Staphylococcus aureus: Evasion of neutrophils
Introduction
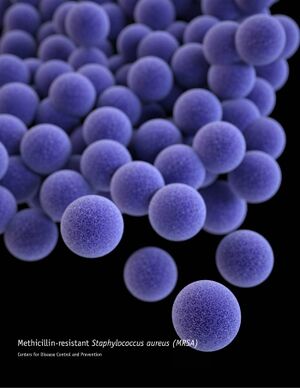
Staphylococcus aureus (S. aureus), also known as “golden staph” and “oro staphira", is a member of Bacillota. Staphylo meaning grape in Greek and aureus meaning golden, indicating S. aureus is a kind of yellow-colored, grapelike-cluster of bacteria. [1] [2]
S. aureus is a common type of bacteria that appears everywhere in our daily life and has a high lethal rate all around the world.
S. aureus is commonly found in the environment such as soil, water, and air, and also in the nose and on the skin of humans and animals.[3]
Its high lethality is due to its high antibiotic resistance. In the past, doctors used penicillin to treat patients with S. aureus infection but the antibiotic no longer kills the bacteria by the end of 1940s.
S. aureus is famous for its serious infection reaction in the human body. In order for bacteria to cause infection in the human body, they need to escape from the immune system. S. aureus has developed a number of strategies to survive outside of the immune system before infecting a cell. Besides, S. aureus seems to be inextirpable in that it is resistant to nearly all types of antibiotics. Whenever a new drug is tested against S. aureus infection, it fails after preliminary successes.
The infection of S. aureus is completed within the human body. After S. aureus enters the bloodstream, it will be detected by the immune system. Neutrophils, mast cells and different kinds of immune cells quickly respond to the infection site, causing inflammation reaction and other signaling pathways that command the body to fight against the intruder. While they are still in the bloodstreams, S. aureus have a wide variety of mechanisms to avoid being killed by neutrophils. For example, they release cytotoxic compounds to kill phagocytes which inhibit the function of neutrophils. [1]
Inhibition of neutrophil extravasation, activation, and chemotaxis

Extravasation inhibition
The extravasation of neutrophils includes tethering, rolling, adhesion, crawling and transmigration. [4] These steps are inhibited by S. aureus to reduce the ability of neutrophils. One way to inhibit extravasation is to inhibit neutrophil rolling. Staphylococcal superantigen-like protein 5 (SSL5), a member of SSL family that is produced by S. aureus is being used to prevent neutrophil rolling. The rolling of neutrophil is primarily promoted by P-selectin glycoprotein ligand-1 (PSGL-1), a glycoprotein binds to P-selectin that is found on white blood cells and endothelial cells. [5] Recent research suggest that during infection, the interaction between PSGL-1 and P-selectin is being disturbed by SSL5 by directly binding to PSGL-1 and competing with antibiotics. [6]
Activation inhibition
The activation of leukocytes is also inhibited by SSL5. [7] Chemoattractants, the small molecules that bind to the receptors on leukocytes, act as an important factor in neutrophil activation, including stimulation, polarization, and locomotion. [8] Thus, in order to limit the function of neutrophils, SSL5 will also target chemoattractants. In the process of inactivation, SSL5 interact to cells with chemokine and anaphylatoxin receptors on the cell surface and directly bind to G protein-coupled receptors (GPCRs). To be more specific, among variety kinds of chemoattractants, C3a, C5a, and CXCL8 induced-neutrophil stimulation is being inhibited by SSL5. [7]
Chemotaxis inhibition
Chemotaxis, the movement of neutrophils responding to chemoattractants [9], is also inhibited by S. aureus. Research showed that chemotaxis inhibitory protein of S. aureus (CHIPS) is responsible for the inhibition of chemotaxis by specifically targeting and inhibiting the C5a- and fMLP-induced responses. When the gene of CHIPS was identified and knocked-out, S. aureus is not able to prevent chemotaxis. [10] To be more specific, CHIPS cut down the mobilization or neutrophils by affecting fMLP or C5a, by directing binding to their receptors.
