Antibiotic Use for Farm Animals: Difference between revisions
(Created page with "{{Curated}} [[Image:naturally-yours-antibiotics-animals.jpg|thumb|500px|right|Cow being injected with antibiotic. [[http://thebigceci.files.wordpress.com/2012/01/naturally-yours-...") |
|||
| Line 32: | Line 32: | ||
There are three main ways antibiotic resistant bacteria get from farms to humans. | There are three main ways antibiotic resistant bacteria get from farms to humans. | ||
[[Image: | [[Image:antibiotics-for-agriculture/uploads/2012/04/antibiotics-for-agriculture.jpg|thumb|500px|left|Route of Antibiotic from Farm Animals to Humans | ||
[[http://momentscount.com/wp-content/uploads/2012/04/antibiotics-for-agriculture.gif]]]]<p></p> | [[http://momentscount.com/wp-content/uploads/2012/04/antibiotics-for-agriculture.gif]]]]<p></p> | ||
Revision as of 00:54, 8 May 2012

Antibiotic Use for Farm Animals
Overview
Usage of antibiotics in farm animals is quite heavy and widespread, and has been a typical practice of farmers in North America and Europe for quite some time. Most beef, pork, poultry consumed by humans contains small amounts of antibiotics. This is a result of attempts to increase quality and quantity of output on farms. The United States uses over 29 million pounds of antibiotics in livestock per year. The majority of drugs are fed to animals to promote their growth in factory farms. A factory farm is characteristic of U.S. livestock production and consists of keeping animals in high-density confinement. Consistently using drugs in farm animals raises concerns that this administering of antibiotics has caused an increase in the antibiotic-resistant bacteria that can be harmful to humans. Antibiotic resistant infections cost the US over 16 million dollars per year. Bacteria in the human microbiome can learn how to resist more drugs because humans are exposed to slight amounts of antibiotics in the meats that they eat. Antibiotics are used in animals and can help bacteria become resistant to the same or similar drugs used in humans. Antibiotics are naturally occurring, semi-synthetic and synthetic compounds of antimicrobial activity are used in human and veterinary medicine to treat and prevent disease, and for other purposes including growth promotion in food animals. Bacteria can spread via animals, which are turned into food, which are eaten by humans and can then cause human infection. This is a reason behind using antibiotics in farm animals, in addition to growth promotion. Antibiotic resistance occurs when “survival of the fittest” occurs with bacteria populations. When antibiotics do somehow not kill bacteria, these cells can multiply and pass on the genetic material that can resist drugs on to more bacteria. Thus, greater exposure to antibiotics, especially unnecessarily, will beget more resistance. Concern over antibiotic use in farm animals relates to the disadvantages to human and animal health that result from potential overexposure. The threat of antibiotic resistance is real, but some argue that the actual danger seems small: some question the quantified harm this process begets (drug companies, for instance, that have an economic stake in this issue). Growth promotion via antibiotics requires only small dosages. Some antibiotics are used both in animals and in humans but most of the resistance problems are from human use. While antibiotic use in farm animals is contributing to the problem of resistance, over prescription in humans is certainly a large factor as well.
Uses of Antibiotics for Farm Animals
A startling 80% of all antibiotics sold in the United States are used for farm animals. While some of that 80% is used to treat animal illnesses, the majority (90%) is administered through the animals’ water or feed to assist the animals’ growth and subsequent weight gain and to also preventively help the livestock survive the harsh farm and living conditions through antibiotic treatment. Farm animals ingested 29.1 million pounds of antibiotics in 2010, a 400,000-pound increase from 2009. Antibiotics are primarily administered in two different agricultural contexts: Therapy and Growth Promotion.
