Aggregatibacter actinomycetemcomitans
Classification
Kingdom: Bacteria
Phylum: Proteobacteria
Class: Gammaproteobacteria
Order: Pasteurellales
Family: Pasteurellaceae
Genus: Aggregatibacter
Species: Actinomycetemcomitans
Species
NCBI: HK1651 Taxonomy
Aggregatibacter Actinomycetemcomitans
Description and Significance
Description
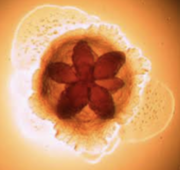
In 1975, scientists Killian and Schiott were the first to demonstrate that Aggregatibacter actinomycetemcomitans was present in dental plaque and from that point on, more and more important discoveries about A. actinomycetemcomitans have been made. Aggregatibacter actinomycetemcomitans are nonmotile, gram-negative bacteria capable of growing under both aerobic and anaerobic conditions. They also thrive in high concentrations of carbon dioxide. What’s really interesting about this bacterium is its shape. You can see it has an internal star-shape and translucent colonies. Aggregatibacter actinomycetemcomitans has three main features including fimbriae, vesicles and extracellular amorphous materials. Fimbriae of A. actinomycetemcomitans are small, filamentous cell surface appendages. They are uniformly distributed in bundles and don’t measure more than two micrometers in diameter. A. actinomycetemcomitans can either have star-positive fimbriated colonies or have a non-fimbriated strain. Non-fimbriated A. actinomycetemcomitans are smooth, leading to poor adherence and poor biofilm forming capacity. The most abundant fimbriae protein is 304-a, a thin protein with a low molecular weight. These fimbriae provide the attachment factor, allowing adhesion. Vesicles, otherwise known as blebs, of A. actinomycetemcomitans are lipopolysaccharide in nature, which is common for a great majority of gram-negative bacteria. Highly leukotoxic strains of A. actinomycetemcomitans tend to have more vesicles. These leukotoxins are described as virulence factors that kill leukocytes allowing them to escape from the host immune system. They play a critical role in the survival of A. actinomycetemcomitans and periodontal disease progression. A. actinomycetemcomitans vesicles also contain endotoxin, which is critical in the role of A. actinomycetemcomitans. Endotoxin basically links cytokine stimulation and proinflammatory reactions, leading to the decay of dental pulp and periodontal disease. Vesicles also contain a bacteriocin named actinobacillus which is known for adhering to and colonizing the human oral cavity, leading to aggressive periodontitis. Furthermore, these vesicles also exhibit adhesive properties and function to deliver toxic materials. Finally, the extracellular amorphous material exhibits bone-resorbing activity and adhesive properties as well.
Significance
A. actinomycetemcomitans inhabits the mouths of one-third or more of the population.
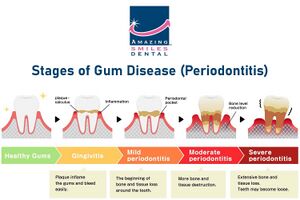
It is most commonly known as a systemic pathogen, causing the rapid progression of localized aggressive periodontal disease, otherwise known as LAP. As a matter of fact, A. actinomycetemcomitans is present in approximately 90% of patients with LAP. LAP is significant because, as opposed to general periodontitis, it specifically impacts the central incisors (which are your top two teeth and bottom two teeth) and first molars. It is common for LAP patients to have tooth loss and breakdown of supporting tooth structures when this disease is left untreated. Another risk is through blood circulation, there is the risk of swelling of the endocardium, the innermost tissue lining the heart. This actually makes a lot of sense because A. actinomycetemcomitans thrives in environments of periodontal pockets and blood circulation. This shines light on the importance of maintaining proper oral hygiene because of the significant correlation between oral and cardiovascular health. Referring to the general population, approximately 70,000 adolescents in the United States develop periodontitis disease annually. And individuals of African-American descent have a 10 to 15 fold greater risk of developing periodontal disease than Caucasian Americans.
Genome Structure
The genome size of Aggregatibacter actinomycetemcomitans, a bacterium, ranges from 2.0 to 2.7 Mb, which is tiny in comparison to other bacteria. Its single circular chromosome, which houses 2,206 genes, is what defines its genomic structure. These genes include 2,129 coding sequences that are involved in several biological processes, as well as 19 rRNAs and 54 tRNAs that are in charge of protein synthesis. In addition, 4 noncoding RNAs found in the genome may have regulatory functions in the bacteria. According to whole genome sequencing (WGS) research, A. actinomycetemcomitans can be categorized into three evolutionary lineages (I, II, and III) based on variations in its genomic makeup and transformation competence. Serotyping, which has been the standard method of classification, has also been demonstrated to be ineffective for fully describing the species because some serotypes are not exclusive to particular lineages. A. actinomycetemcomitans demonstrates variation in capacity for transformation in addition to genetic diversity; different lineages display different levels of natural competence. This ability to transform is associated with horizontal gene transfer and may have an effect on the amount of a strain's genome within the species. Additionally, previous taxonomy classifications of A. actinomycetemcomitans based only on serotyping have been questioned by WGS investigations.