Avoid phagocytosis by aggregation and biofilm formation
Aggregation
During the infection, S. aureus sometimes form fibrin-containing bacterial aggregates to elude phagocytosis. [1] To achieve agglutination with fibrinogen, S. aureus produces three important products. They are: coagulase (Coa), von Willebrand factor binding protein (vWbp), and clumping factor (Clfa). Interestingly, fibrinogen is a glycoprotein complex that is produced normally by human body to stop bleeding and it is made of three pairs of three chains of Aα-, Bβ-, and γ-chains. [11] The compounds produced by S. aureus, coagulase and vWbp, promotes cleavage of Aα- and Bβ- chains of fibrinogen. [12] Then, S. aureus uses Clfa to bind to fibrin clots and generate fibrin-containing bacterial aggregates. [1]
Biofilm formation
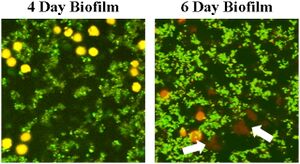
With the assistance of polysaccharide intercellular antigen (PIA), S. aureus forms multilayered biofilm to protect itself from phagocytosis. Within the bacteria cell population, the number of cells is kept at a certain level for S. aureus to metabolize and survive. [13] With the protection of biofilm, macrophages and other immune cells are not prevented from eliminating the essential cells in the population. S. aureus biofilm not only evade TLR2 and TLR9 cognition, but also largely kills the macrophages that invaded into the biofilm. Morphological difference appears between macrophages inside immature biofilm and matured biofilm. Macrophages that entered matured biofilm appear to have ghostlike and deformed morphology compared. Also, research discovered dead macrophages that are closely associated to biofilm. One possible explanation of this phenomenon is that biofilm contains large amounts of polysaccharides, eDNA, and protein polymers that are difficult for macrophages to engulf., leading to frustrated phagocytosis. [14]
Inhibition of opsonization
Surface protein A (SpA)
Opsonization is the second step of phagocytosis. During opsonization, antibodies (immunoglobulins, Igs) are added to pathogens (S. aureus) as tags for them to be more visible for phagocytes. To avoid recognition, S. aureus produce a kind of surface protein called virulence factor A (SpA). SpA contains several immunoglobulin binding-sites that are able to be recognized by IgG antibodies and Variable Heavy 3 (VH3) idiotype antibodies. [15]. Massive plasmablast, the precursor of plasma cells, were observed to response to SpA. Moreover, since nearly all B-cells recognize SpA, the presence of SpA will trigger the production of B-cell, leading the immune response to a wrong track. Therefore, SpA serves as a deceiver to allure antibodies activities, uses up B-cell repertoire, and allows S. aureus to survive.
Complement system
The complement system is also affected by a number of proteins produced by S. aureus. The complement system consists of several small proteins that are produced by liver and circulated in the bloodstream. The proteins could be recruited to the infection site by antibodies as what the adaptive immune system does on lymphocytes. [16] C3-convertase, as one of the important proteins produced by the complement system, is responsible to evaluate opsonization, release of inflammatory peptides, C5 convertase formation, and cell lysis. [17] Additionally, efficient phagocytosis requires the presence of opsonic C3 fragments. To disturb the normal function of immune system especially to opsonization, S. aureus produces the staphylococcal complement inhibitor (SCIN) that blocks C3-convertase to inhibit all major pathways of the complement system. In details, recent study shows that SCIN successfully prevent C3b/iC3b deposition and phagocytosis. [18]
Inhibition of neutrophil killing mechanisms
Staphyloxanthin
A brief look at the killing mechanism of neutrophils:
Reactive oxygen species (ROS), including superoxide (O2-), hypochlorous acid (HOCl), and hydrogen peroxide (H2O2) are normally produced by phagocytes to kill the ingested bacteria inside phagosomes. Myeloperoxidase (MPO) and nicotinamide adenine dinucleotide phosphate (NADPH) both function as producer of ROS that kills the bacteria. [19] [20]

Staphyloxanthin is a carotenoids pigment that gives the yellow (golden) color of S. aureus (Figure 4) and is also crucial for the bacteria to withstand oxidative stress. The pigment serves as an antioxidant that function against molecules like MPO and NADPH. Recent research shows that when crtM, the gene that contribute to the function of carotenoids pigment, was inhibited, S. aureus present to be more susceptible to ROS, indicated by the decreased survival rate of S. aureus over time. [21] Therefore, S. aureus phagocyte resistance is due to the antioxidant property that is directly enhanced by staphyloxanthin.
