Skin: Difference between revisions
| Line 1: | Line 1: | ||
== | ==Introduction== | ||
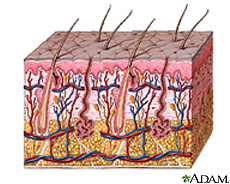
The skin is an organ that contributes to several different epithelial systems as it represents the largest interface between the internal environment of humans and the external world [1,2]. With a mass of approximately five kilograms and it's most superficial layer, known as the stratum corneum, having a surface area generally in the range of 1.75 square meters; the skin is also the largest organ of the human body [1,2]. The skin serves a number of key functions, with its most basic purposes surrounding its role as a physical barrier protecting the host's internal environment from external pathogens, as well as osmo- and thermoregulation. | The skin is an organ that contributes to several different epithelial systems as it represents the largest interface between the internal environment of humans and the external world [1,2]. With a mass of approximately five kilograms and it's most superficial layer, known as the stratum corneum, having a surface area generally in the range of 1.75 square meters; the skin is also the largest organ of the human body [1,2]. The skin serves a number of key functions, with its most basic purposes surrounding its role as a physical barrier protecting the host's internal environment from external pathogens, as well as osmo- and thermoregulation. | ||
Revision as of 14:34, 29 August 2008
Introduction
The skin is an organ that contributes to several different epithelial systems as it represents the largest interface between the internal environment of humans and the external world [1,2]. With a mass of approximately five kilograms and it's most superficial layer, known as the stratum corneum, having a surface area generally in the range of 1.75 square meters; the skin is also the largest organ of the human body [1,2]. The skin serves a number of key functions, with its most basic purposes surrounding its role as a physical barrier protecting the host's internal environment from external pathogens, as well as osmo- and thermoregulation.
The microbial fauna colonizing the skin of a healthy human possess a wide and varying lexicon that is distributed across the body in a manner largely dependent on the environmental conditions specific to distinct regions of skin. Important qualities to note that effect the identity of colonizing bacteria include include moisture, carbohydrate content, temperature, and pH. Generally speaking, three categorical regions of human skin have been identified, with the driest and most basic area being the upper arms and legs; the moistest and most acidic area being the axilla and toewebs; and the area falling in between these two extremes being the face and hands.
DESCRIPTION OF THE SKIN
Location and Significance
The skin’s key role as the physical barrier delineating between the bloodstream and external environment carries many responsibilities. The dermal epithelium is charged with preventing excess water loss, controlling and maintaining its own plasticity and elasticity, and protecting against UV radiation; but also must integrate all these duties in such a way that provides a barrier against the natural microbial proclivity of pathogens to seek out and colonize the skin’s nutrient-rich environment. (Elias, Feingold, 363?)
While there is some consistency in the microbial biodiversity across all regions of skin, there are considered to be three general regions of skin that distinguish the specific bacterial flora observed there upon. These regions are (1) the axilla and toewebs; (2) the hands and face; and (3) the upper arms, legs, and trunk. These anatomical distinctions in microbial biodiversity are products of their physical conditions -- specifically, their variation in pH, moisture, body temperature, and concentrations of skin lipids are of particular importance.
Skin epithelium functions to keep microbes off the rest of the body by:
- Acting as a physical barrier against microbe penetration to tissues underneath [2]
- Secreting a mucus layer so that microbes can not permanently attach to the epithelial cells beneath [2]
- Shedding or keratinization of the outermost skin cells so microbes are removed from the body [2]
- Secreting antimicrobial peptides and proteins to kill off microbes or at least prevent their growth [2].
Physical Conditions of the Skin
The composition of the skin’s most superficial layers is such to optimize its capacity to prevent bacterial growth on its surface. Examples of this can be found in its relatively high temperature, low carbohydrate and water content, acidic pH, and antimicrobial peptide activities.
The acidic quality of the skin plays an important role in combating bacterial growth. The skin’s pH generally fluctuates between 5.6 and 6.4 depending on the region of the body it is covering, establishing an environment that few species of bacteria are capable of proliferating in. The skin’s acidity results from lactic acid from its own keratinocytic biproducts, amino acids from sweat, the fatty acids from sebum; as well as the metabolites of the rare microbes capable of colonizing its various surfaces [1]. Although the skin is acidic, it is only suitable for neutrophile growth and not acidophiles or alkaliphiles [1].