Cell Structure, Metabolism and Life Cycle
Cell Structure and Metabolism
A clinically relevant bacterium linked to periodontal disease, Aggregatibacter actinomycetemcomitans, has a unique cell structure and metabolism. A.actinomycetemcomitans is a facultatively anaerobic, Gram-negative rod with particular traits. Its cells may appear as cocci under a microscope in clinical samples and broth, suggesting pleomorphism. This bacterium exhibits environmental flexibility despite not being motile and lacking flagella; it grows well in 5% CO2 but poorly in ambient air. On chocolate agar, colonies are tiny, rough-textured, and tenacious, sticking to the agar surfaces with great vigor. A. actinomycetemcomitans is also unique in that it can create a number of different enzymes and toxins, such as leukotoxin and cytolethal distending toxin, which add to its pathogenicity in periodontal infections. A. actinomycetemcomitans is also distinguished at the molecular level by its outer membrane, which encloses an inner cytoplasmic membrane and a thin coating of peptidoglycan. The dimensions of its rod-shaped cell normally range from 0.4 to 0.5 µm in width and 1.0 to 1.5 µm in length. Although this bacteria lacks mobility, its rough texture helps it stick to surfaces, which increases colonization and pathogenicity. A. actinomycetemcomitans can produce a variety of toxins that are essential to its pathogenicity through metabolism, which can lead to tissue damage and immune evasion in the host.
Life Cycle
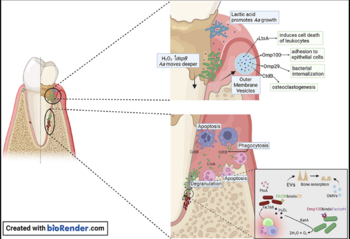
The bacterium colonizes the oral mucosa early in life and is inherited by vertical transmission from close relatives. There is a prevalence and gingival localization of Aggregatibacter actinomycetemcomitans in periodontal lesions of young patients along with intra-tissue bacterial cells and phagocytic cells, which had invaded gingival connective tissue. A. actinomycetemcomitans utilizes metabolic products from other inhabitants of the biofilm for survival and growth. This bacterium also makes use of lactic acid produced by Streptococcus pyogenes as a nutrient to increase its numbers. More recent studies have demonstrated invasion of A. actinomycetemcomitans into epithelial cells. Outer membrane protein OmpA1 is associated with the entry of A. actinomycetemcomitans into gingival epithelial cells caused by the up-regulating F-actin rearrangement via the FAK signaling pathway. Another outer membrane protein, Omp100 promotes adhesion of A. actinomycetemcomitans, and their invasion of gingival epithelial cells. These outer membrane proteins contribute to pathogenicity which will be discussed later on. Streptococcus pyogenes produce Hydrogen peroxide, protecting A. actinomycetemcomitans from oxidative damage and allowing it to migrate deeper into the gingival pocket where they are exposed to th host immune response. The image on the top right shows the invasion of A. actinomycetemcomitans into epithelial cells. A. actinomycetemcomitans is now protected from mechanical removal, antibiotics, immune cell phagocytosis, and antibody building. A. actinomycetemcomitans has developed mechanisms to survive in human serum‐rich environments in vivo, including resistance to complement‐mediated cell lysis and phagocytosis regardless of serotypes and leukotoxin production.
These features allow it to survive in hostile environments of periodontal pockets and blood circulation, where human serum is the predominant nutrient source for bacterial metabolism. Human serum is basically blood plasma without clotting factors. In the presence of human serum, bacteriophages are induced to undergo a transition from a lysogenic prophage into the lytic cycle, resulting in bacterial lysis. The pyruvate dehydrogenase complex oxidatively decarboxylates pyruvate to acetyl-coA for the TCA cycle. The TCA cycle, otherwise known as cyclic acid cycle, provides large amounts of energy in aerobic conditions. This energy production and delivery system is required for the replication of phage progeny. Under the PDHc catalytic reaction, bacterial lysis occurs and regulates this bacterium.
Ecology and Pathogenesis
Aggregatibacter actinomycetemcomitans, a Gram-negative bacterium found in the oral microbiota, plays a significant role in human disease due to its aggregative nature and pathogenic potential. While initially cultured from non-oral infections, its involvement in periodontitis has gained recognition, highlighting its dual capacity to cause both oral and systemic diseases. A. actinomycetemcomitans can be isolated from various oral and non-oral infectious diseases, including infective endocarditis, arthritis, bacteraemia, osteomyelitis, skin infections, urinary tract infections, and abscesses. Its pathogenicity in infective endocarditis is particularly notable, with the bacterium being a member of the HACEK group associated with a small but significant percentage of cases. In the context of periodontitis, A. actinomycetemcomitans contributes to the dysbiotic changes within the periodontal microbiota, leading to inflammatory destruction of connective tissue and bone around teeth. The bacterium's ability to evade host immune responses and interact with other microbial species in the oral cavity underscores its complex role in disease pathogenesis.