Therapy
Therapy is the administration of antibiotics to animals or groups of animals in order to treat animal illness. When farm animals exhibit clinical diseases a common method of treatment is the use of appropriate antibiotics. Veterinary medical advances made it possible to locate, treat, and prevent catastrophic animal health risks that could be detrimental to the agriculture sector as a whole. For many farm animal diseases and illness prove to be readily amenable to antibiotic immunizations. At the first signs of animal distress, the owner or farmer will refer the case to animal physician, veterinarian, who will then discern the course of antibiotic treatment, is necessary. The main objective in employing antibiotic therapy treatment in farm animals is to limit the progression of disease in a population of animals. Also the therapy use of antibiotics is meant to treat the specific animal’s illness because disease negatively impacts and decreases farm animals’ performance and abilities. The principal goal of the antibiotic agents, in a therapy situation, is to treat the animals’ infections and destroy the harm causing pathogens as quickly as possible while also causing minimal adverse effects to the animal in question. In doing so the specific antibiotic will bind to the target site, or active site, of the organism to attack the disease causing pathogens. Therapeutic applications of antibiotics in farm animals are essential components to increase profitable and humane livestock production in response to broad economic pressure of consumer demand for protein. Therapeutic uses of antibiotics must be under the advice and discretion of a practicing animal physician. Farmers, ranchers, and farm animal owners alike all must consult the advice of a veterinarian prior to the employment of antibiotic treatment to sick animals. Similarly, the full course of antibiotic treatment for farm animals requires a valid prescription and the oversight of a veterinarian. This being said, malpractice and misuse of antibiotics on farm animals, i.e. using therapeutic antibiotics to treat disease in farm animals without a prescription or without a veterinarian’s opinion, inevitably does occur. In addition, farmers, ranchers, and animal owners must only use antibiotics approved by the U.S. Food and Drug Administration, which monitors antibiotic use for farm animals to ensure not only the effectiveness in treatment but also safety for the animals and their meat and milk products. As stated in the American Dairy Association and Dairy Council’s review in 2003, “All milk is strictly tested for antibiotics on the farm and at the processing plant. Any milk that tests positive [for antibiotics] cannot be sold to the public” ensuring both meat and milk are rigorously monitored for the presence of antibiotics. Overall, therapeutic antibiotic use in animal agriculture results in healthier animals, which in turn provides for healthier sources of food for humans. Therefore, in terms of antibiotic use for farm animals, the health promotion benefits should be highlighted despite the controversial effects of antibiotic use for animal growth promotion.
Growth Promotion
The other major source of antibiotic use for farm animals is the employment of antibiotics for animal growth promotion. Growth promotion refers to the administration of antibiotics to farm animals, usually as an animal feed additive, over a period of time to growing animals that results in improved physiological performance. Many antimicrobials have been found to dramatically improve the average daily weight gain of farm animals and also the feed efficiency of livestock in addition to other results deemed beneficial to farm animal owners. While the actual net benefit of using antibiotic feed for farm animals is difficult to measure, it is significant enough to the farmer’s profit that this method is commonly used. Growth-promoting effects of antibiotic use for farm animals are often mediated through alterations of the normal intestinal microbial population of the animal, which results in more efficient digestion of animal feed and metabolic uptake of nutrients. In addition, the low dosage of antibiotics used for growth promotion in farm animals is also effective and proven to suppress some infectious diseases. Therefore, other effects of the use of antibiotics for farm animals in a growth-promotion context are mediated through the immune system. In this regard, the regulation and suppression of infections and diseases in farm animals is an important effect of growth promoter antibiotic use in farm animals. Though, this seemingly unorthodox use of antibiotics for farm animals to promote their growth is highly controversial in terms of its safety not only for the animals but also for the people who consume these animals’ products. The question of increased antibiotic resistant in humans, due to antibiotic use in animals, is contested.
Human Implications
The use of antibiotics in livestock results in a major cause for concern about the potential transfer of resistance from animal to human microbes.
How Bacteria in Farm Animals Develop Resistance
Antibiotics are widely used in medicine to treat and prevent human infection. The rising use of antibiotics in livestock production (for the two main purposes outlined above) leads the animals’ microbes to be overexposed to these drugs. This leaves the animals’ intestinal tracts or other body sites colonized by microbes that have adapted and built up resistance to the antibiotics. Achieving resistance requires some kind of change in the bacterial DNA – either through spontaneous mutation or acquiring a new piece of DNA, typically a plasmid. Bacteria typically develop resistance through the following three ways:
1. Changing the intracellular target. This occurs through spontaneous random mutation of the DNA in such a way that the cell alters the protein that the drug is designed to target. 2. Pumping out the antibiotic. This occurs because the bacteria has acquired new DNA “instructions” that allow it to force the antibiotic to leave the cell. 3. Altering the antibiotic to a harmless form. This also occurs through the bacterial acquisition of new DNA “instructions” that allow it to change it to an innocuous form.
