on the skin, nose, mouth, external ear, and urethra of humans. S.epidermis is known to be a “mild-pathogen,” meaning that is does not normally cause infections. Meanwhile, S. aureus, often observed as large round golden-yellow colonies, is known to cause skin pustules, boils and carbuncles. Staphylococcus aureus is also ‘coagulase-positive’, meaning they produce the enzyme, coagulase, which converts fibrinogen to fibrin. When S. aureus comes in contact with blood, it can form a fibrin coat, making it more resistant to phagocytosis. S. aureus uses the host’s blood as a heme source to obtain iron for nutrients, cofactors, or other uses via ABC-type transporters(6). With the right nutrients and thermal conditions, Staphylococcus aureus may grow, spread, and seriously infect its host(2). In addition, S. aureus is commonly the cause for infected wounds, bronchopneumonia, septicemia, acute endocarditis, meningitis, and food poisoning(1). In rare cases, Staphylococcus aureus can also cause necrotizing fasciitis, which is known as deep-tissue flesh-eating bacteria(2).
Since the initial discovery of Staphylococcus, Staphylococcus aureus has branched into many strains, and have developed many forms antibiotic resistant. One particular is known as Methicillin-resistant Staphylococcus aureus or MRSA. This bacterium is difficult to treat due to the resistance to an entire group of antibiotics known as the beta-lactams (consisting of penicillins and cephalosporins)(4). The development and acquisition of resistance genes is mainly transferred through ‘Horizontal Gene Transfer.(5)’ In addition, S. aureus, S. pyogenes and other Staphylococci can synthesize toxins like Pyrogenic toxin superantigens, Exfoliative toxins, and αβδ-toxins. These antigens lead to specific diseases like Toxic Shock Syndrome (TSS), Staphylococcal scalded-skin syndrome (SSSS), and more commonly, food poisoning.
Aside from the more frequently seen species of staphylococcus (S. aureus, S. epidermis), the following are some of the are also commonly studied: Staphylococcus arlettae, S. carnosus, S. cohnii, S. delphini, S. equorum, S. hyicus, S. intermedius, S. kloosii, S. lugdunensis, S. warneri, S. capitis, S. caprae, S. chromogenes, S. gallinarum, S. haemolyticus, S. hominis, S. lentus, S. muscae, S. saprophyticus, S. sciuri, S. simulans, S. xylosus, S. auricularis, S. felis, and S. schleiferi.
Condition of this disease in the United States
The bacteria staphylococcus aureus, was discovered in 1880 in Scotland by surgeon Sir Alexander Ogston. He observed the pus of surgical abscesses. What he saw was a group of “grape-like” clusters of bacteria. Hence he gave the name staphylococcus coming from the Greek word for grapes “staphylia.”(13) Up until the 1940’s a diagnosis of staph infection more likely than not led to death usually by bacterial pneumonia or bacteria in the bloodstream. With the discovery of antibiotics, namely penicillin, this changed. Unfortunately, the overuse and misuse of antibiotics has allowed the bacteria to evolve resistance to many different drugs. By the late 1950’s staphylococcus was almost completely resistant to penicillin. Methicillin was the next progression in fighting the disease. In 1961, the first reports of methicillin were reported. A new form of the staph infection developed, methicillin resistant staphylococcus aureus (MRSA). This is a strain that is resistant to an entire beta-lactam class of drugs.(11) The gram-positve bacteria continues to evolve. Vancomycin-resistance has been reported since as early as 2002.
In 2005, the CDC conducted a survey of percentage of infections that occurred in health care setting, hospital and community-based. The incidence of non-hospital infections seems to be on the rise. It was found that hospital infections were similar strains to the community-based infections. The move of staph infections out of the hospital and into the community, demonstrates the mutation rate and severity of staphylococcus.(10) Recent research by a team of doctors at the National Institute of Allergy and Infectious Diseases (NIAID), have found that the genetic factors the influence drug resistance and virulence are transferred in one horizontal gene transfer. When combined with research in 2007, that stated the staphylococci secreted a toxin, phenol-soluble modulin, which attacked neutrophils, it may be possible to develop new methods in which to fight staph infections. By knowing where these genes are, there is a possibility to turn them off instead of killing the bacteria completely. (13) The fear of a super-bug is ever present in many healthcare settings.
