Antibiotic Resistance Within Staphylococcus Aureus: Difference between revisions
No edit summary |
No edit summary |
||
| Line 8: | Line 8: | ||
[[File:MRSA SEM 9994 lores.jpg|MRSA SEM 9994]] | [[File:MRSA SEM 9994 lores.jpg|MRSA SEM 9994]] | ||
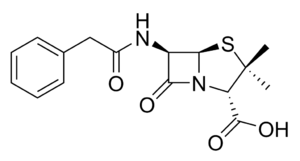
[http://commons.wikimedia.org/wiki/File:MRSA_SEM_9994_lores.jpg Figure 1.] 20000x magnified image of methicillin resistant <i>S. aureus</i> bacteria under high magnification [http://commons.wikimedia.org/wiki/File:MRSA_SEM_9994_lores.jpg] | |||
The bacteria was first discovered by Alexander Ogston in 1880 when he became interested in the high post surgery mortality rates, and was later named by Friedrich Julius Rosenbach. More commonly referred to as a “staph infection” or “staph bacteria”, <i>S. aureus</i> is reportedly found in 30% of the population who are asymptomatic nasal carriers, while another large portion carry the bacteria on their skin.[http://www.nejm.org/doi/full/10.1056/NEJM199808203390806] <i>S. aureus</i> is transferred through skin to skin contact and more commonly affects persons previously diseased or with weaker immune systems. The most common transfer happens from a health worker who has been in contact with an active strain of it. Other transfers occur from environmental sources or from other carriers of the bacteria. Possible outcomes from staph infections include many hospital originated issues including pneumonia and bloodstream and wound infections. When <i>S. aureus</i> was first identified, and before antibiotics were developed, the bacteria had a mortality rate of 80%. Today, with antibiotic treatment, the mortality rates around the world range from 20-40% [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC154455/]. | The bacteria was first discovered by Alexander Ogston in 1880 when he became interested in the high post surgery mortality rates, and was later named by Friedrich Julius Rosenbach. More commonly referred to as a “staph infection” or “staph bacteria”, <i>S. aureus</i> is reportedly found in 30% of the population who are asymptomatic nasal carriers, while another large portion carry the bacteria on their skin.[http://www.nejm.org/doi/full/10.1056/NEJM199808203390806] <i>S. aureus</i> is transferred through skin to skin contact and more commonly affects persons previously diseased or with weaker immune systems. The most common transfer happens from a health worker who has been in contact with an active strain of it. Other transfers occur from environmental sources or from other carriers of the bacteria. Possible outcomes from staph infections include many hospital originated issues including pneumonia and bloodstream and wound infections. When <i>S. aureus</i> was first identified, and before antibiotics were developed, the bacteria had a mortality rate of 80%. Today, with antibiotic treatment, the mortality rates around the world range from 20-40% [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC154455/]. | ||
Revision as of 17:37, 24 March 2015
Staphylococcus aureus is a growing issue both within hospitals and communities because of its ability to adjust to different environments. Over the years, S. aureus has become resistant to many different antibiotics including penicillin and methicillin. Today, Staphylococcus aureus remains a growing pandemic because of its increasing antibiotic resistance through different mechanisms including horizontal gene transfer and altering of antibiotics. It continues to cause serious and sometimes life threatening infections.
Introduction
Staphylococcus aureus is a gram positive bacteria that belongs to the micrococcaceae family and appears in the form of cocci clusters. It differs from other staphylococcus because it appears with gold pigmentation. The bacteria also tests positive for coagulase, mannitol-fermentation, and deoxyribonuclease. Staphylococcus aureus has a thick cell wall made up of peptidoglycan and in this case are 50 percent by weight. The peptidoglycan are made up of both N-acetylglucosamine and N-acetylmuramic acid, which are linked with tetrapeptide chains, found only in S. aureus. It contains prophages, plasmids, and transposons all within a 2800 bp circular chromosome [1]. This is where mechanisms of antibiotic resistance are found.