How Resistance is Transferred to Human Microbes
There are three main ways antibiotic resistant bacteria get from farms to humans.
Food Products
Resistant bacteria remain in livestock and farm animal products during slaughter and processing and then are passed along to humans who consume these products. Common examples of such organisms are salmonella and e. coli. Research on antibiotic resistant strains has proven that the food chain is the main means of transmission.
Environment
Bacteria are spread by manure on farmland, contaminating runoff and water. This contributes to the small amount of antibiotics that were found in soil samples and in 48% of the country’s streams as well as the traces of resistant bacteria that were found in shellfish.
Direct Transfer to Farmers
This occurs primarily when enteroccoci, for example, are directly transferred from animals to the farmers who work with them.
Concerns
The transfer of resistant bacteria from farm animals to humans poses a health threat because many of the antibiotics given to livestock, such as fluoroquinolones and cephalosporins) are the same drugs used to cure human afflictions like urinary tract infections and pneumonia. Over time, as bacteria in livestock have been increasingly exposed to antibiotics such as penicillin or tetracycline, more resistance has built up. When healthy human guts are colonized by resistant bacteria it makes antibiotics less effective for human medicine. 100,000 Americans die yearly due to bacterial infections contracted in hospitals that are resistant to most antibiotics. In addition to being a public health concern, antibacterial resistance is also extremely costly. It costs $16-26 billion in medical expenses annually and $35 billion for lost time from work.
Avoparcin
Avoparcin, a gram-positive antibiotic used for growth promotion in livestock in Europe, is linked to the recent occurrence of vancomycin-resistant enterococci in livestock, demonstrating that resistance can spread from animals to humans. Avoparcin was used as an antimicrobial growth promoter (for livestock) and later became known as the antibiotic vancoymycin, which is used to treat multi-resistant hospital-acquired infections. This is particularly concerning because this class of antibiotics are used to treat infections that are resistant to many commonly-used drugs so when they become resistant to vancomycin the infections become virtually untreatable. Avoparcin was never allowed for use on livestock in USA and Canada but was allowed in EU and then later banned. The elimination of using avoparcin caused a reduction in levels of resistance in animals, food, and thus humans.
Other Sources of Resistant Bacteria
While the recent increase in bacterial resistance of human microbes has been proven, the cause of this resistance is debated. Many argue that the probability for humans to contract resistant bacteria from livestock products is low because the traces of resistant bacteria in such products is already low and then many would be killed off by the high temperatures during cooking. Additionally, many point to other factors as the source of these resistant bacteria. For example, humans are blamed for introducing pathogens and resistant strains to the environment via sewage, vegetable fertilizers, or careless measures that allow wild animals to acquire them and pass them on through their excretions to the grazing land of farm animals. The excess use of antibiotics in medical practices has also been pointed to as a contributor to bacterial resistance, yet there have not been many attempts to limit this as such efforts are though to be ineffective without reducing antibiotic farm use.
History
The use of antibiotics on livestock dates back to the late 1940’s when farmers first found they promoted growth in poultry. Ever since, farmers have increased the amount and types of antibiotics used on livestock in order to increase output and profits. The FDA has passed legislature to curb some of the use, however most conclude that these futile attempts have proved ineffective. In 1943, Selman Waksman found a revolutionary new antibiotic, “streptomycin.” This drug went on to become incredibly useful for human because it was effective on far more diseases than the previously found, penicillin. In fact, Waksman had been attempting to find drugs for livestock, not humans. And streptomycin proved to be an industry-changing discovery. It prompted more farmers and researchers to test antibiotics on animals to prevent sickness, but a popular side product emerged, the animals grew quicker and larger. Therefore the use of antibiotics on livestock increased immensely.
