Quorum Sensing in Staphylococcus aureus Infections
Introduction to Staphylococcus aureus
By Elizabeth Eder
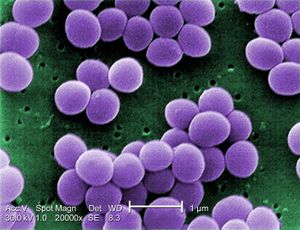
Staphylococcus aureus is a gram-positive cocci-shaped bacterium that commonly colonizes human epithelia. Epithelial surfaces include the skin and respiratory tract, and in these areas S. aureus is considered a natural component of the human microbiome and does not serve as a benefit or detriment to its human host. First identified in 1880, S. aureus is a facultative anaerobe, meaning it generates ATP with or without oxygen. While S. aureus is not naturally pathogenic on epithelial surfaces, infections can occur in these areas and range from pimples and impetigo to pneumonia and meningitis. Pathogenicity can develop through the infection of S. aureus in the bloodstream, and these infections are of great medical relevance due to their prevalence and virulence. Infections can be community-acquired (CA) or hospital-acquired (HA), with the latter illustrating the challenge of sterility in healthcare settings.
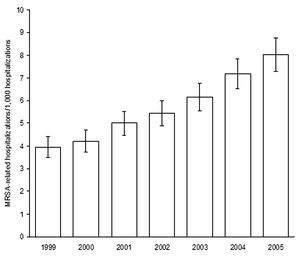
Compounding the issue of infection is the bacteria’s ability to develop drug resistance, resulting in strains such as methicillin-resistant Staphylococcus aureus (MRSA). These strains have been of increasing concern in the medical field for their persistence in nosocomial infections and comprise the majority of S. aureus infections (Boucher). The frequency of S. aureus infections, and the frequency of those infections acquiring methicillin-resistance, is increasing in hospitals in the U.S. The CDC reported a 62% increase in S. aureus-related hospitalizations from 1999 to 2005, and suggested that MRSA be considered “a national priority for disease control.” Understanding the molecular mechanism of virulence is critical for addressing the issue of S. aureus and MRSA infections, because the resistance that S. aureus develops seriously limits antibiotic usefulness. Despite the advances in patient care, technology, and heath environment sterility, S. aureus infections continue to be an issue in U.S. hospitals and communities. One mechanism of S. aureus that is currently being studied for its potential contribution to pathogenicity is the quorum sensing (QS) system of communication.
Medical Relevance and MRSA

Staphylococcus aureus can become pathogenic whether or not it develops antibiotic resistance, but cases where strains do become resistant are of great concern for the morbidity and mortality associated with them. The economic costs infections impose on hospitals are also serious and significant. S. aureus isolates that do begin to acquire antimicrobial drug resistance are usually resistant to methicillin and other beta-lactam drugs, but progress through a series of stages prior to complete resistance. Isolates are initially considered susceptible, and then progress to intermediate, and finally resistant.
Staphylococcus aureus infections can be categorized into five main types: localized skin infection, diffuse skin infection, deep localized infections, toxinoses, and other infections. Localized skin infections can result in cutaneous or subcutaneous abscesses and possibly bacteremia. Bacteremia is the infection of bacteria in the blood, which is normally a sterile and bacteria-free environment. When bacteria such as S. aureus are found in the blood, intravenous antibiotics are used as treatment to prevent further spread from the blood into the heart endocardium or bone marrow. Diffuse skin infections include impetigo, which results in facial sores and blisters and is also treated with antibiotics. Deep localized infections include infection of bone and bone marrow, called osteomyelitis, as well as septic arthritis. Toxinoses include toxic shock syndrome and gastroenteritis, but are not necessarily caused by bacterial infection but by bacterial toxins. S. aureus produces toxins that can lead to toxinosis when ingested. The other infections S. aureus can cause include endocarditis, pneumonia, and other inflammatory responses.
Antibiotics used to treat MRSA are vancomycin, linezolid, teicoplanin, tigecycline, daptomycin, and telavancin. Vancomycin remains the most common, though different studies investigating each antibiotic have revealed pros and cons to each. The over-prescription and over-use of antibiotics has been controversial in aiding the progression of multiple species of bacteria towards antibiotic resistance, and as strains continually develop less susceptibility newer antibiotics with different antimicrobial targets are in demand. In healthcare settings infections by both S. aureus and MRSA have increased over 1999-2005 as reported by the CDC. S. aureus-related infections in the U.S. increased from 294,570 to 477,927 and of those totals the number of MRSA infections increased from 127,036 to 278,203. Resistance to ampicillin, cephalothin, and erythromycin also increased over that period of time.
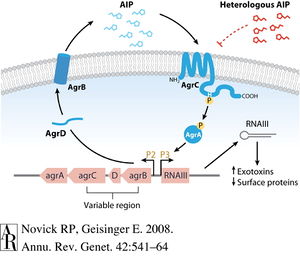
Quorum Sensing System
Include some current research, with at least one figure showing data.
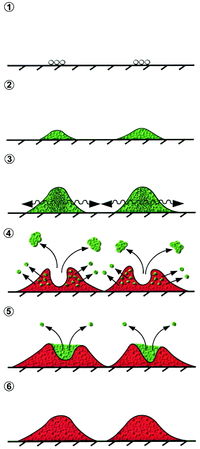
QS and Pathogenicity
Include some current research, with at least one figure showing data.
Infection Prevention and Treatment
References
[1] Boucher, HW and Corey, GR (2008) Epidemiology of methicillin-resistant Staphylococcus aureus. Clinical Infectious Diseases 46:344-349.
[2] Haddadin, AS, Fappiano, SA, Lipsett, PA (2002) Methicillin resistant Staphylococcus aureus (MRSA) in the intensive care unit. Postgrad Med J 78:385-392.
[3] Novick, RP and Geisinger, E (2008) Quorum sensing in Staphylococci. Annu Rev Genet 42:541-564.
[4] Yarwood, JM, Bartels, DJ, Volper, EM, Greenberg, EP (2004) Quorum sensing in Staphylococcus aureus biofilms. J Bacteriol 186:1838-1850.
[5] Periasamy, S, Joo, H, Duong, AC, Bach, TL, Tan, VY, Chatterjee, SS, Cheung, GY, Otto, M (2011) How Staphylococcus aureus biofilms develop their characteristic structure. PNAS 109:1281-1286.
[6] Rutherford, ST and Bassler, BL (2012) Bacterial quorum sensing: its role in virulence and possibilities for its control. Cold Spring Harb Perspect Med 2:a012427.
[7] Yarwood, JM, Schlievert, PM (2003) Quorum sensing in Staphylococcus infections. J. Clin. Invest. 112:1620-1625.
[8] Klein, E, Smith, DL, Laxminarayan, R (2007) Hospitalizations and deaths caused by methicillin-resistant Staphylococcus aureus, United States, 1999–2005. Emerg Infect Dis 13(12):1840-1846.
[9] Kiran, MD, Adikesavan, NV, Cirioni, O, Giacometti, A, Silvestri, C, Scalise, G, Ghiselli, R, Saba, V, Orlando, F, Shoham, M, Balaban, N (2008) Discovery of a quorum-sensing inhibitor of drug-resistant staphylococcal infections by structure-based virtual screening. Mol Pharmacol 73:1578-1586.
Authored for BIOL 291.00 Health Service and Biomedical Analysis, taught by Joan Slonczewski, 2016, Kenyon College.