This newly developed resistance is a problem, especially in hospitals, because of the lack of antibiotics which can combat it. It has become prevalent in nursing homes, adapted to hospital life, and been a stepping stone to the next scare of MRSA, the EMRSA or epidemic MRSA. MRSA is called EMRSA when MRSA spread internationally or if MRSA isolates thrive successfully throughout hospitals within a country. Following the evolutionary progression of S.aureus, the EMRSA clones are increasingly becoming resistant to glycopeptide targeted antibiotics, especially with the increased use of vancomycin. [21]
In the United States, one strain has been brought to attention due to its strong virulence and is found to be the culprit of the community-associated MRSA (CA-MRSA) epidemic . The infectious strain, USA300 like, its progenitor, USA 500, is thought to be extremely virulent amongst animals. Both strains also have the ability to evade host immune defenses. USA 300 and USA 500’s is thought to have “differential expression of core genome-encoded virulence determinants, such as phenol-soluble modulins and α-toxin”, contributing to their high virulence. The fact that differential expression plays a key role in USA300’s virulence , and not mobile genetic elements as once hypothesized, brings scientists a step closer to successfully combating these S.aureus strains. [22]
In the past, cases of infection from S.aureus were found prevalently in hospitals. After the introduction of community-associated MRSA, there are now many cases spread amongst the community, and within the past decade, many cases found associated with livestock such as pigs and poultry. [23,24] It is now believed that there is a connection between livestock colonization and MRSA infections in humans who associate closely with animals. In the Netherlands, studies have been conducted in pig farmers and pigs, revealing the increasing presence of MRSA sequence type (ST) 398. [23]The prevalence of this strain of MRSA has been found to be greater than 20 percent in pig farmers and 39 percent in pigs found in slaughterhouses. The MRSA epidemic has spread internationally, with cases also found in Canada, Singapore, and other European countries. [25] In addition to pig related infection cases, there is also evidence of S. aureus growing resistance to numerous antimicrobials in poultry within the past forty years. [24] Furthermore, the growing number of these infection and MRSA carrier cases in livestock and people who work with animals raises concern that there may be infection risk dealing with domesticated animals.
Current Methods of Treatment
Staphylococcus Aureus, like most other infections, can be contained in two ways—treatment and prevention; more specifically, the treatment of those presently affected and the prevention of future spread. There are currently five popular methods of treatment for Staphylococcus in the United States.
Appropriate antibiotics are currently the most effective and common way to treat those infected(16). These antibiotics are delivered to the patient in a variety of ways, usually in an ointment form, but also orally or intravenously if more serious(15). However, the type of antibiotic given to the patient is dependent on the vulnerability and resistance of that specific Staphylococcal strain. For instance, Methycillin-Resistant Staphylococcus Aureus (MRSA) is an example of a Staphylococcal strain that has developed a resistance to the penicillin-family of antibiotics. Patients infected by MRSA are treated by a different antibiotics like Vancomycin(14).
There are a few other methods currently used to treat those infected with s. Aureus, usually in cases in which antibiotics are ineffective or dangerous. Sometimes the strain triggers a buildup of pus in various parts of the body; therefore, some doctors drain these pus collections as an alternative method for treatment. Two other methods involve the actual removal of dead tissue and foreign bodies (stitches) that may be a focus of persisting infection. Surgery eliminates these infected areas and the possibility of further proliferation by the Staphylococcus. The last method is less common and specific to those with a skin disease that might encourage Staphylococcus attack. Rather than treat the bacterial infection, doctors focus their treatment on the root of the problem, the underlying skin disease (e.g. atopic eczema)(16). All these treatments, however effective, have not fully eliminated the chance of infection. This is due to the resistance that bacteria develop in relatively short periods of time to many antibiotics.
Methods of prevention
Staphylococcus is a very common bacteria, found on the skin and in the nasal passages of most people. When an opportunity arises, such as a compromised immune system or a break in the epidermis, Staphylococcus Aureus can cause infection. Although several treatments are available for Staph, as it is commonly referred to, the best method of treatment is to avoid infections altogether via preventative measures. Since most Staph infections are easily treated with antibiotics, the real concern is MRSA (methicillin-resistant Staphylococcus aureus), since it has developed resistance to the entire family of penicillin antibiotics.
