Early gut colonization and type 1 diabetes mellitus: Difference between revisions
Kmuenzen6395 (talk | contribs) No edit summary |
Kmuenzen6395 (talk | contribs) No edit summary |
||
| Line 39: | Line 39: | ||
Phylum: Actinobacteria | Phylum: Actinobacteria | ||
Class: Actinobacteria | Class: Actinobacteria | ||
Order: Bifidobacteriales | Order: Bifidobacteriales | ||
Family: Bifidobacteriaceae | Family: Bifidobacteriaceae | ||
Genus: Bifidobacterium29 | Genus: Bifidobacterium29 | ||
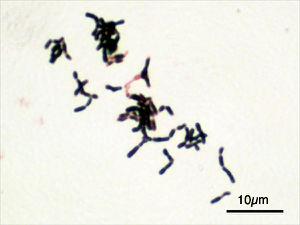
Bifidobacterium is a | The genus Bifidobacterium is a group of [http://en.wikipedia.org/wiki/Gram-positive_bacteria Gram-positive], rod-shaped anaerobic microbes that typically inhabits the [http://en.wikipedia.org/wiki/Human_gastrointestinal_tract gastrointestinal tract] (GIT) and urogenital tract of mammals. These bacteria thrive in temperatures between 36 and 38 <sup>o</sup>C and in a pH range of 6.5 to 7.22. Bifidobacteria that reside in the human body are typically isolated from the feces of adults and infants.29 Accordingly, Bifodobacteria thrive in the mammalian GIT, which is supplied with a constant source of carbohydrates, has a pH that remains within the range of 5.7 to 7.4, and has a temperature range of 37 and 42 <sup>o</sup>C.24 In most healthy adults, Bifidobacteria predominate in the gut microbiotia (108-109 cells/g of intestinal content) for the host’s entire lifetime. | ||
Bifidobacteria that | Bifidobacteria express a unique [http://en.wikipedia.org/wiki/Fructose-6-phosphate_phosphoketolase fructose-6-phosphate phosphoketolase] pathway that drives the fermentation of carbohydrates—most notably the non-digestible oligosaccharides commonly found in breast milk. This fermentation pathway, termed the “bifid shunt,” allows these bacteria to ferment a wide variety of carbon sources and results in the formation of acetic and [http://en.wikipedia.org/wiki/Lactic_acid lactic acids]. | ||
===Dendritic Cell Modulation=== | ===Dendritic Cell Modulation=== | ||
In the context of T1DM, | In the context of T1DM, antigen-presenting [http://en.wikipedia.org/wiki/Dendritic_cell dendritic cells] (DCs) initiate T-cell-induced autoimmunity by engulfing beta cell autoantigens and releasing cytokines (http://en.wikipedia.org/wiki/Cytokine) that induce cytotoxic T cell proliferation19. The specific antigen recognition and tolerance profile of each active dendritic cell is highly dependent on a process called [http://lab.rockefeller.edu/steinman/dendritic_intro/maturationDendritic maturation], which is influenced both by the stimuli provided by the engulfed autoantigen and by other members of the immune environment that interact with antigen-presenting cells. A 2006 in vitro study of the effects of Bifidobacterium breve on DC maturation showed that the supernatent of a Bifidobacterium breve C50 strain (BbC50SN) upregulated [http://en.wikipedia.org/wiki/Co-stimulation costimulatory molecule] expression by activated DCs (BbC50SN-DCs), increased the production of the anti-inflammatory cytokine [http://en.wikipedia.org/wiki/Interleukin_10 IL-10], and increased the average lifespan of DCs.18 The same study found that BbC50SN downregulated the expression of cytokine [http://en.wikipedia.org/wiki/Interleukin_12 IL-12], a pro-inflammatory molecule that stimulates the differentiation of T cells into pro-inflammatory Th1 helper cells. An overactive Th1 response has been correlated with amplified infiltration of CD8+ into the islets of Langerhans, and thus with the pathogenesis of T1DM.20 | ||
====TLR2 Mechanism==== | ====TLR2 Mechanism==== | ||
Recent evidence suggests that Bifidobacteria influence dendritic cell maturation through a TLR-2 pathway. Toll-like receptors are transmembrane proteins in antigen-presenting cells that recognize microbe-associated molecular patterns (MAMPs) | Recent evidence suggests that Bifidobacteria influence dendritic cell maturation through a [http://en.wikipedia.org/wiki/TLR2 TLR-2 pathway]. [http://en.wikipedia.org/wiki/Toll-like_receptor Toll-like receptors] are transmembrane proteins in antigen-presenting cells that recognize the differential [http://en.wikipedia.org/wiki/Pathogen-associated_molecular_pattern microbe-associated molecular patterns] (MAMPs) of pathogenic and non-pathogenic bacteria within the body. In particular, TLR2 recognizes the peptidoglycan and lipotechoic acids present in the cell membrane of Gram-positive bacteria and is responsible for mounting the innate immune response against invading pathogens.20 orchestrates dendritic cell maturation and activation.25 As a genus of Gram-positive bacteria, Bifidobacteria are recognized by the surface TLRs of dendritic cells from the moment they enter the infant GIT and act as TLR2 ligands, which initiate the TLR2 immune pathway when bound to their respective TLR receptors on the surface of dendritic cells. In this way, | ||
