Rickettsia rickettsii: Difference between revisions
| Line 58: | Line 58: | ||
==Pathology== | ==Pathology== | ||
Typical symptoms of RMSF can appear 2 to 14 days after exposure and include fever, headache, depression, nausea, vomiting, and gradually may develop a skin rash called purpura or petechiae. Sometimes the rash occurs 2 to 5 days after the onset of the fever. Serious cases of RMSF can include central nervous system, pulmonary, or hepatic injuries. Patients that had compromised immune | Typical symptoms of RMSF can appear 2 to 14 days after exposure and include fever, headache, depression, nausea, vomiting, and gradually may develop a skin rash called purpura or petechiae. Sometimes the rash occurs 2 to 5 days after the onset of the fever. Serious cases of RMSF can include central nervous system, pulmonary, or hepatic injuries. Patients that had compromised immune systems often had an increased susceptibility to other infections. [2][9] | ||
Rickettsia Rickettsii can infect endothelial cells within the human body through the vascular smooth muscle cells. [5] In addition, it is an intracellular pathogen that can infect and multiple within the nucleus or cytosol of endothelial cells of the blood vessels. [9] | Rickettsia Rickettsii can infect endothelial cells within the human body through the vascular smooth muscle cells. [5] In addition, it is an intracellular pathogen that can infect and multiple within the nucleus or cytosol of endothelial cells of the blood vessels. [9] | ||
Revision as of 05:35, 28 August 2007
A Microbial Biorealm page on the genus Rickettsia rickettsii
Classification
Higher order taxa
Bacteria; Proteobacteria; Alpha Proteobacteria; Rickettsiales; Rickettsiaceae; Spotted fever group
Species
|
NCBI: Taxonomy |
Rickettsia rickettsii
Other Names
synonym: Dermacentroxenus rickettsii
synonym: "Dermacentroxenus rickettsii" Wolbach 1919
synonym: Rickettsia rickettsii (Wolbach 1919) Brumpt 1922
Description and significance
Rickettsia rickettsii is a small, rod-shaped bacterium known to cause Rocky Mountain spotted fever (RMSF). This disease can be transmitted to humans either from a tick bite with an incubation period of 1 week, or by contamination of a cut on the skin or a wound with ticks feces. Dr. Ricketts first isolated this microbe in Montana, 1906. Rickettsia need host cells to be able to grow. In addition, they also require arthropods as vectors; therefore, ticks are the vectors, or vehicles used for Rickettsia rickettsii. [2] [4] [6]
Describe the appearance, habitat, etc. of the organism, and why it is important enough to have its genome sequenced. Describe how and where it was isolated. Include a picture or two (with sources) if you can find them.
Genome structure
Genes: 1311
Length: 1,257,710 nt
Protein coding: 1311
Structural RNAs: None
GC Content: 32%
% Coding: 77%
Pseudo genes: None
Topology: other
Molecule: DNA
Completed 02/06/2004[3]
Describe the size and content of the genome. How many chromosomes? Circular or linear? Other interesting features? What is known about its sequence? Does it have any plasmids? Are they important to the organism's lifestyle?
Cell structure and metabolism

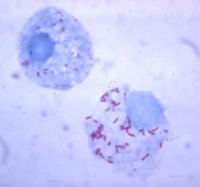
The Rickettsia rickettsii bacterium are intracellular organisms, and they live in the cytoplasms of host cells sometimes in the nucleus. They are adapted as intracellular organisms because they have transport systems and metabolic enzymes. These microbes divide by binary fission and take about 8 hours to double. [2]
Rickettsia rickettsii are similar to small, gram-negative nods. They are barely visible under a light microscope, and they stain poorly with Gram stains. The cell wall is made up of peptidoglycan, lipopolysaccharide, and a cell membrane. These microbes contain two outer membrane proteins, outer membrane protein A (OmpA) and outer membrane protein B (OmpB). OmpA sticks to the host cell wall, and it is a protective layer of about 190 kDa. It contains a region of 13 identical repeating units that include antigenic function. OmpB is an abundant outer membrane protein that contains sequences related to the typhus group of rickettsiae.[2][7]
Describe any interesting features and/or cell structures; how it gains energy; what important molecules it produces.
Ecology
Rickettsia rickettsii can be found in the western hemisphere, more notably in North America and South America. In North America, it’s more well known in the southeast and southcentral states. In North America, Rickettsia rickettsii is transmitted by the American dog tick (Dermacentor variabilis) and the Rocky Mountain wood tick (Dermacentor andersoni). In Latin America. In Latin America, Rickettsia rickettsii is transmitted by Rhipicephalus sanguineus and the Cayenne tick Amblyomma cayenne. [9]
Describe any interactions with other organisms (included eukaryotes), contributions to the environment, effect on environment, etc.
Pathology
Typical symptoms of RMSF can appear 2 to 14 days after exposure and include fever, headache, depression, nausea, vomiting, and gradually may develop a skin rash called purpura or petechiae. Sometimes the rash occurs 2 to 5 days after the onset of the fever. Serious cases of RMSF can include central nervous system, pulmonary, or hepatic injuries. Patients that had compromised immune systems often had an increased susceptibility to other infections. [2][9]
Rickettsia Rickettsii can infect endothelial cells within the human body through the vascular smooth muscle cells. [5] In addition, it is an intracellular pathogen that can infect and multiple within the nucleus or cytosol of endothelial cells of the blood vessels. [9]
How does this organism cause disease? Human, animal, plant hosts? Virulence factors, as well as patient symptoms.
Application to Biotechnology
Does this organism produce any useful compounds or enzymes? What are they and how are they used?
Current Research
Currently there is a major lack in controlling the RMSF organism. In addition, an effective diagnostic test to detect early symptoms is still not available. Doctors have a hard time detecting RMSF because the patients rarely have the Rickettsia rickettsii antibodies. Although PCR (Polymerase Chain Reaction) testing is available in a few laboratories, detection of Rickettsia DNA in the blood is still tactless, especially in the early symptoms. After diagnosis with RMSF, it is usually treated with Tetracycline unless the CNS has already been affected thereby using Chloramphenicol instead.[8] [9]
Enter summaries of the most recent research here--at least three required
References
1) NCBI Taxonomy Browser "Rickettsia Rickettsii" Retrieved 26 August, 2007
2) Primary Care Update for OB/GYNS, Volume 9, Issue 1, January-February 2002, Pages 28-32 Whitney Jamie
3)http://www.ncbi.nlm.nih.gov/sites/entrez?Db=genome&Cmd=ShowDetailView&TermToSearch=5211
4) http://jmm.sgmjournals.org/cgi/content/full/56/1/138
6) Phylogenetic analysis of the genus Rickettsia by 16S rDNA sequencing Research in Microbiology, Volume 146, Issue 5, June 1995, Pages 385-396 V. Roux and D. Raoult
7) Comparison of the rompA gene repeat regions of Rickettsiae reveals species-specific arrangements of individual repeating units Gene, Volume 125, Issue 1, 15 March 1993, Pages 97-102 R. D. Gilmore
8) http://www.cdc.gov/ncidod/eid/vol12no04/05-1282.htm
9) Transfusion-transmitted tick-borne infections: A cornucopia of threats Transfusion Medicine Reviews, Volume 18, Issue 4, October 2004, Pages 293-306 David A. Leiby and Jennifer E. Gill
Edited by Amber Chou; student of Rachel Larsen