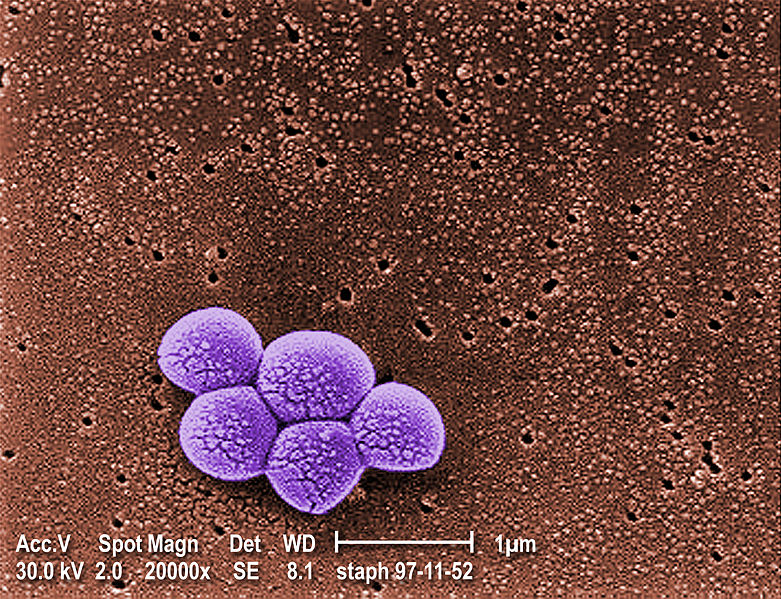
Figure 1. 20000x magnified image of methicillin resistant S. aureus bacteria under high magnification [2]
The bacteria was first discovered by Alexander Ogston in 1880 when he became interested in the high post surgery mortality rates, and was later named by Friedrich Julius Rosenbach. More commonly referred to as a “staph infection” or “staph bacteria”, S. aureus is reportedly found in 30% of the population who are asymptomatic nasal carriers, while another large portion carry the bacteria on their skin.[3] S. aureus is transferred through skin to skin contact and more commonly affects persons previously diseased or with weaker immune systems. The most common transfer happens from a health worker who has been in contact with an active strain of it. Other transfers occur from environmental sources or from other carriers of the bacteria. Possible outcomes from staph infections include many hospital originated issues including pneumonia and bloodstream and wound infections. When S. aureus was first identified, and before antibiotics were developed, the bacteria had a mortality rate of 80%. Today, with antibiotic treatment, the mortality rates around the world range from 20-40% [4].
Penicillin Resistance: History and Mechanisms
The first antibiotic introduced to fight S. aureus was penicillin in 1940, which decreased mortality rates significantly. Two years later, resistance to the drug was already being recognized both within communities and hospitals. More than 80% of staphylococcus strains were found to be resistant by the early 1960’s [5]. These strains were found by Bondi and Dietz in 1948 to contain penicillinase, which is a specific type of β-lactamase [6]. β-lactam antibiotics, like penicillin, work by inhibiting the cell enzyme which in this case would be β-lactamase. Inhibiting the cell enzyme slows down cell wall formation which brings down osmotic pressure and eventually kills the cell. β-lactam antibiotics are able to inhibit enzymes with a β-lactam ring, which binds to the enzyme in the bacteria cell.
One way in which bacteria become resistant to antibiotics is by hydrolyzing the β-lactam ring (shown in Fig. 2). They do this when they contain a blaZ gene, which codes for penicillinase. The gene reorganizes the enzyme and does not allow for it to bind with β-lactam ring. BlaZ gene is located on a transposable part of the large plasmid within the S. aureus bacteria cells. Because of this location, the gene is easily movable to surrounding cells through horizontal gene transfer.
Methicillin: History and Resistance
In 1961, methicillin was introduced as an attempt to combat pencillin resistant staphylococcus aureus strains. In less than a year, some S. aureus were reported to be methicillin resistant. Beginning in hospitals in the 1970s, and slowly moving out to the community, methicillin resistant S. aureus (MRSA) became a growing issue. Similar to penicillin, methicillin works by inhibiting the synthesis of cell wall through stoppage of peptidoglycan formation. Peptidoglycan for S. aureus is externally by penicillin binding proteins. These proteins both cross link and extend the peptidoglycan chain that form the cell wall.Methicillin works by inhibiting these proteins, thus stopping cell wall formation and making the cell weak and eventually die. Over time, S. aureus has built resistance to this type of antibiotic. This is attributed to the mecA gene, which is actually transferred from different bacteria and can be traced back to Staphylococcus sciuri [7]. When the gene is present, penicillin binding proteins are still produced, but their structure make it harder for β-lactam rings within the antibiotics to bind and stop cell wall formation. This mechanism is similar to that of penicillin and the blaZ gene.
Further Reading
References
Edited by (Liza Ach), a student of Nora Sullivan in BIOL168L (Microbiology) in The Keck Science Department of the Claremont Colleges Spring 2014.