The symbiotic interaction between Bifidobacteria and the | The symbiotic interaction between Bifidobacteria and the mammalian immune system can be explained in part by the “old friends hypothesis,” which proposes that mammalian coevolution with microorganisms in the host gut allows the host immune system to recognize the once-foreign bacteria as “self.” Meanwhile, these microbes interact with the host digestive and immune systems, aiding in proper digestion of a wide variety of carbohydrates and priming immune system members for immunoregulation.26 When Bifidobacteria act as [http://www.invivogen.com/tlr2-ligands ligands] for TLR2 proteins in dendritic cells, they induce a constant background of low-grade [http://en.wikipedia.org/wiki/Regulatory_T_cell regulatory T cell] (Treg) upregulation. In turn, these Treg cells downregulate proinflammatory processes, maintaining a healthy population of “old friends” within the gut and increasing tolerance to “self.” Upon binding to TLR receptors, symbiotic gut bacteria like Lactobacilli present their DNA to APCs in a “package” that identifies them as “self.”27 The exact mechanism behind this interaction is still under study...more here (chrons model) | ||
==Probiotic treatments for type 1 diabetes== | ==Probiotic treatments for type 1 diabetes== | ||
Revision as of 06:10, 14 April 2015

Caesarean section, commonly known as C-section, is a surgical procedure that allows pregnant women to deliver one or more babies through incisions made in the abdomen and uterus. In the case that vaginal delivery poses a serious threat to the health to either the mother or the child, C-section is a successful and often necessary alternative to vaginal delivery. From 1996 to 2009, the rate of C-section among all gestational age groups increased by more then 40 percent in the United States alone, a trend that has benefited from an increase in social tolerance of surgical intervention, from monetary incentives on the part of healthcare providers and from limited patient awareness of short and long-term risks associated with the procedure1,2.
Recent medical interest in the human gut flora, or gut microbiotia, has yielded multiple studies that suggest that mode of delivery heavily impacts early colonization of the infant gut microbial community and potentially alters the long-term composition and diversity of the gut microbiotia. Furthermore, a growing body of evidence links both aberrance of the gut microbiotia and mode of delivery with increased risk for immune disorders including allergy, gastrointestinal disease, and type 1 diabetes mellitus3. Coincidently, the American Diabetes Association reported a 23 percent increase in the number of reported cases of type 1 diabetes from 2001 to 2009, a trend that may be driven by a variety of environmental factors4. As a potential risk factor for type 1 diabetes, C-section and consequent aberrance of the gut microbiotia have recently received scrutiny in the context of early and late immune health.
Modes of Delivery
Vaginal Delivery
When an infant passes through its mother’s birth canal during vaginal delivery, it is exposed to its first non-sterile environment outside the uterus via direct contact with the vagina and its own mucous membranes. The vagina is typically colonized by a wide variety of anaerobic bacteria and is dominated by several species of lactic acid bacteria5,6. During delivery, infants also come into contact with the microbes that colonize their mothers’ feces as a result of the proximity of the birth canal and the anus5 Direct contact with the mother’s lower genital tract and anus initiates colonization of the infant’s skin and oral mucosa, and eventually of the infant’s intestinal tract, which is first dominated by facultative anaerobes including enterobacteria and lactobacilli, and then dominated by other anaerobes including Bifidobacteria, Bacteroides, Clostridia and Eubacteria7. Following expulsion from the birth canal, infants are continuously exposed to environmental, oral and cutaneous microbes through mother-infant contact and environmental exposure, and they continue to ingest gut-colonizing microbes during the breastfeeding process. By two years of age, most healthy infants show a gut microbial composition similar to that of a typical healthy adult5.