Multiple peptide resistance factor (MprF)
In addition to ROS, when the phagocytes successfully engulfed bacteria by phagocytosis, they released plenty of peptides that participate in the killing mechanism of bacteria. Antimicrobial peptides (AMPs), as part of the innate immune respons[22], play a role in the elimination of S. aureus inside phagosomes. The effective portion of AMPs is cationic antimicrobial peptides (CAMPs). Just as its name, CAMPs are attracted by negative charge due to electrostatic interaction. The majority of bacterial membrane is made of phospholipids phosphatidylglycerol (PG) and cardiolipin, which are both negatively charged. [23] During elimination, CAMPs are said to recognize S. aureus inside phagosomes. To evade from this killing mechanism, S. aureus produce multiple peptide resistance factor (MrpF) These proteins exert aminoacylation on PG through a series of chemical reactions and thus reduce the negative charge on the bacterial membrane and weaken the electrostatic interaction. [23] The binding and recognition of CAMPs to S. aureus is therefore harder, allowing the bacteria to evade.
Toxin-driven elimination of neutrophils
In additional to passively avoid elimination, S. aureus also forwardly produce toxic chemicals that directly kill neutrophils. The most significant toxins are: α-toxin (Hla), the bicomponent leucocidins, and the PSMs.
α-toxin
Staphylococcus aureus α-hemolysin, which is also called α-toxin, function as a pour former on the cell membrane. In other words, α-toxin punch holes on the cell membrane and allow outer fluid and different kinds of ions to flow into the cell, disturbing cell’s normal function and eventually kill the cell. α-toxin is not only a chemical that lysis normal cells, such as erythrocyte, but also fight against immune cells, such phagocytes and neutrophils. One of the mechanisms S. aureus has is the interference of efferocytosis. Efferocytosis is the process of macrophages cleaning up dead neutrophils that are being infected by bacteria. As mentioned above, S. aureus inhibit the killing mechanism of neutrophils by Staphyloxanthin and MprF, so S. aureus could survive within neutrophils. If the infected neutrophils are not removed from the infection site, S. aureus is likely to keep infecting the cell until the neutrophil is fully died. [cite R]
Bicomponent leucocidins
Panton-Valentine leucocidin (PVL) is a pore-forming toxin produced by S. aureus. the toxic part of PVL consist of two subunit proteins, LukS-PV and LukF-PV. [cite S] Current research suggested that LukS-PV recognize and bind to C5L2 and Ca5 receptor (Ca5R) [cite S], a complement receptor that is normally found on a number of immune cells, such as monocytes and Granulocytes. [cite T] By binding to Ca5 and C5L2, LukS-PV could successfully find neutrophils among many cells at the infection site.
Phenol-soluble modulin (PSM)
Phenol-soluble modulin (PSM) is a type of small protein that has the function of cytolysis. S. aureus produces a number of PSMs, including PSMs, PSMα 1-4, PSMβ 1-2, PSMγ, and PSM-mec. [cite V] Until now, not all kinds of peptides are found to have cytolysis function, but the research [cite U] showed that the PSMα peptide is identified to kill neutrophils and rescue S. aureus. After neutrophil phagocyte the bacteria, the production of PSMα within the neutrophil eventually kills the cell. [cite U]
Conclusion
When S. aureus enter the body from any opening (commonly on skin or in the food) , they travel along the bloodstream and trigger inflammation reaction. The immune cells in the bloodstreams are a major threat to S. aureus as they have to avoid being attacked by the immune system. The strategies used by S.aureus include neutrophils activation and chemotaxis inhibition, phagocytosis inhibition, opsonization suppression, and neutrophils elimination. In specific, S.aureus inhibits phagocytosis by aggregation, biofilm structures, antioxidant molecules, and peptide resistance factors and kills neutrophils by cytolytic toxins or apoptosis.
A better understanding of S. aureus neutrophil evasion mechanism has great contribution to future prevention and treatment of S. aureus infection, including vaccine development and clinical therapy. The recognition and activity of neutrophils and S. aureus requires a series of transduction pathway and biochemical structural analysis. The more detailed and specific mechanisms and protein function require future research.
Include at least 5 references under References section.
References
- ↑ 1.0 1.1 1.2 1.3 Gordon Y. C. Cheung, Justin S. Bae & Michael Otto (2021) Pathogenicity and virulence of Staphylococcus aureus, Virulence, 12:1, 547-569
- ↑ Liu GY, Essex A, Buchanan JT, Datta V, Hoffman HM, Bastian JF, Fierer J, Nizet V. Staphylococcus aureus golden pigment impairs neutrophil killing and promotes virulence through its antioxidant activity. J Exp Med. 2005 Jul 18;202(2):209-15.
- ↑ Agents of Foodborne Illness.
- ↑ Kolaczkowska, E., Kubes, P. Neutrophil recruitment and function in health and inflammation. Nat Rev Immunol 13, 159–175 (2013).