The temperature of the skin varies depending on the location on the body. Toes and fingers tend to have the lowest temperatures, while the axillae and the groin tend to have the highest [1]. The temperatures are usually 25-35 degrees Celsius, which is ideal for mesophiles rather than thermophiles or psychrophiles [1]. The temperature only varies slightly so it there is not a dramatic selection for microbes colonizing certain areas, but does affect the growth rate of the microbes present [1].
The moisture content on the skin is generally low, which limits the survival and growth of microbes. However, the eccrine glands can produce sweat that increases moisture on the surface of the skin, and can be of particular metabolic value to bacteria in areas where evaporation does not occur easily, such as the toes and axillae [1]. Microbes tend to have greater populations in those occluded areas since there is an accumulation of secretions[1].
The skin generally has a high oxygen concentration, so it acts primarily as an aerobic environment for anaerobes to grow [1]. However, the hair follicles inside the skin provide a microaerophillic and/or anaerobic environment that have lower levels of oxygen, so that microaerophiles and obligate anaerobes can also grow [1].
Influence by Adjacent Communities
The skin is always exposed to the external environment. Ecological factors such as climate and habitat have great influence on the microbial flora that colonize the skin. Generally speaking, gram-negative bacilli more frequently colonize regions of the skin with higher moisture content or partial occlusion. Contact with dirt, for example, can introduce non-indigenous or harmful microbes onto the skin. Even air can influence the microbe communities by preventing the airborne microbes from settling on the skin [2]. The openings of the host’s body such as the nose, mouth, urethra, and rectum can also introduce microbes from those regions on to the skin [2].
Conditions Causing Environment Changes
Do any of the physical conditions change? Are there chemicals, other organisms, nutrients, etc. that might change the community of your niche.
Variations in the amount or concentration of sebaceous and sudoriferous glands can affect the skin's temperature, water content, concentration nutrients, osmolarity, pH, and concentration of antimicrobial substances [2]. This is because sebaceous glands are major sources of nutrients for microbes, while the sudoriferous glands produce sweat as a source of water on the skin [2]. Both glands also produce antimicrobial substances important to the skin [2].
Clothing, air-conditioning, or housing, for example, can be considered forms of protection against extreme environments. However, the conjunctiva and exposed regions of the skin have greater fluctuations in temp, humidity, and so forth, in comparison to other bodily systems [1]. Covering areas of the skin, for instance, can prevent the evaporation of water and encourage a build up of secretions and alter the pH [2].
Even host characteristics such as age, gender, host’s nutrition, stress, emotional state, disability, hospitalization, personal hygiene, lifestyle, occupation, living conditions, and so on can affect the skin environment[1].
BACTERIAL INHABITANTS OF THE THREE CATEGORICAL REGIONS OF SKIN
Microbes are described as “nonpathogenic” if they demonstrate limited growth on the epithelial surface, while those that can invade and have the potential to reach levels of unrestrained growth are defined as “pathogenic” (Elias, Feingold, 363?). The majority of the microorganisms that live in the epidermis live in its most superficial layer, known as the stratum corneum, while there are certain species of bacteria that reside in the more secluded areas of follicular canals.
Axilla and Toewebs: Corynebacterium
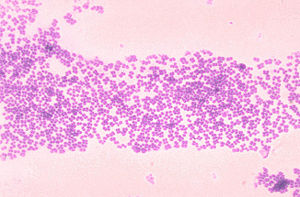
Corynebacterium is a microbe ofter found on the skin and is classified as a coryneform. This means that it is non-branching, not-sporing, non-acid-fast, gram-positive, nonmotile and aerobic.
Corynebacteria can grow at temperatures ranging from 15 to 40 degrees Celsius, but have the best growth at 37 degrees. They are also halotolerant and can grow at NaCl concentrations of up to 10 percent. Because of this, they able to live on locations of the skin with high salt content such as the axillae and in between the toes. These areas are somewhat occluded and therefore have a higher moisture and temperature. These conditions make corynebacteria more prevalent in these regions of the skin. They are found on the skin throughout the body such as the head, arms, legs and hands, but are more prevalent on the lower half.