Prevention of Staph, and in particular MRSA, is an area of ongoing study. Valle et. al. confirmed that “colonization represents a high risk factor for MRSA” via their study in hospitals of the correlation between positive MRSA nasal swabs and rate of infection (17). Thus, prevention of colonization is one approach to prevention – if the bacteria is unable to colonize, it will be unable to infect. Also, securing access to open wounds and ensuring infected patients are isolated and decontaminated can help prevent MRSA spread. A reduction in MRSA cases has been seen in US hospitals due to greater infection control (of contaminated individuals), improved management of intravenous lines (a common MRSA infection entry point), and mupirocin-based decontamination treatments used to decolonize patients (18). However, to strategically apply preventative measures where they are needed most, proper reporting by health facilities to a central database is necessary. As surveillance and reporting increase, the number of MRSA cases was found to decrease (19), since high-risk areas and locations were able to apply more preventative measures to stop its spread before treatment was needed for actual infection. The more complicated methods of prevention discussed above go hand-in-hand with common sense practices such as washing hands with soap and warm water frequently, wearing protective gear when contacting contaminated or infected patients, thoroughly sterilizing high-risk or infected environments, etc.
Also worth noting are future possibilities of prevention. Several new drugs have been or are being developed specifically to treat MRSA infection, including the development of 11- and 13-valent vaccines (18). Since MRSA works partially by secretion of Pyrogenic toxin, some drug development is focusing on knocking out that gene from ever being expressed, which may reduce or remove MRSA's resistance to some antibiotics. Even natural oils such as PRE (pomegranate rind extract) have shown promise – PRE, in combination with Cu(II) ions, was shown to “exhibit moderate antimicrobial effects against clinical isolates of MRSA,” indicating that natural oils with antimicrobial properties may also hold promise for future MRSA preventative techniques (20).
Photographs (click on photo for more information)
References
(1) http://www.medicinenet.com/staph_infection/article.htm
(2) http://www.nlm.nih.gov/medlineplus/staphylococcalinfections.html#cat45
(3) http://gsbs.utmb.edu/microbook/ch012.htm
(4) "Staphylococcus." Encyclopædia Britannica. 2009. Encyclopædia Britannica Online <http://www.britannica.com/EBchecked/topic/563360/staphylococcus>
(5) "Staphylococcus," Microsoft® Encarta® Online Encyclopedia 2009 <http://encarta.msn.com/encyclopedia_761555010/Staphylococcus.html>
(6) “Genetic Classification and Distinguishing of Staphylococcus Species Based on Different Partial gap, 16S rRNA, hsp60, rpoB, sodA, and tuf Gene Sequences” B. Ghebremedhin,*† F. Layer,† W. König, and B. König <http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2268370&tool=pmcentrez>
(7) “The evolution of Staphylococcus aureus” Deurenberg RH, Stobberingh EE, 2008 Dec <http://www.ncbi.nlm.nih.gov/pubmed/18718557>
(8) “Genetics of antimicrobial resistance in Staphylococcus aureus” Jensen SO, Lyon BR 2009 Jun, <http://www.ncbi.nlm.nih.gov/pubmed/19492967>
(9) “Intracellular metalloporphyrin metabolism in Staphylococcus aureus” Reniere ML, Torres VJ, Skaar EP, <http://www.ncbi.nlm.nih.gov/pubmed/17387580>
(10) Stoppler, Melissa C. "Staph Infection (Staphylococcus aureus)." Medicine Net. Ed. William C. Shiel. 20 Aug. 2009.
(11) "Community-Associated MRSA Information for the Public." Center for Disease Control and Prevention. 30 June 2008. Division of Healthcare Quality Promotion (DHQP). 20 Aug. 2009.
(12) Stanway, Amy. "Staphylococcal Skin Infections." DermNet NZ. Department of Dermatology, Health Waikato, Private Bag 3200, Hamilton, New Zealand., 15 June 2009. Web. 22 Aug. 2009.
(13) JAMA and Archives Journals. "Drug-resistant Staph Infection Appears More Widespread Than Previously Thought." ScienceDaily 17 October 2007. 24 August 2009 <http://www.sciencedaily.com /releases/2007/10/071016160644.htm>.
(14) "Methicillin-Resistant Staphylococcus aureus (MRSA): History." Antimicrobial Resistance. National Institute of Allergy and Infectious Diseases, 5 Mar. 2008. Web. 24 Aug. 2009. <http://www3.niaid.nih.gov/topics/antimicrobialResistance/Examples/mrsa/history.htm>.