- ↑ Wikipedia: Leukocyte extravasation
- ↑ ovanka Bestebroer, Miriam J. J. G. Poppelier, Laurien H. Ulfman, Peter J. Lenting, Cecile V. Denis, Kok P. M. van Kessel, Jos A. G. van Strijp, Carla J. C. de Haas; Staphylococcal superantigen-like 5 binds PSGL-1 and inhibits P-selectin–mediated neutrophil rolling. Blood 2007; 109 (7): 2936–2943
- ↑ 7.0 7.1 Jovanka Bestebroer, Kok P. M. van Kessel, Hafida Azouagh, Annemiek M. Walenkamp, Ingrid G. J. Boer, Roland A. Romijn, Jos A. G. van Strijp, Carla J. C. de Haas; Staphylococcal SSL5 inhibits leukocyte activation by chemokines and anaphylatoxins. Blood 2009; 113 (2): 328–337
- ↑ Douglas J. Weiss, Bruce Walcheck, in Clinical Biochemistry of Domestic Animals (Sixth Edition), 2008
- ↑ Wikipedia: Chemotaxis
- ↑ de Haas CJ, Veldkamp KE, Peschel A, Weerkamp F, Van Wamel WJ, Heezius EC, Poppelier MJ, Van Kessel KP, van Strijp JA. Chemotaxis inhibitory protein of Staphylococcus aureus, a bacterial antiinflammatory agent. J Exp Med. 2004 Mar 1;199(5):687-95.
- ↑ Wikipedia: Fibrinogen
- ↑ McAdow M, Kim HK, Dedent AC, Hendrickx AP, Schneewind O, Missiakas DM. Preventing Staphylococcus aureus sepsis through the inhibition of its agglutination in blood. PLoS Pathog. 2011 Oct;7(10):e1002307.
- ↑ Archer NK, Mazaitis MJ, Costerton JW, Leid JG, Powers ME, Shirtliff ME. Staphylococcus aureus biofilms: properties, regulation, and roles in human disease. Virulence. 2011 Sep-Oct;2(5):445-59.
- ↑ Lance R. Thurlow, Mark L. Hanke, Teresa Fritz, Amanda Angle, Amy Aldrich, Stetson H. Williams, Ian L. Engebretsen, Kenneth W. Bayles, Alexander R. Horswill, Tammy Kielian; Staphylococcus aureus Biofilms Prevent Macrophage Phagocytosis and Attenuate Inflammation In Vivo. J Immunol 1 June 2011; 186 (11): 6585–6596.
- ↑ Pauli NT, Kim HK, Falugi F, Huang M, Dulac J, Henry Dunand C, Zheng NY, Kaur K, Andrews SF, Huang Y, DeDent A, Frank KM, Charnot-Katsikas A, Schneewind O, Wilson PC. Staphylococcus aureus infection induces protein A-mediated immune evasion in humans. J Exp Med. 2014 Nov 17;211(12):2331-9.
- ↑ Wikipedia: Complement system
- ↑ Wikipedia: C3-convertase
- ↑ Jongerius I, Köhl J, Pandey MK, Ruyken M, van Kessel KP, van Strijp JA, Rooijakkers SH. Staphylococcal complement evasion by various convertase-blocking molecules. J Exp Med. 2007 Oct 1;204(10):2461-71.
- ↑ Klebanoff SJ, Kettle AJ, Rosen H, Winterbourn CC, Nauseef WM. Myeloperoxidase: a front-line defender against phagocytosed microorganisms. J Leukoc Biol. 2013 Feb;93(2):185-98.
- ↑ Clauditz A, Resch A, Wieland KP, Peschel A, Götz F. Staphyloxanthin plays a role in the fitness of Staphylococcus aureus and its ability to cope with oxidative stress. Infect Immun. 2006 Aug;74(8):4950-3.
- ↑ Liu GY, Essex A, Buchanan JT, Datta V, Hoffman HM, Bastian JF, Fierer J, Nizet V. Staphylococcus aureus golden pigment impairs neutrophil killing and promotes virulence through its antioxidant activity. J Exp Med. 2005 Jul 18;202(2):209-15.
- ↑ Wikipedia: Antimicrobial peptides
- ↑ 23.0 23.1 Hwang-Soo Joo, Michael Otto, Mechanisms of resistance to antimicrobial peptides in staphylococci, Biochimica et Biophysica Acta (BBA) - Biomembranes, Volume 1848, Issue 11, Part B, 2015, Pages 3055-3061, ISSN 0005-2736
Edited by Reina He, student of Joan Slonczewski for BIOL 116 Information in Living Systems, 2022, Kenyon College.