They are able to use both carbohydrates and amino acids as carbon and energy sources. These macronutrients are readily available in sweat. Glucose is obtained through the hydrolysis of glycoproteins, whereas amino acids are obtained from the hydrolysis of proteins. These amino acids are required for growth. Lipophilic corynebacteria also need other nutrients which they obtain from sweat. These nutrients include riboflavin, thiamine, biotin, nicotinamide, and pantothenate. (1)
Corynebacteria provide the environment that allows other bacteria to grow. They are able to hydrolyze urea to NH4, which provides a nitrogen source for most cutaneous microbes. At the same time they are dependent on other microbes such as Staphylococcus and Propionibacterium. These types of bacteria provide fatty acids which they obtain from lipids. And in this way they have a complex relationship with these other organisms.(1)
Corynebacterium make up 19% of microbes found on the human skin. And the frequency of detection is much higher in the month of May than in any other time of the year. This is probably due to the increase in average temperature from 8.2 to 16.5 degrees Celsius.(1) Some species of Corynebacterium, such as Corynebacterium diphtheriae and Corynebacterium ulcerans, are capable of causing skin lesions.(3) These ulcers are often co-infected with Staphylococcus aureus and group A streptococci. These infections can spread to other areas of the body causing pharyngeal infections.(2) Other species like, Corynebacterium tenuis are the cause for trichomycosis axillaris. This is a colonization of the hair shaft in sweat glands in areas such as armpits and pubic area.(5) It consists of a tightly packed overgrowth of this microbe.(6)
Microbial Interactions of Corynebacterium and its Effects on the Dermal Environment
Corynebacteria provide the environment that allows other bacteria to grow. They are able to hydrolyze urea to NH4, which provides a nitrogen source for most cutaneous microbes. At the same time they are dependent on other microbes such as Staphylococcus and Propionibacterium. These types of bacteria provide fatty acids which they obtain from lipids. And in this way they have a complex relationship with these other organisms.(1)
Corynebacterium make up 19% of microbes found on the human skin. And the frequency of detection is much higher in the month of May than in any other time of the year. This is probably due to the increase in average temperature from 8.2 to 16.5 degrees Celsius.(1) Some species of Corynebacterium, such as Corynebacterium diphtheriae and Corynebacterium ulcerans, are capable of causing skin lesions.(3) These ulcers are often co-infected with Staphylococcus aureus and group A streptococci. These infections can spread to other areas of the body causing pharyngeal infections.(2) Other species like, Corynebacterium tenuis are the cause for trichomycosis axillaris. This is a colonization of the hair shaft in sweat glands in areas such as armpits and pubic area (5). It consists of a tightly packed overgrowth of this microbe (6).
Hands and Face: Propriobacterium acnes
Propionibacterium acnes, named for its production of propionic acid, is a commensal gram positive bacterium, found in the sebum produced by sebaceous glands in the skin . It is aerotolerant, allowing it to grow in aerobic conditions but preferring anaerobic fermentation . It tends to grow on hair follicles where there are reduced levels of oxygen and in areas with aerobic organisms that consume oxygen from their immediate environment . Its optimal temperature is 37*C, optimal pH 5.5-6.0. P. acnes is sensitive to UV irradiation but is increasingly antibiotic resistant. It metabolizes fatty acids and sebaceous fluid secreted by the pores they reside in. The products of its fermentation of free short-chained fatty acids assist in its colonization on hair follicles. In addition, they also synthesize proteases, which kill staphylococci and others of the Propionibacteria species. The propionic and acetic acid that it produces are also seen to inhibit growth of other microbial species found in its environment. Although there is no direct benefit to our human skin in harboring such a bacterium, its existence prevents possible onset of more dangerous pathogens, as the worst pathogenic consequences it can bring about are painful lesions and disfiguring acne scars. Its presence occupies the skin such that no dangerously pathogenic microbes can do it harm.
