Diagnosis and Prevention of Neisseria meningitides Induced Meningitis: Difference between revisions
| Line 22: | Line 22: | ||
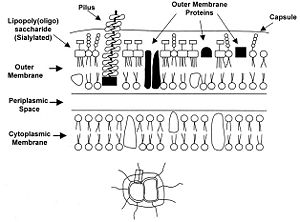
<br>Certain genetic and membranous features of N. meningitidis are vital to understanding and classifying strains of the bacteria. Outer membrane proteins, for example, are particularly important because they provide specific substrates for vaccines and medicines to target.<br> | <br>Certain genetic and membranous features of N. meningitidis are vital to understanding and classifying strains of the bacteria. Outer membrane proteins, for example, are particularly important because they provide specific substrates for vaccines and medicines to target.<br> | ||
<br>The main manner in which N. meningitidis is classified is by serogroup. A serogroup is defined by the presence of specific capsular polysaccharides. N. meningitidis strains have been classified into twelve different serogroups, however only five of the twelve are known to cause meningitis (Taha). The serogroups of the virulent strains are group A, B, C, Y and W-135. Vaccines exist against all of these serogroups except for serogroup B since its capsular polysaccharides are poorly immunogenic (Cripps).<br> | <br>The main manner in which N. meningitidis is classified is by serogroup. A serogroup is defined by the presence of specific capsular polysaccharides. N. meningitidis strains have been classified into twelve different serogroups, however only five of the twelve are known to cause meningitis (Taha). The serogroups of the virulent strains are group A, B, C, Y and W-135. Vaccines exist against all of these serogroups except for serogroup B since its capsular polysaccharides are poorly immunogenic (Cripps). Each serogroup causes a unique type of infection. For example, serogroup A tends to result in epidemic meningitis infections while serogroup B is typically behind endemic ones (Taha).<br> | ||
[[Image:Membrane.JPG|thumb|300px|right|]] | [[Image:Membrane.JPG|thumb|300px|right|]] | ||
Revision as of 22:34, 15 April 2009
By Emily Staudenmaier
Introduction
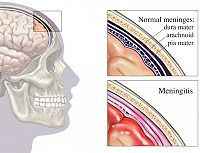
Meningitis is an inflammation of the membrane surrounding the human brain and spinal cord also known as the meninges. Meningitis can be caused by a bacterial or viral infection. Of the two types of infections, bacterial causation generally results in a more severe infection. The inflammation of the meninges results in headache, neck stiffness, fever, sensitivity to light and sometimes vomiting (Slonczewski). These symptoms can progress quickly when bacteria are behind the infection, resulting in death 10-20% of the time (Tzeng). Three species of bacteria, Streptococcus pneumonia, Haemophilus influenzae and Neisseria meningitidis, are known to cause this infection. Certain characteristics of the latter species, N. meningitidis, result in difficult obstacles when it comes to the development of measures to diagnose, treat and prevent meningitis. Those obstacles and promising solutions are discussed in detail below.
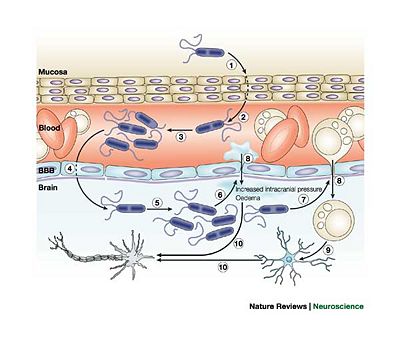
Neisseria meningitidis is Gram-negative, aerobic, nonmotile, coccal bacteria which is pathogenic only to Homo sapiens. Initial infection occurs in the nasopharynx where the bacteria can bind easily to the mucus membrane using their type IV pilli. These bacteria also have a capsid which is minimized during attachment to epithelial cells and then maximized to protect the organism agains the host's immune response. When present in the nasopharynx, the bacteria typically do not cause serious health problems to the host. In fact, 5-10% of adults have N. meningitidis present in their nasopharynx and do not develop meningitis. The asymptomatic presence of the bacteria can be beneficial to the human host since it allows antibodies to develop that can be useful in fighting a more serious subsequent infection. The entrance of the bacteria into the bloodstream results in serious consequences for the host. N. meningitidis has the unusual ability to cross the blood-brain barrier and enter the cerebral spinal fluid (Tzeng). The mechanism of this infiltration is unknown. Once the crossing has occurred, the bacteria release inflammatory cytokines which leads to the inflammation of the meninges.
Infection is spread through direct contact with nasal or oral fluids contaminated with the bacteria. Inhalation of large droplet nuclei can also result in the spread of N. meningitidis. N. meningitidis induced infections are most common and most serious in children, young adults and the elderly. Children who have lost antibodies from their mother and have yet to gain exposure to asymptomatic infections of the bacteria in their nasopharynx, lack any antibiotic immune response to the presence of N. meningitidis (Sánchez). Young children are therefore the most susceptible age group to contracting meningitis. Many vaccines and medications normally prescribed to fight an N. meningitidis infection are not recommended for children younger than two which further complicates the issue of preventing and curing infection in this age group. Infection rate increases again for the young adult age group due simply to an increased level of exposure and transmission especially on college campuses where people live closely in relatively small spaces. The infection rate is also high in the elderly population. Often the elderly possess weakened immune systems which cause them to be more prone to infection.