Furthermore, A. actinomycetemcomitans is associated with specific virulence factors, notably leukotoxin, which is implicated in localized aggressive periodontitis and can induce apoptosis in epithelial cells, contributing to tissue damage. Additionally, the bacterium produces cytolethal distending toxin (CDT), which disrupts the cell cycle in host cells, leading to DNA damage. Clinical symptoms associated with A. actinomycetemcomitans infections include gingival inflammation, periodontal pocket formation, bone loss, and tooth mobility. The complexity of interactions between A. actinomycetemcomitans, other microbial species, and the host immune system underscores the multifaceted nature of its ecology and pathogenesis, highlighting the need for comprehensive approaches to understanding and managing diseases associated with this bacterium.
Reference
1) Belibasakis, G. N., Maula, T., Bao, K., Lindholm, M., Bostanci, N., Oscarsson, J., Ihalin, R., & Johansson, A.(2019). Virulence and Pathogenicity Properties of Aggregatibacter actinomycetemcomitans. Pathogens (Basel,
- Switzerland), 8(4), 222.
2) Flemmig, T. F. (1999). Periodontitis. Annals of periodontology, 4(1), 32-37.
3) Kelk, P., Abd, H., Claesson, R., SandstrÃm, G., SjÃstedt, A., & Johansson, A. (2011). Cellular and molecular response of human macrophages exposed to
- Aggregatibacter actinomycetemcomitans leukotoxin. Cell Death & Disease, 2(3), e126–e126.
4) Lindholm, M., Min Aung, K., Nyunt Wai, S., & Oscarsson, J. (2019). Role of OmpA1 and OmpA2 in Aggregatibacter actinomycetemcomitans and Aggregatibacter
- aphrophilus serum resistance. Journal of Oral Microbiology, 11(1), 1536192.
5) May, A. C., Ehrlich, R. L., Balashov, S., Ehrlich, G. D., Shanmugam, M., Fine, D. H., ... & Cugini, C. (2016).Complete genome sequence of Aggregatibacter
- actinomycetemcomitans strain IDH781. Genome Announcements, 4(6), 10-1128.
6) Nedergaard, S., Kobel, C. M., Nielsen, M. B., Møller, R. T., Jensen, A. B., & Nørskov-Lauritsen, N. (2019).
- Whole Genome Sequencing of Aggregatibacter actinomycetemcomitans Cultured from Blood Stream Infections Reveals Three Major Phylogenetic Groups Including a
- Novel Lineage Expressing Serotype a Membrane O Polysaccharide. Pathogens, 8(4), 256.
7) Nørskov-Lauritsen, N., Claesson, R., Jensen, A. B., Åberg, C. H., & Haubek, D. (2019). Aggregatibacter Actinomycetemcomitans: Clinical Significance of a
- Pathobiont Subjected to Ample Changes in Classification and Nomenclature. Pathogens, 8(4).
8) Oscarsson, J., Claesson, R., Lindholm, M., Höglund Åberg, C., & Johansson, A. (2019). Tools of Aggregatibacter actinomycetemcomitans to evade the host response. :: Journal of clinical medicine, 8(7), 1079.
9) Ozuna, H., Snider, I., Belibasakis, G. N., Oscarsson, J., Johansson, A., & Uriarte, S. M. (2022). Aggregatibacter actinomycetemcomitans and Filifactor alocis Two exotoxin-producing oral pathogens. Frontiers in oral health,
- 3, 981343.
10) Raja, M., Ummer, F., & Dhivakar, C. P. (2014). Aggregatibacter actinomycetemcomitans–a tooth killer?. Journal of clinical and diagnostic research: JCDR, 8(8), ZE13.
11) Sampathkumar, V., Velusamy, S. K., Godboley, D., & Fine, D. H. (2017). Increased leukotoxin production: Characterization of 100 base pairs within the 530 base pair leukotoxin promoter region of Aggregatibacter
- actinomycetemcomitans. Scientific reports, 7(1), 1887.
12) Tang-Siegel, G. G. (2023). Human Serum Mediated Bacteriophage Life Cycle Switch in Aggregatibacter actinomycetemcomitans Is Linked to Pyruvate Dehydrogenase
- Complex. Life, 13(2), 436.
13) Tsai, C. C., Ho, Y. P., Chou, Y. S., Ho, K. Y., Wu, Y. M., & Lin, Y. C. (2018). Aggregatibacter (Actinobacillus) actimycetemcomitans leukotoxin and human
- periodontitis–A historic review with emphasis on JP2. The Kaohsiung journal of medical sciences, 34(4), 186-193.
14) Vega, B. A., Belinka Jr, B. A., & Kachlany, S. C. (2019). Aggregatibacter actinomycetemcomitans leukotoxin (LtxA; Leukothera®): mechanisms of action and
- therapeutic applications. Toxins, 11(9), 489.
15) Yoshida, A., Bouziane, A., Erraji, S., Lakhdar, L., Rhissassi, M., Miyazaki, H., ... & Ennibi, O. (2021). Etiology of aggressive periodontitis in individuals of African descent. Japanese Dental Science Review, 57, 20-26.
Authors
Page authored by Hannah Pedersen and Nirali Patel, students of Professor Jay Lennon at Indiana University.