Microbial Interactions
Little beneficial interactions are seen among skin microbes; usually, they are rather antagonistic. However, a beneficial interaction is seen with P. acnes. As one of the more predominant cutaneous microbes, its existence depends on aerobic microbes, including Corynebacterium jeikeium and Acinetobacter, and facilitative microbes, such as staphylococci and Dermabacter hominis, for these microbes consume oxygen and provide P. acnes with their ideal atmosphere to flourish. Without these aerobic and facilitative microbes, they are unable to grow in an aerobic environment. In turn, P. acnes provide other microbes like micrococci and Brevibacteria with propionic and acetic acids, used as carbon sources. Additionally, the bacteria requires vitamins for growth, including biotin, nicotinamide, pantothenate, and thiamine. Other examples of beneficial interactions include staphylococci producing lactate that is used as a carbon source for Actinobacteria and keratin hydrolysis that produces amino acids used by staphylococci, micrococci, and Brevibacterium.
Effects of P. acnes on the Dermal Environment
Although normally nonpathogenic, P. acnes paves the way for opportunistic pathogens to generate infections. Like most of the skin’s normal flora, it does not pose as a threat until the skin is compromised. An accumulation of P. acnes in sebum-rich areas is implicated in the onset of acnes vulgaris, a skin condition affecting 80% of adolescents in America. P. acnes can bind to oleic acid, which is a major component of sebum. Oleic acid, in turn, promotes co-aggregation, of the organism. This co-aggregation, along with the interaction of the microcolony with oleic acid, would help maintain the organism in the habitat; in this case, hair follicles. Sebum is normally excreted through pores of the skin. Acne, characterized by inflamed lesions, results when sebum and oil builds up under the skin and is further blocked by blackheads.
Though not a direct cause of acnes vulgaris, the presence of P. acnes certainly aids in its onset. Research shows that an acnes inflammation is deemed less severe after treatment with antibiotics that target P. acnes, although P. acnes is becoming increasingly antibiotic resistant. The putative genome of P. acnes has 2333 genes encoding metabolic products including the degradative enzyme lipase that damages host tissue, as well as the heat shock protein that induces an immune response that triggers inflammation. Lipases can also digest excess skin oil and sebum in regions that contain hair follicles and sebaceous glands. Blocked pores create an optimal anaerobic condition for P. acnes to thrive. As P. acnes proliferate in excess, their metabolic products overwhelm the cell wall such that it is ruptured open and a bacterium, such as S. aureus, can cause irritated lesions.
Upper Arms, Legs, and Trunk: Micrococcus luteus
Micrococcus luteus is the most common bacteria of the Micrococcus species found on the skin. (**) The bacteria mostly colonize the legs, arms, and head (Kloos* and Musselwhite, 1975). These areas of the body do not hold as much moisture as other areas, like the axilla, which explains how Micrococcus luteus tolerate dry conditions. They are mainly innocuous on the skin, although immunodeficiency in the host, like HIV patients, can lead to infection.
These gram-positive bacteria are tolerant at high salt concentrations. It’s halotolerant up to 7.5% NaCl, which allows it to tolerate the salinity of the skin- note that seawater is 3% NaCl (Wilson, 2005). Sweat and sebaceous glands greatly contribute to the salinity of the skin. Secretions of sweat from sweat glands to the skin are high in salt concentration and low in water. As the amount of sweating increases, the amount of salt reaching the skin’s surface increases too. The evaporation of water from the release of heat enables the salts to remain present on the skin. (Marples, 1965). As a result of these secretions, nutrients and minerals are present for halotolerant bacteria to survive on the skin.
The nutrients utilized by these bacteria are present on the skin environment. Their primary carbon energy source is derived from amino acids available on the skin after being secreted from sweat glands. These amino acids include arginine, cysteine, methionine, tyrosine, making M. luteus one of the most demanding nutritionally bacteria of the skin (Noble, 1993). A secondary energy source is the lactic acid secreted from sweat glands to the skin’s surface, which can be converted to its lactate salt form by other bacteria (Wilson, 2005).