Caesarean Section
During delivery by C-section, the infant bypasses the birth canal and is directly removed from the mother’s body through incisions made in her abdomen and uterus8. As opposed to initial microbial exposure via direct vaginal and anal contact, infants delivered by C-section are initially exposed to microbial isolates from the medical and nursing staff, surgical equipment and other elements of the immediate external environment5. As a result, early microbial composition—including diversity and total cell count—of the skin and oral/nasal mucosa in infants delivered by C-section differs greatly from the early microbiotia of infants delivered vaginally. Directly following delivery, the skin and oral/nasal mucosa microbiotia of vaginally delivered infants resemble the mother’s vaginal microbiotia and are dominated by the Lactobacillus genus. The microbiotia of infants delivered by C-section closely resemble the microbiotia of skin surfaces and is dominated by Staphylococcus9.
Gut Microbiotia Aberrance
Initial colonization of the skin and mucous membranes is closely linked with the successive colonization of the infant intestinal tract, whose composition is highly affected by the initial composition of the mucosal microbiotia. During the first month of life, the infant gut microbiotia is composed predominantly of Bifidobacteria, a genus of Gram-positive anaerobes that are found in moderate numbers in the lower female genital tract. In a 2007 study that controlled for variant breastfeeding among test subjects, a group of researchers from Finland found that the number of bifidobacteria in vaginally delivered infants was 1,300-fold higher than in infants delivered by C-section at one month of age7. The same study reported significantly hampered mucosal immunity in C-section infants at 6 months of age, which suggests that early composition of the gut microbiotia may be related to immune health.
Type 1 diabetes
Type 1 diabetes mellitus (T1DM), commonly known as type 1 diabetes, is a metabolic autoimmune disease that develops in early childhood or adolescence. The disease is characterized by chronic hyperglycemia, which results from defects in insulin production due to autoimmune destruction of insulin-producing beta cells in the pancreas11. The precise cause of T1DM is so far unknown, although individuals with a family history of the disease are known to be at higher risk for developing T1DM. Beyond genetic susceptibility, T1DM is currently thought to be triggered by one or more environmental factors12.
Pathophysiology
Within the pancreas, regions of endocrine cells called the islets of Langerhans are responsible for producing hormones like glucagon, insulin and amylin. Beta cells, which are one of the five secretory cells located within the islets of Langerhans, are responsible for storing and secreting insulin and amylin directly into the bloodstream. When beta cells become damaged or undergo turnover, they release autoantigens which, in healthy individuals, are not recognized by the immune system16. However, when these autoantigens are received by antigen-presenting cells within the pancreas that recognize the autoantigens as foreign bodies, namely macrophages and dendritic cells, CD4+ T cells become activated by the signals secreted by the antigen-presenting cells. These activated CD4+ T cells induce the differentiation of CD8+ T cells into cytotoxic T cells, which are involved in the destruction of beta cells14.
Animal Models
Recent studies of type 1 diabetes in animal models suggest that the composition of the gut microbiotia is closely linked with autoimmune diabetes. In a 2009 study that compared the bacterial genera in the guts of diabetes resistant (BB-DR) and diabetes-prone (BB-DP) biobreeding rats, researchers found a higher abundance of the probiotic Lactobacillus and Bifidobacterium genera in BB-DR rats, suggesting that a lack of these bacteria in the rodent gut microbiotia is associated with the onset of type 1 diabetes13. As the most likely culprit of beta cell autoimmunity, antigen-specific T cell activation in diabetic individuals may be induced by the presence and/or absence of specific bacteria within the gut, which may determine an individual’s risk for developing autoimmune diabetes.
