Gonorrhoea (Neisseria gonorrhoeae) in the United States: Difference between revisions
No edit summary |
|||
| Line 1: | Line 1: | ||
==Introduction== | ==Introduction== | ||
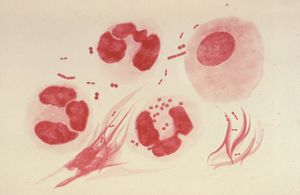
[[Image:Gonorrhea.jpg|thumb|Neisseria gonorrhoeae. Image courtesy of CDC/Dr. Norman Jacobs]] | |||
Globally, gonorrhea is one of the most commonly transmitted venereal diseases. First used in the second century by Aelius Galenus, a Roman physician and philosopher, the term literally translates to “flow of seed” [2]. In the sixth century, the disease and treatments of pelvic abscesses caused by gonorrhea is described by a Byzantine physician and medical writer, Aetius Amidenus. The disease also became prevalent in France, being well known by one of its symptoms as ‘La chaude pisse’ which meant hot piss. [1] In 1879, a German physician and bacteriologist, Albert Ludwig Sigesmund Neisser was the first person to describe the bacterium, Neisseria gonorrhoeae as the causative agent of gonorrhea. | Globally, gonorrhea is one of the most commonly transmitted venereal diseases. First used in the second century by Aelius Galenus, a Roman physician and philosopher, the term literally translates to “flow of seed” [2]. In the sixth century, the disease and treatments of pelvic abscesses caused by gonorrhea is described by a Byzantine physician and medical writer, Aetius Amidenus. The disease also became prevalent in France, being well known by one of its symptoms as ‘La chaude pisse’ which meant hot piss. [1] In 1879, a German physician and bacteriologist, Albert Ludwig Sigesmund Neisser was the first person to describe the bacterium, Neisseria gonorrhoeae as the causative agent of gonorrhea. | ||
Revision as of 09:06, 27 August 2009
Introduction
Globally, gonorrhea is one of the most commonly transmitted venereal diseases. First used in the second century by Aelius Galenus, a Roman physician and philosopher, the term literally translates to “flow of seed” [2]. In the sixth century, the disease and treatments of pelvic abscesses caused by gonorrhea is described by a Byzantine physician and medical writer, Aetius Amidenus. The disease also became prevalent in France, being well known by one of its symptoms as ‘La chaude pisse’ which meant hot piss. [1] In 1879, a German physician and bacteriologist, Albert Ludwig Sigesmund Neisser was the first person to describe the bacterium, Neisseria gonorrhoeae as the causative agent of gonorrhea.
STATISTICS
Although a cure exists, statistics show that cases of infection are still on the rise. Today, gonorrhea is one of the leading reported sexually transmitted diseases in adults in the United States. The reoccurring trend of increasing rates of gonorrhea infection can be seen uniformly across regions, states, sex, age, and race/ethnicity. In 2007, 355,991 cases of gonorrhea were reported in the United States. This equates to roughly 118.9 cases per 100,000 people in 2007. [4] This rate of gonorrhea infection has remained relatively stable the past decade, especially among women. The gonorrhea rate among women was reported at 123.5 and the rate among men was reported at 113.7 cases per 100,000 people in 2007 [4]. In the same year, the gonorrhea rates continue to be the highest among young adults and adolescents; among females in the ages of 15 – 24 and among males between the ages of 20 – 24. The data suggests that gonorrhea is still on the rise and further development of treatment beyond the boundaries of medication is needed.
Description of Gonorrhoea (Neisseria gonorrhoeae)
Description of the microbe
Neisseria gonorrhoeae (N. gonorrhoeae) is a gram-negative diplococcus ranging from 0.06 to 1.0 µm in diameter and is usually seen in pairs with adjacent flattened sides. The organism is typically observed inside polymorphonuclear leukocytes (neutrophils) that have become a part of the gonorrhea pustular exudates. Fimbriae are used by the bacteria for adherence, extending several micrometers from the cell surface [2]. N. gonorrhoeae have antigenic type IV pilus and the opacity (Opa) proteins. It moves by long pili that are constituted of repeated peptide subunits (pilin) characterized by both antigenic and phase variations. The bacterium is able to rearrange its chromosomal DNA altering the expression of any one of several silent pilin genes. [3] By doing so, phase variation (pi + to pil-) occurs when the rearrangement involves a defective pilin gene or to avoid their host cell (humans) immune system [1,3]. The tight junctions and adherence to the host cell is due by the Opa proteins. The bacterium, like N. meningitidis, is also naturally competent for DNA uptake after attachment [4]. Since N. gonorrhoeae is a typical gram-negative bacteria, its outer membrane is composed of proteins, phospholipids, and lipopolysaccharides (LPS). The lipopolysaccharide can be distinguished from other typically LPS by its highly-branched basal oligosaccharide structure and the absence of repeating O-antigen subunits. So typically, the neisserial LPS is usually referred to as lipooligosaccharide (LOS). During growth, it releases outer membrane fragments called "blebs" which contains LOS and has a role in pathogenesis when they are spread during an infection [2]. N. gonorrhoeae infect the mucous surfaces that are lined with columnar epithelium cells by the attachment of the bacterium via pili (fimbriae) and the production of lipopolysaccharide endotoxin [1, 2]. Due to the fact that the lipopolysaccharide is highly toxic and contains virulence factors in the form of its antiphagocytic capsule which produces IgA proteases, they contribute to the viral infection [2]. N. gonorrhoeae is a fragile organism that is easily susceptible to environmental change conditions including temperature changes, drying, UV light, and such. It is a "fastidious" bacterium that requires blood or hemoglobin and several amino acids and vitamins to nourish in order to grow. In the laboratory, cultures must be grown at 35-36 degrees in an atmosphere of 3-10% added CO2. [1]
