Clostridium perfringens Bacteria and Food Illness: Difference between revisions
| Line 30: | Line 30: | ||
==Clostridium perfringens Toxin== | ==Clostridium perfringens Toxin== | ||
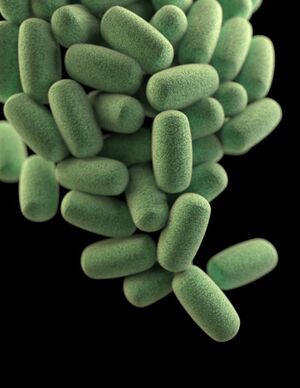
[[Image:nihms617524f1.jpeg|thumb|300px|left|Fig. 1. | [[Image:nihms617524f1.jpeg|thumb|300px|left|Fig. 1. <I>Clostridium perfringens</i> toxins. CPA: C. perfringens alpha toxin (1CA1); CPE: C. perfringens enterotoxin (3AM2); Delta: Delta toxin (2YGT); ETX: C. perfringens epsilon toxin (1UYJ); ITXa: C. perfringens iota toxin a subunit (1GIR); NetB: Necrotic enteritis toxin B (4ION); PFO: Perfringolysin O (1PFO). This figure was created by Uzal et al. (2014)<ref name=b/>]] | ||
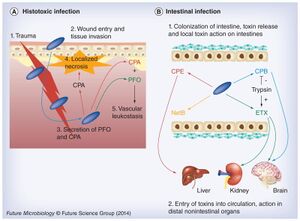
[[Image:Nihms617524f9.jpeg|thumb|300px|left|Fig. 2. A schematic that summaries toxin involvement under <I>Clostridium perfringens</I> infection. (A) During histotoxic infections CPA plays a predominant role after | [[Image:Nihms617524f9.jpeg|thumb|300px|left|Fig. 2. A schematic that summaries toxin involvement under <I>Clostridium perfringens</I> infection. (A) During histotoxic infections CPA plays a predominant role after pathogen (blue rods) is introduced by trauma into muscle tissue. This toxin induces localized necrosis, as well as toxemic effects in other organs when toxins enter the circulation. Both CPA and PFO are important in vascular leukostasis. (B) During intestinal infections, <I>C. perfringens</I> (blue rods) is able to produce several pore-forming toxins, including CPE during sporulation or (during vegetative growth) NetB, ETX or CPB. Host intestinal protease levels can either destroy (e.g., CPB) or activate (e.g., ETX) these toxins. When present in an active form, these toxins can cause local damage (necrosis) or be absorbed into the circulation to damage internal organs such as the brain, kidney or liver. | ||
CPA: C. perfringens alpha toxin; CPB: C. perfringens beta toxin; CPE: C. perfringens enterotoxin; PFO: Perfringolysin O.. This figure was created by Uzal et al. (2014)<ref name=b/>]] | CPA: C. perfringens alpha toxin; CPB: C. perfringens beta toxin; CPE: C. perfringens enterotoxin; PFO: Perfringolysin O.. This figure was created by Uzal et al. (2014)<ref name=b/>]] | ||
Most bacterial infections are caused by potent toxic proteins. The many diseases occur as a result of the bacterium’s toxins it produces, many of which are extracellular (Rood et al. 2018). There are >16 toxins that can cause histotoxic and intestinal infections, and it is unclear as to why there are so many different kinds when many have the same target: host cell plasma membranes<ref name=b/>. Each toxin is produced depending on the type of <i>C. perfringens</i> and there are 5 types: A, B, C, D, and E<ref name=b/>.In figure 1, the structure of different types of <i>C. perfringens</i> toxins are shown.<br> | Most bacterial infections are caused by potent toxic proteins. The many diseases occur as a result of the bacterium’s toxins it produces, many of which are extracellular (Rood et al. 2018). There are >16 toxins that can cause histotoxic and intestinal infections, and it is unclear as to why there are so many different kinds when many have the same target: host cell plasma membranes<ref name=b/>. Each toxin is produced depending on the type of <i>C. perfringens</i> and there are 5 types: A, B, C, D, and E<ref name=b/>.In figure 1, the structure of different types of <i>C. perfringens</i> toxins are shown.<br> | ||