Microbial Interactions of M. luteus
M. luteus can find carbon energy sources from the fermentative products of other dermal-colonizing bacteria. Proprionibacterial species – such as P. acnes – produce proprionate and acetate, which is one such potential source of energy; another example is lactate produced by Staphylococcus species (Wilson, 2005). Lactate may be a nutrient for bacteria as well as a contributor to skin pH. The lactate and lactic acid interconvert and contribute to the buffering of the skin pH balance; amphoteric amino acids also contribute to this buffer (Marples, 1965). As a result, these symbiotic relationships between bacteria are beneficial for providing nutrient sources to each other, allowing many species to inhabit the skin. These bacteria also secrete products to their environment, which keep the skin niche in equilibrium. For example, glycerol is another carbon source used for metabolism in Micrococcus luteus (Wilson, 2005). Lipases are used to degrade oils on the skin into free fatty acids and glycerol. This alcohol generated is metabolized by M. luteus and releases an acid bi-product. Increasing acidity in the environment can contribute to the acidity of the skin pH. This acidity of the skin can be lethal to other microbes that prefer more basic environments. M. luteus therefore contributes to protecting the skin from unwanted microbes by contributing to acidity.
Effects of M. luteus on the Dermal Environment
With the functioning of these enzymes, many amino acids are released into the environment. Itself along with other neighboring bacteria (like Malassezia species, Staphylococcus species, and Brevibacterium species) benefit from the break down of the proteins so it may acquire free amino acids (Wilson, 2005). Some of the products from the breakdown of these nutrients produce rancid odors (Noble, W.C. 1993). For example, the stench of feet is produced by Micrococcus species breaking down nutrients. These smelly compounds are antibacterial to some bacterial species and can prevent other microbes from inhabiting the skin.
NON-BACTERIAL INHABITANTS OF THE SKIN
Genus Fungi, Malassezia globosa of Malassezia (Pityrosporum)
One type of fungi that is normally found on the skin is known as Malassezia globosa. It is one species belonging to the genus Malassezia. It is a lipophilic, dimorphic yeast that is normally present on the healthy skin of humans [1]. It is most commonly found on host’s skin in tropical environments. It utilizes lipids as a source of carbon and energy, since it is not able to ferment sugars [2]. The lipids contain fatty acids, which Mal. globosa can use for growth [1]. Because fatty acids and lipids are required for this yeast, it prefers to colonize in areas of the skin that are rich in sebaceous glands such as the scalp, chest, face, and upper back [1]. The yeasts multiply by budding of a scar at the base of the cell, and occurring as either spherical or cylindrical forms. Normal skin is mostly saprophytic yeast phase in the spherical form on trunk and oval on the scalp. The diseased parasitic mycelial forms occur in short septates of filamentous cell with some branching. Factors like puberty, excessive sweating, warmer season, oil application, malnutrition, and steroids, help in massive growth of the fungus in diseased states. Studies show Malassezia acts as a chemotactic agent for leukocytes inducing inflammation and activation of dermatitis and folliculitis indicating irritant and non-immunogenic stimulant [5]. Although Mal. globosa occurs normally on the skin, it can also play a pathogenic role, which is why it has been associated with skin diseases such as pityriasis versicolor, seborrhoeic dermatitis, and dandruff in addition to atopic dermatitis and folliculitis [1 and 2]. For instance,Pityriasis Capitis, also known as dandruff, is an inflammatory scalp disorder disrupting cohesion on corneocytes. This is a result of toxin production and lipase activity of the yeast, which stimulates host immune response to the yeast’s antigens [6].
Microbial Interactions
Microbial Effects on the Environment
Microbial Interactions
Microbe-microbe interactions on the skin tend to either be beneficial or antagonistic.
- Beneficial interactions between microbes, whether it is commensalism or synerism, exist between many microbes on the skin.
The nutritional web of interactions between the microbes is shown to be simple and it is easy to understand the benefits of other microbes in the niche. For instance, propionibacteria is shown to excrete acids that can be used by micrococci, Acinetobacter spp., and brevibacteria as a source of carbon and energy. Lactate produced by staphylococci can be used as a carbon and energy source for Acinetobacter spp and micrococci as well.
In addition to providing nutritional benefits , interacting microbes can also provide hospitable environments for other microbes. This type of commensalism is shown by Malassezia spp., which metabolizes lauric acid that is toxic to propionibacterim acnes, so that the propionibacterim acnes can survive where lauric acid is plentiful [1].