N. meningitidis is also unique in that it can cause both epidemic and endemic cases of meningitis. Epidemic outbreaks of meningitis have become a serious issue in developing nations where the supply of vaccines and medication is limited and confined living situations result in increased transmission of virulent strains of the bacteria. One region of Africa has been termed the “Meningitis Belt”. The infection rate in this area can be as high as 1000 cases for every 100,000 people in the population (Tzeng).
Due to the highly infectious nature of virulent N. meningitidis and the quick escalation of the severity meningitis infections, timely diagnostic measures and effective vaccines are essential.
Important Features of N. meningitidis
Certain genetic and membranous features of N. meningitidis are vital to understanding and classifying strains of the bacteria. Outer membrane proteins, for example, are particularly important because they provide specific substrates for vaccines and medicines to target.
The main manner in which N. meningitidis is classified is by serogroup. A serogroup is defined by the presence of specific capsular polysaccharides. N. meningitidis strains have been classified into twelve different serogroups, however only five of the twelve are known to cause meningitis (Taha). The serogroups of the virulent strains are group A, B, C, Y and W-135. Vaccines exist against all of these serogroups except for serogroup B since its capsular polysaccharides are poorly immunogenic (Cripps). Each serogroup causes a unique type of infection. For example, serogroup A tends to result in epidemic meningitis infections while serogroup B is typically behind endemic ones (Taha).
As far as genomes go, N. meningitidis has a fairly small one compared to other microorganisms such as E. coli. Their genome is approximately 2, 200 kb long and is particularly susceptible to mutation events due to multiple repetitive sequences and polymorphic sequences (Tzeng). During DNA replication, the replication machinery can slip on particularly long repetitive sequences which results in daughter DNA having either a larger or shorter number of repeats increasing variability in the next generation. Despite the fact that repetitive sequences are a prominent feature of N. meningitidis’ genome, the mutation rate is not particularly high (approximately 10-3 mutations per bacterial cell per generation), and no error-prone repair system exists which also decreases the occurrence and frequency of mutation (Taha). The majority of strain diversity is introduced by recombination.
N. meningitidis also has the interesting attribute of being naturally competent making it easy for the organism to acquire genetic information from other N. meningitidis cells. Competence has allowed for the rapid development of anti-biotic resistant strains which has created a serious barrier to treatment of meningitis. Strains resistant to penicillin, sulfa antibiotics and chloramphenicol have recently been discovered, which is particularly discouraging news since penicillin was a primary method of treatment, especially in epidemic outbreaks of meningitis (Tzeng). The competence of these organisms also allows them the frustrating ability to switch serogroups even during the course of an epidemic (Taha). Since vaccines are targeted to specific serogroups and certain treatments are more effective for some serogroups rather than others, the ability to switch which capsular polysaccharides are expressed makes treatment and prevention difficult. Therefore vaccines protecting against more than one serogroup have been developed but this still leaves the issue of antibiotic resistance.
Detection and Diagnostic Techniques
Include some current research in each topic, with at least one figure showing data.
Vaccination Strategies
Include some current research in each topic, with at least one figure showing data.
Conclusion
Overall paper length should be 3,000 words, with at least 3 figures.
References
Cripps, A., Foxwell, R., and Kyd, J., “Challenges for the development of vaccines against Haemophilus influenzae and Neisseria meningitides”. Current Opinion in Immunology. 2002. Volume 14. p. 553-557
Lansac, N., Picard, F. J., Ménard, C., Boissinot, M., Ouellette, M., Roy, P. H., and Bergeron, M. G. “Novel Genus-Specific PCR-Based Assays for Rapid Identification of Neisseria Species and Neisseria meningitidis”. European Journal of Clinical Microbiology and Infectious Diseases. 2000. Volume 19. p. 443-451.
Sánchez, S., Troncoso, G., Criado, M. T., and Ferreirós, C., “In vitro induction of memory-driven responses against Neisseria meningitidis by priming with Neisseria lactamica”. Vaccine. 2002. Volume 20. p. 2957-2963.
Slonczewski, J., and Foster, J. Microbiology: An Evolving Science. New York: W. W. Norton, 2009.
Taha, M. K., Deghmane, A. E., Antignac, A., Leticia Zarantonelli, M., Larribe, M., and Alonso, J. M. “The duality of virulence and transmissibility in Neisseria meningitidis”. Trends in Microbiology. 2002. Volume 10. p. 376-382.
Tzeng, Y. L. and Stephens, D. “Epidemiology and pathogenesis of Neisseria meningitides”. Microbes and Infection. 2000. Volume 2. p. 687-700.
Edited by student of Joan Slonczewski for BIOL 238 Microbiology, 2009, Kenyon College.