Livestock Pathogens and Human Consequences: Case Studies of RVF and Maedi Visna
Introduction
By Jack Caine
For thousands of years humans have cultivated animals as companions and food sources. This long-lasting and close relationship, in addition to providing a foundation for human global expansion, has exposed us to many of their pathogens [1]. While these diseases can be quite deadly in their original hosts, the opportunity for a pathogen to be transmitted to a human from an animal increases with duration with them. Zoonoses are any disease that originates in animals and is transmitted to humans [2]. Nearly 60% of known infectious diseases come from zoonotic sources [1]. While zoonoses are not the most common type of disease in humans they do have the capacity to have outbreaks which can result in epidemics or pandemics. Many of the world’s most recent and devastating epidemics and pandemics have resulted from the spillover--the introduction of a novel pathogen into humans from animals--of diseases previously only found in animals. The most well-known of these are the sudden acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) epidemics, the SARS-CoV-2 pandemic, and the ongoing AIDS pandemics [1].
While wild animals are more frequently the source of zoonoses, the animals we have domesticated have their own virulent and devastating diseases [1]
[3]. In addition, these livestock pathogens also cause issues for people because of the significant economic losses they can inflict [4] [5]. This problem is exacerbated when the causative pathogens have no vaccine, or treatment, or are under-researched. This is the case for many neglected tropical diseases (NTD) like Rift Valley Fever virus (RVFV) as well as others like Maedi-Visna virus (MVV). This often gives the
Rift Valley Fever
Virus
Rift Valley Fever is caused by an approximately 100 nm diameter spherical Phlebovirus in the family Bunyaviridae. It has a negative sense RNA genome with three segments, L, M, and S. The large (L) segment codes for the virus’s RNA-dependent RNA polymerase, and the medium (M) segment codes for the glycoproteins that coat the surface of the viral lipid bilayer envelope (Pepin). The small (S) segment is ambisense and codes for two proteins: a nucleoprotein and a virulence factor (Lorenzo). The nucleoprotein (N) aids the RNA-dependent RNA polymerase in transcription and replication of the viral genome. The virulence factor (NSs) plays a significant role in suppressing the innate host immune response (Lorenzo). The NSs factor suppresses the immune system by forming fibrils, clusters of the NSs proteins that appear filamented, which act as a general inhibitor of transcription as well as induce many DNA damage signaling proteins within the cell (Baer). This has the effect of halting the cell cycle, typically in S phase, which allows for greater viral replication (Lorenzo, Baer).
The virus is also an arthropod-borne virus or arbovirus (CDC). For RVF, the virus is vectored by the species in the Aedes and Culex genus. This transmission varies on location but is often spread by the Aedes aegypti mosquito due to the near-global distribution. Additionally, RVFV can be transmitted through the eggs of Aedes aegypti mosquitoes (CDC, Lorenzo). This vertical transmission of the virus from a female mosquito to her offspring plays a significant role in the persistence of the virus. In this way, the mosquito acts not just as a vector of the virus, but also as a reservoir host and can maintain the presence of the virus in the absence of mammals to infect. Additionally, when there are floods, and female Aedes mosquitoes have more opportunities for egg-laying, there are many more cases of RVF in animal and human populations because there is an influx of RVFV positive mosquitoes (CDC). The virus can also be spread between animals in contaminated body fluids. These two modes of transmission, by mosquito vector and bodily fluid exposure, contribute to human exposure to the virus.
Animal Health
Symptoms
Rift Valley Fever is an endemic disease in much of sub-saharan Africa as well as Egypt, Saudi Arabia and Yemen. It is caused by the Rift Valley Fever virus (RVFV) and causes hemorrhagic fever. It typically causes nonspecific symptoms but can cause significant morbidity and mortality in sheep and goats (Merck manual). When symptoms do show they present as a biphasic fever of up to 108 degrees F (42 degrees C), malaise and sluggishness, as well as hematemesis, hematochezia, and nasal discharge. The most severely affected individuals are young goats (kids), lambs, and pregnant ruminants (Merck). In kids and lambs the mortality rate is between 70-100% (WOAH). In the adults of the same species the mortality rate is lower, around 10-30%. Cows and calves are affected similarly. Calves infected with RVFV can have mortality rates as high as 70%, with mature individuals experiencing a mortality rate of 5-10%. However, recorded rates of abortion in ewes is as high as 100% whereas sows consistently abort in greater than 10% of cases ( Chengula, Merck).
Diagnosis
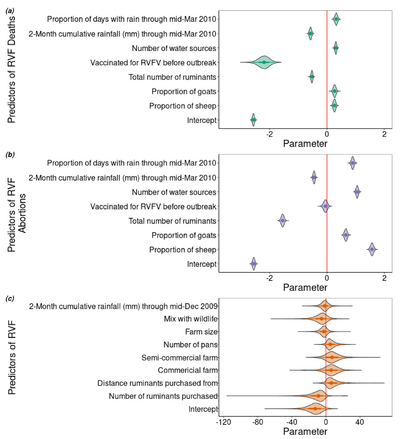
Because the disease is nonspecific, conditional factors can often give an indication that there is an outbreak of RVF. Factors like heavy rainfall, and large mosquito populations act as predictors for outbreaks (figure 4) and significant abortions post infection can be a sign that there is a current outbreak ( Chengula, Merck). Tissues from recently aborted fetuses from cattle or sheep contain high titers of the virus and can be used for its isolation. Serum or whole blood samples from animals in the febrile stage of the disease can also be readily used for viral isolation. However, the procedures for viral isolation are slow and expensive so new technologies were vital to accommodate the need for rapid assessment of RVF infection (pepin). This came in the form of real-time reverse-transcription loop mediated isothermal amplification assays (RT-LAMP). These RT-LAMP assays had the benefits of high diagnostic accuracy within 30 minutes and are manufactured with relatively inexpensive materials, making it a promising diagnostic tool not only for global health NGOs but also for the people who raise livestock.