- Antagonistic substances may be produced by cutaneous microbes for competition against non-indigenous microbes.
- CO2 is produced by many bacteria against dermophyte growth [1]
- Lysozymes are produced by staphylococci which kills micrococci, Brevibacterium spp., and Corynebacterium spp. [1].
- Proteases are produced by P. acnes to kill off other Propionibacterium spp. and staphylococci[1].
- Propionic acid is produced by propionibacteria, which inhibits other species from growing at low pH’s on the skin [1].
- Acetic acid is produced by propionibacteria and Dermabacter hominis to inhibit the growth of other species [1].
- Lactic acid is produced by staphylococci and D. hominis to inhibit the growth of other species [1].
- Bacteriocins are produced by staphylococci, Coryebacterium spp., Propionibacterium spp., Micrococcus spp., and Brevibacterium spp. to inhibit the growth of or kill cutaneous organisms [1].
- Antagonistic substances may be produced by cutaneous microbes for competition against non-indigenous microbes.
Do the microbes change their environment?
Do they alter pH, attach to surfaces, secrete anything, etc. etc.
Microbe Metabolism Affecting the Environment
Do they ferment sugars to produce acid, break down large molecules, fix nitrogen, etc. etc.
- Mal. globosa produces proteases that can break down skin proteins, so that amino acids become available[1]. It can also take more of a pathogenic role by producing toxic metabolites or hydrolases that degrade sebum, freeing fatty acids that came from sebaceous triglycerides, consuming certain saturated fatty acids, and leaving behind the unsaturated fatty acids on the skin which can cause irritation, inflammation, and flaking of the scalp [3].
- Corynebacterium spp., staphylococci, and Brevibacterium spp. produce ureases which can break down urea into ammonium ions as a nitrogen source, which is sued by most cutaneous organisms[1 and 2].
Current Research
Enter summaries of the most recent research. You may find it more appropriate to include this as a subsection under several of your other sections rather than separately here at the end. You should include at least FOUR topics of research and summarize each in terms of the question being asked, the results so far, and the topics for future study. (more will be expected from larger groups than from smaller groups)
Molecular Identification of the Malassezia Species (2008)
Polymerase Chain Reaction has recently been used to distinguish between the species within the genus Malassezia. Previous techniques for identification of the Malassezia species were based on morphological biochemical, and physiological characteristics that were complex and time consuming. PCR provides a fast and simple method of analyzing the internal transcribed spacer, which varies between species of Malassezia, as a means of differentiation. In this study, four particular Malassezia species which include: Mal. globosa, Mal. furfur, Mal. sympodialasis, and Mal. restricta that were isolated from dermatitis infections. The specificity of primers were tested and each species of Malassezia had a specific pair primer. The strains of Malassezia were then put into a PCR assay. PCR was able to distinguish between species that were physiologically similar.. The PCR method provides an efficient identification system of the malassezia species that can be used in routine practices [4].
"A diversity profile of the human skin microbiota" (2008)
By surveying different depths of skin: swab, scrape, and punch biopsy, the skin was tested for the different skin microbiota. Similarities between the human and mouse were found to be the strongest. The human inner elbow was compared to the mouse ear skin, resulting in similarities. Test was done with the help of Polymerase Chain Reaction and the test of 16SrRna (small subunit ribosomal genes- site specific phylogenic relationships). This study of healthy human skin microbiota can help determine the complex physiological interactions between the skin and the microbes that inhabit this environment [7].
References
1. Wilson, Michael. Bacteriology of Humans: an Ecological Perspective. Blackwell Publishing, 2008.
2. Wilson, Michael. Microbial inhabitants of Humans: Their Ecology and Role in Health and Disease. Cambridge University Press, 2005.
5. Inamadar AC, Palit A. "The genus Malassezia and human disease." Indian J Dermatol Venereol Leprol [serial online] 2003 [cited 2008 Aug 26];69:265-70. Available from: http://www.ijdvl.com/text.asp?2003/69/4/265/4990
Edited by Patrick A. McGhee, Susan Lin, Eric Pham, Pavithra Ramasubramanian, Deeba Pourmand, ____________________________________, students of Rachel Larsen