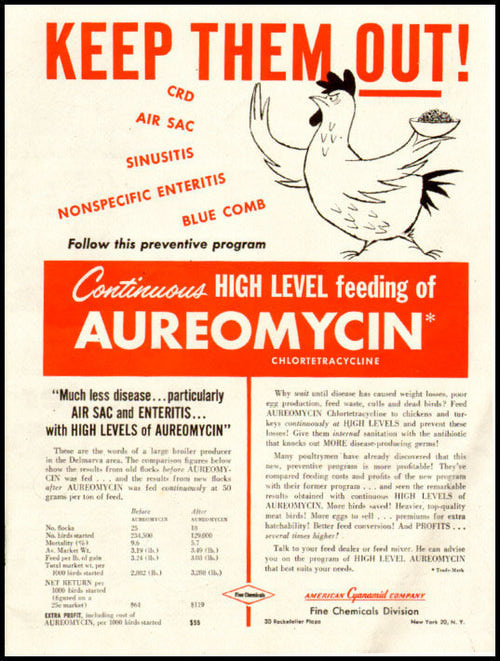
In 1951, the Food and Drug Administration (FDA) approved, for the first time, the use of the antibiotics, penicillin and chlortetracycline, as animal feed additives. Only two years later, another, oxytetracycline, was approved by the FDA for use. They were promoted as “peaceful” weapons against illnesses, and hailed by farmers and the FDA alike. In due time however, researchers revealed that there may be issues with heavily used antibiotics on livestock. In 1969, the UK government found that there could be a potential risk to humans from the use in animals and that the overuse of antibiotics in livestock was increasing the amount of drug-resistant bacteria. Just three years later, the FDA concludes that the use of antibiotics is causing resistant bacteria and requires manufacturers to show the effectiveness and safety of the drugs. A monumental study by Tufts University’s Stuart Levy found that farmers who had fed chickens the antibiotic, tetracycline, had resistant bacteria present in them. His study resulted in the frightening conclusion that the increase in resistance of bacteria was due to the use of antibiotics. Although this study could have prompted major changes within the world of antibiotics and farming, the National Academy of Sciences, which was appointed by the FDA to conduct research on the issue, found that there was not sufficient evidence to prove this fact. Later in the eighties there were two more studies done which concluded that the increase in resistant-bacteria was due to antibiotic use and that these bacteria could flow from chickens to humans through consumption, however there was no action taken. It is important to note that this research and evidence was available up to thirty years ago. However, the FDA continued to deflect the findings and ignore the potential danger. There was substantial pressure from farmers’ advocates and Congress to the FDA to disregard the negative aspects, because of the incredible upside for production and profit.
New FDA Regulations
Antibiotics were continually used on livestock for the next thirty years, even though there were multiple studies revealing major negative effects to humans and an increase in resistant-bacteria. It was not until January 1, 2006, that the EU finally took action against the overuse of antibiotics on livestock by banning the use of antibiotics on livestock for the purpose of growth promotion. This was a major decision and established a precedent for limiting antibiotic use on livestock. However, it took over six years for the FDA to impose any ban on similar use of antibiotics. On January 4, 2012, the FDA prohibited the use of one type of antibiotic, cephalosporin, in animal feed, unless it is to treat disease. Considering that this type of antibiotic makes up only about .3% of the overall use, the ban did not have an overwhelming effect. It may have prompted to the FDA to begin imposing more serious regulations though. On April 11, 2012, the FDA began to seriously regulate the use of antibiotics on livestock, by mandating a prescription for them and prohibiting the phrase “growth promotion” from the use of any antibiotic. This latest action is incredibly recent and so it is difficult to tell whether or not the legislature has been effective. In addition, the FDA proposed to limit the use of antibiotics by farmers in an effort to phase out the use of antibiotics as a growth tool. However, the FDA is looking for more voluntary limitation by the farmers and drug companies. This is a step in the right direction and this recent change in mindset by the FDA will hopefully decrease the rate at which bacteria are becoming resistant to antibiotics.