Treament and Prevention
There is no current treatment for animals with RVF leaving vaccination as the only broadly applicable prevention strategy. There have been several vaccines developed which have seen varying levels of success. The earliest vaccine for RVF was developed in 1949 and is still used today, although its use of a modified live vaccine (Smithburn) retains some virulence and is known to induce abortions and does not produce sufficient antibody response in cattle (pepin, Merck). More recent attempts at a vaccine have proved promising with a live-attenuated vaccine recently being approved in South Africa and some recombinant vaccines expressing the RVFV surface glycoproteins are in development (CDC, Pepin Merck). However, in most places, RVF does not have long lasting endemic infection and so vaccines are used as an emergency measure in the event of an outbreak (Merck).
Human Health
Transmission
People most often infected with RVF get it from exposure to infected livestock, although some transmission via mosquitoes does occur (WHO). This spillover can occur anytime infected fluids can enter the human body. Infection can happen through cuts on hands or arms from contaminated fluid that splashes a person during births, butchering, or veterinary procedures. The virus can also travel in aerosols which a person from a sick animal can inhale. Given the multitude of ways that RVF can pass from animals to humans, it is important to note that there have been no cases of human-to-human transmission of the virus.
Symptoms
RVF is a generally mild disease in humans with an incubation period of 2-6 days. Typically, people are asymptomatic or have a mild illness frequently including flu-like symptoms such as fever, muscle pains, nausea or vomiting. In less than 10% of people, the disease can progress and present as one of 3 forms: ocular form, meningoencephalitis form, or a hemorrhagic fever form. Both the ocular presentation and the meningoencephalitis presentation occur 1-4 weeks after infection. People who contract the ocular form will have 10-12 weeks of vision impairment and half will have permanent blindness (WHO, CDC). The second form can lead to severe headaches, and brain damage which is rarely fatal but causes lifelong neurological defects (CDC, WHO). In less than 1% of patients, the hemorrhagic fever form of the disease has a fatality rate of 50% after 3-6 days due to the blood loss that occurs. In all recorded human cases of RVF, only about 1% of people have died (WHO).
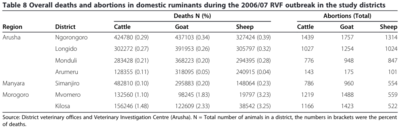
Economic Impact
RVF outbreaks in Africa are sporadic and generally isolated but can cause significant losses to the people who raise and work with livestock and animal products. These losses can take years to recover from, and extend beyond losing numbers of sheep, cattle or goats. In the 2010 South African outbreak of RVF the sheep farmers lost an estimated 10 million USD worth of livestock (Mdlulwa and Ngwane). Earlier, the 2007 RVF outbreak in Kenya cost the nation and its farmers close to 32 million USD (Rich and Wanyoike).
Maedi-Visna
Include some current research, with at least one figure showing data.
Virus
Animal Health
Economic Impact
Human Health
Solutions
Include some current research, with at least one figure showing data.
Section 4
Conclusion
At right is a sample image insertion. It works for any image uploaded anywhere to MicrobeWiki.
The insertion code consists of:
Double brackets: [[
Filename: PHIL_1181_lores.jpg
Thumbnail status: |thumb|
Pixel size: |300px|
Placement on page: |right|
Legend/credit: Magnified 20,000X, this colorized scanning electron micrograph (SEM) depicts a grouping of methicillin resistant Staphylococcus aureus (MRSA) bacteria. Photo credit: CDC. Every image requires a link to the source.
Closed double brackets: ]]
Other examples:
Bold
Italic
Subscript: H2O
Superscript: Fe3+
Sample citations: [6]
[7]
A citation code consists of a hyperlinked reference within "ref" begin and end codes.
To repeat the citation for other statements, the reference needs to have a names: "<ref name=aa>"
The repeated citation works like this, with a forward slash.[6]
References
- ↑ 1.0 1.1 1.2 1.3 Qiu, Y. et al., "Global prioritization of endemic zoonotic diseases for conducting surveillance in domestic animals to protect public health." 2023. Phil. Trans. R. Soc. B 378.
- ↑ Quammen, David. "Spillover: animal infections and the next human pandemic." 2012. W.W. Norton & Company.
- ↑ Minardi da Cruz, et al., "Small Ruminant Lentiviruses (SRLVs) Break the Species Barrier to Acquire New Host Range" 2013. Viruses 5:1867-1884.
- ↑ Kalogianni et al.: Etiology, Epizootiology and Control of Maedi-Visna in Dairy Sheep: A Review. 2020. Animals 10:616.
- ↑ 5.0 5.1 Chengula et al.: "Socio-economic impact of Rift Valley fever to pastoralists and agro pastoralists in Arusha, Manyara and Morogoro regions in Tanzania" 2013. SpringPlus 2:549.
- ↑ 6.0 6.1 Hodgkin, J. and Partridge, F.A. "Caenorhabditis elegans meets microsporidia: the nematode killers from Paris." 2008. PLoS Biology 6:2634-2637.
- ↑ Bartlett et al.: Oncolytic viruses as therapeutic cancer vaccines. Molecular Cancer 2013 12:103.
Authored for BIOL 238 Microbiology, taught by Joan Slonczewski,at Kenyon College,2024