Transmission of disease
Gonorrhea, which is caused by the bacterium N. gonorrhoeae, is harbored in warm and moist areas and sexually trasmitted through contact of an infected tissue surface on vaginal, penile, anus, or mouth [3, 4]. When left untreated, it can severely effect the uterus, cervix, and fallopian tubes in women and the urethra in men, potentially leading to sterility [2]. In addition to being transmitted sexually, it can be transmitted vertically from an infected, pregnant woman to the baby she is carrying. This infection can reach the offspring through the birth canal of the mother during delivery. [4]
Prevention
According to the CDC fact sheet, the best method for prevention is to abstain from sexual intercourse or to be in a long monogamous relationship with a partner that has been tested or treated for Gonorrhea. Other preventive measures include using latex condoms that can reduce risk of catching such STD. It is important to seek a doctor if any symptoms such as discharge or burning during urination or unusual sores or rash arise. Most importantly it is essential that to further spread such a disease those individuals that have been diagnosed to notify all previous partners to get tested immediately and to further prevent a serious outbreak of infections. It is also essential to get a routine screening for any groups at risk to constantly be aware of there medical history and condition before they engage in any high risk activity. Furthermore due to the development of resistance in Neisseria gonorrhea to the many antimicrobial classes brings a much needed challenge to the control of gonorrhea. Another unique prevention strategy implemented enhancement of national and international surveillance, to monitor resistance and to better compliment new strategies to essentially maximize the benefit and further prolong the utility of antimicrobials. This can include combination regimens, applying screening recommendations for those that are high risk for infection, and to further continue proper effective treatment for infected persons and their sexual partners. Testing every 3 to 4 months after treatment for initial infection is highly recommended to prevent re-infection. An article in Drug Week published March 20, 2009 tried to identify intervention strategies for prevention and control in San Francisco, found that there was a substantial gonorrhea increase among young heterosexuals during 2003-2005. The researchers concluded based on there case study that “Prevention and control efforts are focusing on blacks and incarcerated populations using street-based outreach and expanded screening and treatment.” (Barry, 616).
==Why is this disease a problem in the United StatesGonorrhea has been a silent disease in the United States (US) largely because anyone sexually active can be infected. The highest reported rates of infection in the US are among sexually active women and African Americans (CDC). It infects about 20,000 individuals each year. It was not long ago that gonorrhea was a serious concern to the public health like many other major STD or STI such as Syphilis, a top priority of all health organizations. However, according to the New York Times article by Lawrence K. Altman, Sex Diseases Still Rising; Chlamydia Is Leader, “From 1975 through 1997 the reported rate of gonorrhea dropped 74 percent, then plateau, only to rise the last two years to 358,366 cases in 2006. The actual numbers are estimated at about twice of that.” This issues raises concern in America especially because the American people have had the luxury of healthcare that many third world countries are not capable of receiving. It is apparent that safe sex practices had been abandoned and thus have resulted in a jump in gonorrhea cases recently. Another risk factor to consider in America is the disproportionately amount of African-Americans having the higher prevalence than any other ethnic groups. In comparison 18 to 1 ratio of African Americans to Whites. “African Americans account for 69 percent of all gonorrhea in this country” (Altman, 21). Also it is important to note according to the newsletter written in DRUG WEEK on an MMWR Report on Gonorrhea and Chlamydia Incidence among MSM, that gonorrhea or Chlamydia infections can be significant co-factors in the transmission of HIV. This becomes another issue in America as it is the harbor of many homosexuals living in big cities such as San Francisco, Los Angeles, and New York, that such infections can easily be transmitted to many individuals in a very short amount of time. Often drug use is the highest in these areas, which can further cause a much higher incidence rate.