Immunomudulatory effects of Bifidobacteria
As a demonstrated key component of the commensal gut microbiotia and as an organism correlated with type 1 diabetes resistance, the genus Bifidobacterium is of great interest in the context of the immune system. Although specific metabolic characterization of intestinal Bifidobacteria within the larger immune system is still an emerging science, recent studies have demonstrated the significant anti-inflammatory effects of the Bifidobacteria and its critical role in both the homeostasis of the intestine and in dendritic cell modulation.17
Characterization of Bifidobacteria
Phylum: Actinobacteria
Class: Actinobacteria
Order: Bifidobacteriales
Family: Bifidobacteriaceae
Genus: Bifidobacterium29
The genus Bifidobacterium is a group of Gram-positive, rod-shaped anaerobic microbes that typically inhabits the gastrointestinal tract (GIT) and urogenital tract of mammals. These bacteria thrive in temperatures between 36 and 38 oC and in a pH range of 6.5 to 7.22. Bifidobacteria that reside in the human body are typically isolated from the feces of adults and infants.29 Accordingly, Bifodobacteria thrive in the mammalian GIT, which is supplied with a constant source of carbohydrates, has a pH that remains within the range of 5.7 to 7.4, and has a temperature range of 37 and 42 oC.24 In most healthy adults, Bifidobacteria predominate in the gut microbiotia (108-109 cells/g of intestinal content) for the host’s entire lifetime.
Bifidobacteria express a unique fructose-6-phosphate phosphoketolase pathway that drives the fermentation of carbohydrates—most notably the non-digestible oligosaccharides commonly found in breast milk. This fermentation pathway, termed the “bifid shunt,” allows these bacteria to ferment a wide variety of carbon sources and results in the formation of acetic and lactic acids.
Dendritic Cell Modulation
In the context of T1DM, antigen-presenting dendritic cells (DCs) initiate T-cell-induced autoimmunity by engulfing beta cell autoantigens and releasing cytokines (http://en.wikipedia.org/wiki/Cytokine) that induce cytotoxic T cell proliferation19. The specific antigen recognition and tolerance profile of each active dendritic cell is highly dependent on a process called maturation, which is influenced both by the stimuli provided by the engulfed autoantigen and by other members of the immune environment that interact with antigen-presenting cells. A 2006 in vitro study of the effects of Bifidobacterium breve on DC maturation showed that the supernatent of a Bifidobacterium breve C50 strain (BbC50SN) upregulated costimulatory molecule expression by activated DCs (BbC50SN-DCs), increased the production of the anti-inflammatory cytokine IL-10, and increased the average lifespan of DCs.18 The same study found that BbC50SN downregulated the expression of cytokine IL-12, a pro-inflammatory molecule that stimulates the differentiation of T cells into pro-inflammatory Th1 helper cells. An overactive Th1 response has been correlated with amplified infiltration of CD8+ into the islets of Langerhans, and thus with the pathogenesis of T1DM.20
TLR2 Mechanism
Recent evidence suggests that Bifidobacteria influence dendritic cell maturation through a TLR-2 pathway. Toll-like receptors are transmembrane proteins in antigen-presenting cells that recognize the differential microbe-associated molecular patterns (MAMPs) of pathogenic and non-pathogenic bacteria within the body. In particular, TLR2 recognizes the peptidoglycan and lipotechoic acids present in the cell membrane of Gram-positive bacteria and is responsible for mounting the innate immune response against invading pathogens.20 orchestrates dendritic cell maturation and activation.25 As a genus of Gram-positive bacteria, Bifidobacteria are recognized by the surface TLRs of dendritic cells from the moment they enter the infant GIT and act as TLR2 ligands, which initiate the TLR2 immune pathway when bound to their respective TLR receptors on the surface of dendritic cells. In this way,
