Eyes: Difference between revisions
| Line 108: | Line 108: | ||
==References== | ==References== | ||
( | (M1) http://physiologyonline.physiology.org/cgi/content/full/13/2/97 | ||
( | (M2) http://www.nature.com/eye/journal/v17/n8/full/6700566a.html | ||
( | (M3) http://www.tedmontgomery.com/the_eye/cornea.html | ||
( | (M4) http://www.lea-test.fi/en/eyes/lidsncha.html | ||
( | (M5) http://bjo.bmj.com/cgi/content/abstract/68/8/524 | ||
( | (M6) http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6WFD-49H6Y6X-1&_user=10&_rdoc=1&_fmt=&_orig=search&_sort=d&view=c&_version=1&_urlVersion=0&_userid=10&md5=cae06adc263756d8bb890e5f40005b89#toc1 | ||
(M7) http://www.iovs.org/cgi/content/abstract/42/10/2347 | |||
(7) BV | (7) BV | ||
Revision as of 20:04, 27 August 2008
Description of Niche
Where located?
Physical Conditions?
What are the conditions in your niche? Temperature, pressure, pH, moisture, etc.
Influence by Adjacent Communities (if any)
Is your niche close to another niche or influenced by another community of organisms?
Conditions under which the environment changes
Do any of the physical conditions change? Are there chemicals, other organisms, nutrients, etc. that might change the community of your niche.
Tears
Tears are secretion from tear glands to lubricate and protect eyes from infection. The tear film allows gas exchange between the air and the epithelium and also keeps the cornea wet. The substance of the tear film is retinol to provide the transparent nature of the epithelium. (1) Tears are composed of water, electrolytes, proteins (albumin, globulin, and lysozyme), lipid, mucins and others. They are weak base. (2)
Tear production system The protection of tears has three separate layers: the lipid layer, the aqueous layer, and the mucous layer. The outermost lipid layer contains oils produced by the meibomian glands. It is a thin layer (0.1-0.2µm and hydrophobic surface, so it reduces evaporation of water. The temperature in meilbomain gland lipids has the low melting point range 19-32°C depending on the degree of fatty acids unsaturation. The meibomain gland lipids allow lipid get through the meibomian gland ducts and excretion to the tear film. The aqueous layer is a tear film including water and proteins produced by the lacrimal gland. The middle layer of the lacrimal gland is the thickest (7-8µm) and produces 0.9% saline tears. It functions delivery the main nutrients such as oxygen to the cornea and carrying waste products away from the cornea The innermost mucous layer (30µm) contains mucin produced by goblet cells. Its thin layer of hydrophilic surface can make even on the corneal surface to spread water. (1,3,4 and 5)
Many species of bacteria are found in the eyelid and conjunctiva as symbiotic relationships. These are Staphylococcus aureus (S. aureus), Staphylococcus epidermidis, Streptococcus, Corynebacterium, Propionibacterium, and Propionibacterium acnes. These bacteria produce lipase that harm to the tear film lipid layer especially, S. epidermidis and S. aureus produce triglyceride lipase and cholesterol and wax esterase. Accumulated cholesterol is used for the growth of certain ocular bacteria. Increased bacteria are regulated by anti-microbial peptides from the lacrimal gland and conjunctiva. (6)
Who lives there?
Microbe Interactions
Many normal bacteria are present in the human eye which includes Staphylococcus, Staphylococcus aureus, Haemophilus species, and Streptococcus species. However, many other outside bacteria compete for their stay in the eye niche that may lead to tragic diseases and unfavaorable results.
The most common bacteria that can cause corneal ulcer, which could lead to the development of eye blindness, are staphylococcal species, Pseudomonas aeruginosa, Streptococcus pneumoniae, and Moraxella species. Of these, Pseudomonas aeruginosa is found to be the primary bacterium when wearing contact lens, typically soft contacts, that can cause corneal ulcer. Pseudomonas Aeruginosa is a gram-negative, aerobic rod-shaped bacterium which optimally grows at 42 degrees celcius. Although classified as aerobic, it can adapt and live in anaerobic environments. Being an opportunist, this bacterium greatly affects the eye when the defensive mechanisms of the eye are weakened. Otherwise, it does not ordinarily cause disease. It is, however, a very durable bacterium, some of which includes minimal food requirement, a protective outer coating, and resistance to many antibiotics (P1).
A study from the United Kingdom reported that people who wear soft contact lenses result in 8 times more of a chance for bacteria to invade in the cornea when they sleep than the people who only wear them while they are awake (P2).