What is being done to address this problem
According to the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report Sexually Transmitted Diseases Treatment Guidelines, 2006, approximately 600,000 new infections of N. gonorrhoeae occur each year in the United States. As the second most commonly reported sexually transmitted disease, a multitude of prevention and treatment strategies have been developed and enforced to control its spread. Due to the fact that the prevalence of N. gonorrhoeae infection varies among communities and populations [1], the basic sociological measures of control include preventative solutions such as: (1) increasing the education and awareness of the N. gonorrhoeae microbe and its resulting gonorrhea infection, (2) openly supporting condom use, (3) encouraging those at-risk be tested, (4) stressing the urgency in seeking treatment if diagnosed and refraining from sexual intercourse until remission, and (5) referring the diagnosed sex partner(s) be tested [2]. At the clinical front, physicians are doing their part to control N. gonorrhoeae transmission by testing all at-risk groups – the highest at-risk group being sexually active women under the age of twenty-five. Other risk factors include previous gonorrhea infection, diagnosis of other sexually transmitted diseases, new or multiple partners, inconsistent-to-no condom use, commercial sex work, as well as drug use. The effective diagnostic tests at which physicians are currently utilizing to test for N. gonorrhoeae include: Gram stain (reserved for symptomatic patients only), culture, nucleic acid hybridization tests, and nucleic acid amplification tests (NAAT). Each requires the testing of cervical, vaginal, male urethral, and/or urine specimens. Fortunately, if a positive test for N. gonorrhoeae results, due to the fact that the microbe is a bacterium, it can easily be treated and cured with antibiotics such as ceftriaxone, cefixime, ciprofloxacin, ofloxacin, or levofloxacin. However, with N. gonorrhoeae’s rising co-infection with uncomplicated C. trachomatis and health officials’ routine approach to co-treat both bacterial infections, an antimicrobial-resistant N. gonorrhoeae strain known as quinolone-resistant N. gonorrhoeae (QRNG) has developed. As a result, common antidotes containing quinolones, such as ciprofloxacin, are inadvisable, especially in the United States. Two states of particular concern are California and Hawaii as they both contain the highest prevalence of QRNG as seen in the Centers for Disease Control and Prevention’s Gonococcal Isolate Surveillance Project 2004 study of 6,322 isolates showing 6.8% resistant to ciprofloxacin. Excluding the isolates gathered from California and Hawaii, only 3.6% were QRNG [1]. Overall, this study’s conclusion is critical as it highlights the competition between aggressively adapting antibiotic-resistant microbes and the scientific discovery of new antibiotics.
What else could be done to address this problem
As antibiotic-resistant strands of N. gonorrhoeae continue to spread throughout the United States, certain antibiotics are increasingly becoming ineffective in treating gonorrhea. Since 1993, fluoroquinones have been used frequently to treat gonorrhea in the United States because it was the overall drug treatment of choice; fluoroquinones were effective as an oral mode of treatment that required only one dose. By 2006, the Center for Disease Control and Prevention (CDC) announced that it no longer recommends fluoroquinones for treatment of gonorrhea because of increasing resistance throughout the United States. Similarly, other antibiotics such as penicillin, tetracycline, and macrolides have not been recommended in the United States because susceptibility to such drugs has been inadequate [1]. Currently, drugs within the cephalosporin class are being used to treat gonorrhea in the United States, but growing resistance and adaptation to antibiotics places heavy emphasis on the development of novel pharmaceuticals for future treatment of gonorrhea. Current research seeks to uncover the genetic and molecular specifics of N. gonorrhoeae, such that particular drugs may be targeted to disrupt it. For example, antigenic variation has been found in N. gonorrhoeae, thus making it hard to develop a vaccine against it [2]. A more recent study has uncovered the molecular basis by which antigenic variation occurs, such that the newly acquired insight may be useful for ongoing pharmaceutical developments against N. gonorrhoeae [3].
Along with novel drugs for treatment, there can also be novel techniques to diagnose individuals with gonorrhea. One such recently developed technique that has been known as the most sensitive and specific test to date for N. gonorrhoeae detection is the nucleic acid amplification test (NAAT)—of which polymerase chain reaction (PCR) falls into categorically. Despite NAAT qualifications, the food and drug administration (FDA) has not cleared the use of such a nonculture test for testing in the rectum and pharynx [4]. Future developments may empirically test the NAAT to ascertain its usefulness for diagnosing such areas, thereby lifting the FDA restriction.
Another mode for preventing further spread of gonorrhea is through the development of more hubs of disease control (e.g., clinics), particularly in metropolitan areas. By constructing more clinics, a more accurate representation of the epidemiology of N. gonorrhoeae may be ascertained. The means by which the United States currently monitors and controls N. gonorrhoeae epidemiology is through the Gonococcal Isolate Surveillance Project (GISP). GISP monitors N. gonorrhoeae prevalence and its susceptibility to antibiotics through sexually-transmitted disease (STD) clinics, regional laboratories, and the CDC itself. It was through GISP that resistance to a fluoroquinone was first identified in 1991. In GISP protocol, a representative subset of the cultures positive for N. gonorrhoeae are tested for antibiotic resistance. As a result, specific antibiotics are prescribed based on demographic and regional data such that treatment remains effective. Currently, approximately 28 cities with STD clinics are part of GISP. With more hubs of disease control, prevention and treatment may be better tailored to regional needs [5].
References
Edited by [Joelle Abed Elahad, Mykel Anderson, Cuong Nguyen, Fisal Mohsini, Danny Huynh, Tim Chiang], students of Rachel Larsen