Conclusion
The two main uses of antibiotics in livestock is to fight bacterial infections and to promote growth. Both of these aim to produce a healthier stock of animals. Because humans eat the majority of these animals, we are exposed to traces of the different antibiotics that the livestock consume. This has lead to the growth of resistant bacteria in humans. Because of concerns over increasing antibiotic resistance, there have been some moves to contain usage. Since 1970’s the FDA has known about misuse of antibiotics in agriculture yet little has been done until recently. Starting in 1970, a task force from the Food and Drug Administration in the US recommended that some human antibiotics should not be used in animals. From this point on, more information has become available about the usage and affects of antibiotics in farm animals and how it affects humans. While the European Union banned antibiotic use for growth production in 2006, the FDA did not do the same until early 2012. Antibiotic resistance is likely to diminish or lessen in prevalence and strength when antibiotic use is decreased or continued. Many of the antibiotics given to animals are of the same class as those used to treat human infections. While some people debate the argument that antibiotic use in livestock production is the only cause of human antibiotic resistance, it is certainly proven to be a main cause.
References
1. “FDA Bails on Animal Antibiotics Hearings.” Photo Credit Naturally Yours Blog. Last modified January 20, 2012.<http://thebigceci.wordpress.com/tag/animal-antibiotics/>.
2. “FDA Ordered to Examine Antibiotic Use on Farm Animals.” Photo Credit Moments Count from the ASPCA Blog.<http://momentscount.com/archives/10066>.
3. J. Antimicrob. Chemother. “Does the use of antibiotics in food animals pose a risk to human health? A critical review of published data.” Journal of Antimicrobial Chemotherapy. (2004) 53 (1): 28-52.
4. Wegener, Henrik. "Antibiotics in animal feed and their role in resistance development." Current Opinion in Microbiology. 6. no. 5 (2003): 439-45.
5. Walsh, Bryan. Time Magazine, "Environmental Groups Sue the FDA Over Antibiotics and Meat Production Read more: http://ecocentric.blogs.time.Environmental groups sue the FDA over antibiotics and meat production." Last modified May 25, 2011.
6. Editors. Bloomberg, "Cows, Pigs, Chickens Have Drug Problem Congress Can Fix." Last modified Apr 23, 2012. Accessed May 7, 2012. http://www.bloomberg.com/news/2012-04-23/cows-pigs-chickens-have-drug-problem-congress-can-fix-view.html.
7. Wenderoff, Josh. The Pew Charitable Trusts, "Pew Applauds FDA Measure to Preserve Effectiveness of Critical Antibiotics." Last modified January 4, 2012. http://www.saveantibiotics.org/newsroom/pr_04Jan2012.html.
8. "FDA call on antibiotics could increase consumer confidence, but hurt producers” DairyBusiness http://dairybusiness.com/seo/headline.php?title=fda-call-on-antibiotics-could-increase-consum&date=2012-04-18&table=headlines (accessed May 7, 2012).
9. Walsh, Bryan. "Toward a Drug-Free Burger: Ruling May Curb Antibiotics in Meat - TIME." TImeScience. http://www.time.com/time/health/article/0,8599,2110227,00.html (accessed May 7, 2012).
10. Tomson, Bill. "FDA Tries to Curb Antibiotic Use in Farm Animals - WSJ.com." Wall Street Journal. http://online.wsj.com/article/SB10001424052702304444604577338063592731138.html (accessed May 7, 2012).
11. Hurd, SH, S Doores, D Hayes, Am Mathew, J Maurer, P Silley, SS Randall, and RN Jones. "Public Health Consequences of Macrolide Use in Food Animals: A Deterministic Risk Assessment." Journal of Food Protection 67, no. 5 (2004): 980-992.
12. Groeger, Lena. "A History of FDA Inaction on Animal Antibiotics - ProPublica." ProPublica. http://www.propublica.org/special/a-history-of-fda-inaction-on-animal-antibiotics (accessed May 7, 2012).
13. "A history of antibiotic use in farm animals - CBS News." CBS News. http://www.cbsnews.com/8301-505245_162-57418135/a-history-of-antibiotic-use-in-farm-animals/ (accessed May 7, 2012).
Edited by Gillian Hannon, Alexandra Frosina, Becka Levin, and Matthew Egan, students of Rachel Larsen