Dr. Gifford Jones of canadafreepress.com had reported that people who wore contact lens are at risk of developing blinding eye infections during the first six months of use. He proposed that it depended on what the contact lenses were made of. It was said that Pseudomonas aeruginosa infection for soft contact lenses is one in 2,500 and one in 500 if it was worn overnight. For hard contact lenses, infection is one in 10,000. Biodeposits build up on the contact lenses which can cause irritation and corneal ulcers. When contact lenses are worn, it covers up the cornea which restricts oxygen flow to underlying tissues. In an anaerobic environment, Pseudomonas aeruginosa is then able to reside properly. Dr. Dwight Cavanagh, a professor of Opthlalmology at the University of Texas Southern Medical School, stated that new cells on the cornea cannot be produced when the contact lenses cover it, which may decrease the thickness of the cornea by 10 percent (P3).
In 1993, The Department of Ophthalmology at University of Patras medical School in Greece, performed an experiment to determine the clinical microbiological characteristics of corneal ulcers in contact lens wearers. Results showed that, of the ulcerative keratitis patients, 26.74% of them wore contacts. In addition, Pseudomonas aeruginosa was the most frequent isolated bacterium. This experiment concluded that the use of contact lens has a high risk factor for ulcerative keratitis (P4).
Also, a study in Sydney of 2003, Australia found that Pseudomonas aeruginosa produce quorum-sensing signal moleucules which contributed to the induction of the inflammatory response in Pseudomonas keratitis (P5).
Pseudomonas aeruginosa in the eye is targeted by the use of an antibiotic called ciprofloxacin. Current research shows that ciprofloxacin is very effective in treating ulcerative keratitis, although there have been rare results of the bacterium being resistant to the antibiotic, possibly due to the bacterium’s adaptation (6). Pseudomonas aeruginosa has increased its resistance to many antibiotics up to today. Patients who are treats Pseudomonas aeruginosa often have to take multiple antibiotics due to the bacterium’s high barrier of antibiotic resistance (P1).
Fungal Infestation of the Eye Niche
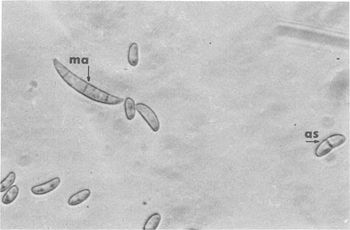
Common fungi found in the Eye: - Acremonium spp. - Aspergillus flavus - Aspergillus fumigatus - Aspergillus niger - Bipolaris spp. - Candida albicans - Curvularia spp - Exserohilum spp. - Fusarium oxysporum - Fusarium solani - Lasiodiplodia theobromae
The warm and moist environment of the eye is subject to mycotic infections from fungal species such as Fusarium, Aspergillus, Acremonium, and the Candida species of yeasts. Due to the preferences for moisture-rich environments and warm weather, the prevalence of fungal infections of the eye is higher in tropical areas and in areas with large agrarian communities [9]. Despite the relatively sterile environment of the eye, factors such as eye “trauma (generally with plant material), chronic ocular surface diseases, contact lens usage, corneal anesthetic abuse and immunodeficiencies” can result in infection of the eye by filamentous fungi or yeasts [8]. Fusarium solani, a species of fungi that is associated with contact lens wearers, normally inhabits warmer climates in soil and organic matter. Invasion of the inner layers of contact lenses and transfer to the surface of the eye, however, is possible due to the ability of Fusarium solani to reside in the moisture-rich inner matrix of soft contact lenses [7].
Fungal infections, such as fungal keratitis, can occur on the anterior surface of the eye or the cornea, and may also infect the posterior of the eye as a result of mycosis. Fungi that inhabit the eye produce proteases that are specific for the surface on which they grow [7]. As a result, protein catabolism by fungal proteases results in tissue damage to the eye, ulceration as well as an inflammatory response around the infected area [7]. Aggregation of fungal microbes into hyphae enlarges the infected region and prevents host inflammatory cells from ingesting the fungi. As a result of the pattern of fungi to join together and form hyphae, fungi that inhabit the eye may extend throughout the entire depth of the cornea, and tend to grow parallel to the lamellae of the cornea [7][8]. As a result of catabolic degradation of the eye environment by the fungi, an inflammatory response by the host is accompanied by necrosis of the surrounding eye tissues [8].
Fungal infection of the eye may occur as a result of fungal growth on contact lenses. Due to tendency of fungi to inhabit moisture-rich locations, contact lens cases and the soft inner matrix of contact lenses are subject to fungal growth [7]. Fungi have the ability to degrade hydrophilic polymers of contact lenses, and may be transferred from contaminated lenses to the surface of the eye, often causing the implantation of fungi into the anterior regions of the eye or the cornea and result in fungal keratitis [7].
Do the microbes that are present interact with each other?
Describe any negative (competition) or positive (symbiosis) behavior
Do the microbes change their environment?
Do they alter pH, attach to surfaces, secrete anything, etc. etc.
Do the microbes carry out any metabolism that affects their environment?
Do they ferment sugars to produce acid, break down large molecules, fix nitrogen, etc. etc.
Defense Mechanisms of the Eye
Barely any microbes live in the eye. This stems from the fact that each section within the eye has mechanisms that defend against infection and microbe colonization.