<br>Histotoxic clostridial infection is a type of pathogenesis that involves the growth of <i>Clostridium</i> in the tissues and extensive tissue destruction, which is a result done by the extracellular toxins. Histotoxic infection includes gas gangrene or myonecrosis. It has been established that <i>C. perfringens</i> uses chromosomally encoded alpha toxin (alpha-phospholipase C) and perfringolysin O (a pore-forming toxin) in histotoxic (poisonous to tissue) infections <ref name=b/>. On the other hand, intestinal disease occurs by employing toxins encoded by mobile genetic elements, including <i>C. perfringens</i> enterotoxin, necrotic enteritis toxin B-like, epsilon toxin and beta toxin<ref name=b/>.<br> | <br>Histotoxic clostridial infection is a type of pathogenesis that involves the growth of <i>Clostridium</i> in the tissues and extensive tissue destruction, which is a result done by the extracellular toxins. Histotoxic infection includes gas gangrene or myonecrosis. It has been established that <i>C. perfringens</i> uses chromosomally encoded alpha toxin (alpha-phospholipase C) and perfringolysin O (a pore-forming toxin) in histotoxic (poisonous to tissue) infections <ref name=b/>. On the other hand, intestinal disease occurs by employing toxins encoded by mobile genetic elements, including <i>C. perfringens</i> enterotoxin, necrotic enteritis toxin B-like, epsilon toxin and beta toxin<ref name=b/>.<br> | ||
<br>After testing to see the effects specific toxins have on the intestinal walls, some toxins (CPA and PFO) are specifically used for histotoxic infection (fig. 2. A). During histotoxic infection, these toxins are able to interfere with the host’s immune response which causes localized necrosis to facilitate the growth of the pathogen. In addition, the toxins allow for host cells leakage and lysis which further benefits pathogen growth by providing nutrients<ref name=b/>. This combination leads to cell death and eventually the death of the host, killed cells only improve <i>C. perfringens</i> multiplication. | |||
==Drug Resistance== | ==Drug Resistance== | ||
Revision as of 02:10, 19 April 2022
By Paula Cancelas Calvo
Introduction
Food-borne illness occurs when one consumes contaminated foods or beverages. This type of illness has been around humans for as long as we have been humans, and the same pathogens not only affects humans but also animals. In humans, "The Centers for Disease Control and Prevention (CDC) estimate that 76 million foodborne illnesses, including 325,000 hospitalizations and 5,000 deaths, occur in the United States each year" [1]. There are many different types of pathogens that can cause food-borne illness, some less serious than others, nevertheless, they are still serious. Many of these bacteria can lead to serious gastrointestinal complications. Clostridium perfringens is one of those bacteria that is known for food related illness. This gram-positive, nonmotile, anaerobic spore producing bacteria is one of the most common and important human and animal pathogens that can cause an array of diseases [2]. In addition, this pathogen is among the most widespread bacteria, with a ubiquitous environmental distribution in soil, sewage, food, fecal, and in normal intestinal gut microbiota of both humans and animals[2].
In regards to food related illness, Clostridium perfringens is one of the most common causes and the CDC estimates that 1 million illnesses are caused by these food poisoning bacteria[3].. Symptoms associated with consumption of contaminated foods are most often diarrhea and stomach cramps and usually appear 6 to 24 hours after consumption of contaminated food, and this is not transmissible directly from one person to another[3]. This type of food poisoning leaves you in pain and dehydrated. In most, antibiotics are not necessary for treatment and as long as fluids are restored there should be no problems. Although these symptoms are considered to be short and temporary, as mentioned before, C. perfringens can lead to serious gastrointestinal infections such as traumatic gas gangrene, necrotic enteritis of both human and neonatal animal species, enterotoxemia of sheep and goats, and among others, all which can lead to death if left untreated[2]. Not only that, but in agricultural circumstances, it can decimate farm output which can affect a country’s economy and consumers if a serious outbreak were to occur. “According to the United States Department of Agriculture (USDA), foodborne illness costs the US economy $10-83 billion per year”[1].