(15) NIH/National Institute of Allergy and Infectious Diseases. "Genes Key To Staph Disease Severity, Drug Resistance Found Hitchhiking Together." ScienceDaily 2 August 2009. 24 August 2009 <http://www.sciencedaily.com /releases/2009/07/090731132921.htm>.
(16) Ogston A (1984). "“On Abscesses”. Classics in Infectious Diseases". Rev Infect Dis 6 (1): 122–28. PMID 6369479.
(17) Valle, Claudia D. et. al. "Control of MRSA infection and colonization in an intensive care unit by GeneOhm MRSA assay and culture methods" BMC Infectious Diseases 24 August 2009. <http://www.biomedcentral.com/1471-2334/9/137>
(18) Livermore, David M. “Has the era of untreatable infections arrived?” Journal of Antimicrobial Chemotherapy September 2009. 24 August 2009 <http://jac.oxfordjournals.org/cgi/content/full/64/suppl_1/i29>.
(19) Pearson, Andrew; Chronias, Andrew; Murray, Miranda “Voluntary and mandatory surveillance for methicillin-resistant Staphylococcus aureus (MRSA) and methicillin-susceptible S. aureus (MSSA) bacteraemia” Journal of Antimicrobial Chemotherapy September 2009. 24 August 2009 <http://jac.oxfordjournals.org/cgi/content/full/64/suppl_1/i11>
(20) Pearson, Andrew; Chronias, Andrew; Murray, Miranda “Voluntary and mandatory surveillance for methicillin-resistant Staphylococcus aureus (MRSA) and methicillin-susceptible S. aureus (MSSA) bacteraemia” Journal of Antimicrobial Chemotherapy September 2009. 24 August 2009 <http://jac.oxfordjournals.org/cgi/content/full/64/suppl_1/i11>
(21) Mark C. Enright, D. Ashley Robinson, Gaynor Randle, Edward J. Feil, Hajo Grundmann, and Brian G. Spratt. (2002) The evolutionary history of methicillin-resistant Staphylococcus aureus (MRSA). PNAS May 28, 2002 vol. 99 no. 11 7687-7692. <http://www.pnas.org/content/99/11/7687.full.pdf+html?sid=48f46a67-2939-49ef-b48e-c2ef0a86509f>
(22) Min Li, Binh An Diep, Amer E. Villaruz, Kevin R. Braughton, Xiaofei Jiang, Frank R. DeLeo, Henry F. Chambers, Yuan Lu, and Michael Otto. (2009) Evolution of virulence in epidemic community-associated methicillin-resistant Staphylococcus aureus. PNAS April 7, 2009 vol. 106 no. 14 5883-5888. <http://www.pnas.org/content/106/14/5883.abstract?sid=d4b1a6a2-8639-4046-a61b-d902c8784f8f>
(23) Burkhard Springer, Ulrike Orendi, Peter Much, Gerda Höger, Werner Ruppitsch, Karina Krziwanek, Sigrid Metz-Gercek and Helmut Mittermayer. (2009) Methicillin-resistant Staphylococcus aureus : a new zoonotic agent? Wiener Klinische Wochenschrift February, 2009 Volume 121, Numbers 3-4. <http://www.springerlink.com/content/1557180k4715t847/>
(24) Mostafa Nemati, Katleen Hermans, Urszula Lipinska, Olivier Denis, Ariane Deplano, Marc Struelens, Luc A. Devriese, Frank Pasmans, and Freddy Haesebrouck. (2008) Antimicrobial Resistance of Old and Recent Staphylococcus aureus Isolates from Poultry: First Detection of Livestock-Associated Methicillin-Resistant Strain ST398. Antimicrobial Agents and Chemotherapy, October 2008, p. 3817-3819, Vol. 52, No. 10 0066-4804. <http://aac.asm.org/cgi/content/full/52/10/3817?view=long&pmid=18663024>
(25) M. Wulf, A. Voss. (2008) MRSA in livestock animals; an epidemic waiting to happen? Clinical Microbiology and Infection. Volume 14, Issue 6 , Pages519 – 521. <http://www.ncbi.nlm.nih.gov/pubmed/18325034?ordinalpos=21&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_DefaultReportPanel.Pubmed_RVDocSum>
Edited by Justin Gibson, Stephen Ly, Anish Dhamija, Naho Fukushima,
Anthony Koutoufidis, and Veronica Cheung, students of Rachel Larsen