Blink Reflex
The blink reflex is a mechanical defense against particles in the air or trauma. Eyelashes and the sensitive cornea both participate in this reflex. Tears, debris, allegans, microbes, etc. are moved over to the lacrimal excretory system with the motion from the eyelid.
Barriers
The orbital septum, cornea and conjunctiva all provide a protective barrier against pathogens. The orbital septum divides the orbit from the eyelid into pre and postseptal spaces which allows for a physical barrier against infections. The various layers of the cornea limit permeability of items into the eye. Also, native flora of the lids and mucosal surface limit possible pathogenic colonization.
Tears
Tears provide a mechanical defense via flushing of foreign particles from the surface of the eye and transporting antimicrobial agents to the surface as defensive measures.
Immune Response
The cornea, due to lack of a vascular system, contains limited immune defenses. Immune defenses are provided by Langerhans cells and immunoglobulins. Langerhans cells modify B and T cell in the cornea Glycocalx coupled with a mucous glycoprotein layer covers the corneal surface for added protection.
Langerhans cells have receptors for immunoglobulins, antigen, and complement. They work like macrophages to destroy foreign invaders. The B and T cells that are modified by Langerhans cells work in conjunction with lymphocytes, resulting in a strong immune reponse.
Leukocyte Defense Leukocytes consume and destroy microorganisms via and oxygen-dependent pathway and oxygen-independent pathway. The oxygen-dependent pathway uses oxygen radicals while the oxygen-independent pathway utilizes defensins, which are antimicrobial proteins consisting of peptides that have broad antimicrobial activity, destroying gram-positive and gram-negative bacteria, some fungi, and various pathogens in the eye.
Current Research
1. Iris Pigment Epithelium Expressing CD86 (B7-2) Directly Suppresses T Cell Activation In Vitro via Binding to Cytotoxic T Lymphocyte–associated Antigen 4
A current study at Schepens Eye Research Insitute at Harvard Medical School identified the thin layer of cells lining the iris of the eye, the iris pigment epithelium (IPE), as a tissue that contributes to ocular-immune privilege by secreting immunosuppressive factors and expressing surface molecules that trigger apoptosis by T cells. Scientists exposed PE cells from various regions of the eye to purified T Cells and found that only the IPE cells from the iris responded to CD86 by stopping T cell activity. Normally, T cell activity in the body promotes inflammation. By suppressing its activity, however, IPE cells are able to prevent inflammation in the eye. The results demonstrated that IPE cells contribute to immune privilege and prevent eye inflammation in the iris. The study identified that disruption of IPE cell activity in the eye, perhaps by infection or other factors, may lead to immunogenic inflammation, disruption of the visual axis and blindness [10].
2. Viral Infection of the Lungs through the Eye
Respiratory syncytial virus (RSV) is a virus that is greatly known to affect the respiratory system of newborns. Researchers discovered an association of this virus with allergic conjunctivitis, also known as Pink Eye, which allowed the virus to flow toward the respiratory system initially from the eyes. They experimented on a live mouse by applying RSV to its eyes. RSV not only replicated but also drifted to the lungs, which produced a respiratory disease. Treatment of RSV with anticytokine was successful. They concluded that respiratory infections could be involved with the eye and that it can be treated. [P7]
3. Phospholipase A2 in Rabbit Tears: A Host Defense against Staphylococcus aureus
Staphylococcus aureus cause keratitis in many human populations. Tear films has many nutrients that are good for bacteria growth. However, tear films has an effective defense system to reduce bacteria replication and regulate bacteria growth. One of inhibitors for the host defense molecule is phosholipase A2 (PLA2). Moreau et al. studied the PLA2 effect on staphylococcal activity. They found PLA2 killed staphylococcus by hydrolyzing bacteria membranes to release fatty acids and destroyed the bacterial cell wall. [M7]
References
(M1) http://physiologyonline.physiology.org/cgi/content/full/13/2/97
(M2) http://www.nature.com/eye/journal/v17/n8/full/6700566a.html
(M3) http://www.tedmontgomery.com/the_eye/cornea.html
(M4) http://www.lea-test.fi/en/eyes/lidsncha.html
(M5) http://bjo.bmj.com/cgi/content/abstract/68/8/524
(M7) http://www.iovs.org/cgi/content/abstract/42/10/2347
(7) BV
(8) BV
(9) BV
(10) Sugita, S., J. Streilein. “Iris Pigment Epithelium Expressing CD86 (B7-2) Directly Suppresses T Cell Activation In Vitro via Binding to Cytotoxic T Lymphocyte–associated Antigen 4.” J. Exp. Med., Jul 2003; 198: 161 - 171.
(P2) http://www.emedicine.com/emerg/topic115.htm
(P3) http://www.canadafreepress.com/medical/ear-nose-throat030203.htm
(P6) http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1920786
(P7) http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1797451