The reason why C. perfringens infections are of concern is because of how common the bacterium is and how it is the major cause of food-borne illness. The toxins that the bacteria produces are believed to be what damages the host, however, there are many different kinds and it unclear why so many kinds are produced. In addition, with the overprescription and improper disposal of antibiotic medication, through mobile genetic elements or horizontal gene transfer, drug resistance is becoming more prevalent in all sorts of bacterial species including C. perfringens. This antibiotic resistance also affects the gut microbiome in both animals and humans. All of these pose as concern as food-borne illness is a major public health threat, and to better understand the major cause of said illness will improve treatment and prevention methods.
Double brackets: [[
Filename: PHIL_1181_lores.jpg
Thumbnail status: |thumb|
Pixel size: |300px|
Placement on page: |right|
Legend/credit: Electron micrograph of the Ebola Zaire virus. This was the first photo ever taken of the virus, on 10/13/1976. By Dr. F.A. Murphy, now at U.C. Davis, then at the CDC. Every image requires a link to the source.
Closed double brackets: ]]
Other examples:
Bold
Italic
Subscript: H2O
Superscript: Fe3+
Sample citations: [4]
A citation code consists of a hyperlinked reference within "ref" begin and end codes.
To repeat the citation for other statements, the reference needs to have a names: "<ref name=aa>"
The repeated citation works like this, with a forward slash.[4]
Clostridium perfringens Toxin

Most bacterial infections are caused by potent toxic proteins. The many diseases occur as a result of the bacterium’s toxins it produces, many of which are extracellular (Rood et al. 2018). There are >16 toxins that can cause histotoxic and intestinal infections, and it is unclear as to why there are so many different kinds when many have the same target: host cell plasma membranes[2]. Each toxin is produced depending on the type of C. perfringens and there are 5 types: A, B, C, D, and E[2].In figure 1, the structure of different types of C. perfringens toxins are shown.
Histotoxic clostridial infection is a type of pathogenesis that involves the growth of Clostridium in the tissues and extensive tissue destruction, which is a result done by the extracellular toxins. Histotoxic infection includes gas gangrene or myonecrosis. It has been established that C. perfringens uses chromosomally encoded alpha toxin (alpha-phospholipase C) and perfringolysin O (a pore-forming toxin) in histotoxic (poisonous to tissue) infections [2]. On the other hand, intestinal disease occurs by employing toxins encoded by mobile genetic elements, including C. perfringens enterotoxin, necrotic enteritis toxin B-like, epsilon toxin and beta toxin[2].
After testing to see the effects specific toxins have on the intestinal walls, some toxins (CPA and PFO) are specifically used for histotoxic infection (fig. 2. A). During histotoxic infection, these toxins are able to interfere with the host’s immune response which causes localized necrosis to facilitate the growth of the pathogen. In addition, the toxins allow for host cells leakage and lysis which further benefits pathogen growth by providing nutrients[2]. This combination leads to cell death and eventually the death of the host, killed cells only improve C. perfringens multiplication.
Drug Resistance
Include some current research, with at least one figure showing data.
biofilms...
The Gut Microbiota
Include some current research, with at least one figure showing data.
Prevention
Conclusion
References
- ↑ 1.0 1.1 Nyachuba, D. G. 2010. Foodborne illness: is it on the rise?: Nutrition Reviews©, Vol. 68, No. 5. Nutrition Reviews 68:257–269.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Uzal, F. A., J. C. Freedman, A. Shrestha, J. R. Theoret, J. Garcia, M. M. Awad, V. Adams, R. J. Moore, J. I. Rood, and B. A. McClane. 2014. Towards an understanding of the role of Clostridium perfringens toxins in human and animal disease. Future Microbiology 9:361–377.
- ↑ 3.0 3.1 CDC, Prevent Illness From C. perfringens
- ↑ 4.0 4.1 Hodgkin, J. and Partridge, F.A. "Caenorhabditis elegans meets microsporidia: the nematode killers from Paris." 2008. PLoS Biology 6:2634-2637.
Authored for BIOL 238 Microbiology, taught by Joan Slonczewski, 2022, Kenyon College