The symbiotic interaction between Bifidobacteria and the mammalian immune system can be explained in part by the “old friends hypothesis,” which proposes that mammalian coevolution with microorganisms in the host gut allows the host immune system to recognize the once-foreign bacteria as “self.” Meanwhile, these microbes interact with the host digestive and immune systems, aiding in proper digestion of a wide variety of carbohydrates and priming immune system members for immunoregulation.26 When Bifidobacteria act as ligands for TLR2 proteins in dendritic cells, they induce a constant background of low-grade regulatory T cell (Treg) upregulation. In turn, these Treg cells downregulate proinflammatory processes, maintaining a healthy population of “old friends” within the gut and increasing tolerance to “self.” Upon binding to TLR receptors, symbiotic gut bacteria like Lactobacilli present their DNA to APCs in a “package” that identifies them as “self.”27 The exact mechanism behind this interaction is still under study...more here (chrons model)
Probiotic treatments for type 1 diabetes
Further Reading
References
1. Osterman MJK, Martin JA. Changes in cesarean delivery rates by gestational age: United States, 1996–2011. NCHS data brief, no 124. Hyattsville, MD: National Center for Health Statistics. 2013. http://www.cdc.gov/nchs/data/databriefs/db124.htm#x2013;2011</a
2. "Why Is the National U.S. Cesarean Section Rate So High?" Why the National U.S. C-Section Rate Is So High. N.p., n.d. Web. http://www.childbirthconnection.org/article.asp?ck=10456
3. Cho, C. E., & Norman, M. “Cesarean section and development of the immune system in the offspring.” American Journal of Obstetrics and Gynecology 208.4 (2013): 249–54. Web. http://www.ncbi.nlm.nih.gov/pubmed/22939691
4. "Growing Number of Autoimmune Disease Cases Reported." Newswise. American Autoimmune Related Diseases Association, 21 June 2012. Web. http://www.newswise.com/articles/growing-number-of-autoimmune-disease-cases-reported
5. Mackie RI, Sghir A, Gaskins HR. Developmental microbial ecology of the neonatal gastrointestinal tract. Am J Clin Nutr 1999; 69: 1035S–1045S. http://ajcn.nutrition.org/content/69/5/1035s.short
6. Vásquez, Alejandra et al. “Vaginal Lactobacillus Flora of Healthy Swedish Women.” Journal of Clinical Microbiology 40.8 (2002): 2746–2749. PMC. Web. 20 Mar. 2015. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC120688/
7. Huurre, Anu, et al. "Mode of delivery-effects on gut microbiota and humoral immunity." Neonatology 93.4 (2008): 236. Web. http://www.ncbi.nlm.nih.gov/pubmed/18025796
8. "C-Section: What Can You Expect for Recovery?" MedicineNet. N.p., n.d. Web. http://www.medicinenet.com/c-section_cesarean_birth/article.htm
9. Dominguez-Bello MG, Costello EK, Contreras M, Magris M, Hidalgo G, Fierer N & Knight R. “Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns.” PNAS 107 (2010): 11971–11975. http://www.pnas.org/content/107/26/11971.full
11. "About diabetes". World Health Organization. http://www.who.int/diabetes/action_online/basics/en/
12. Belle, T. L. Van, K. T. Coppieters, and M. G. Von Herrath. "Type 1 Diabetes: Etiology, Immunology, and Therapeutic Strategies." Physiological Reviews 91.1 (2011): 79-118. Web. http://www.ncbi.nlm.nih.gov/pubmed/21248163
13. Roesch, Luiz Fw, Graciela L. Lorca, George Casella, Adriana Giongo, Andres Naranjo, Arianna M. Pionzio, Nan Li, Volker Mai, Clive H. Wasserfall, Desmond Schatz, Mark A. Atkinson, Josef Neu, and Eric W. Triplett. "Culture-independent Identification of Gut Bacteria Correlated with the Onset of Diabetes in a Rat Model." The ISME Journal 3.5 (2009): 536-48. Web. http://www.ncbi.nlm.nih.gov/pubmed/19225551
14. Yoon J.-W., Jun H.-S. Autoimmune destruction of pancreatic β cells. American Journal of Therapeutics. 2005;12(6):580–591. http://www.ncbi.nlm.nih.gov/pubmed/16280652
16. Poletaev AB, Churilov LP, Stroev YI, Agapov MM. (2012). "Immunophysiology versus immunopathology: Natural autoimmunity in human health and disease." Pathophysiology. http://www.pathophysiologyjournal.com/article/S0928-4680(12)00081-8/abstract
17. Hart, A. L. "Modulation of Human Dendritic Cell Phenotype and Function by Probiotic Bacteria." Gut 53.11 (2004): 1602-609. Web. http://gut.bmj.com/content/53/11/1602.long#ref-8
18. Hoarau C, Lagaraine C, Martin L, Velge-Roussel F, Lebranchu Y. Supernatant of Bifidobacterium breve induces dendritic cell maturation, activation, and survival through a Toll-like receptor 2 pathway. J Allergy Clin Immunol. 2006;117:696–702. http://www.ncbi.nlm.nih.gov/pubmed/16522473
Edited by Kathleen Muenzen, a student of Nora Sullivan in BIOL168L (Microbiology) in The Keck Science Department of the Claremont Colleges Spring 2014.
