Tea Tree Oil Treatment of MRSA
Introduction
Methicillin-resistant Staphyloccocus aureus (MRSA) is a public health problem. As MRSA is commonly contracted in public settings, such as hospitals, and is not susceptible to commonly used antibiotics, the infection may be very difficult to treat. The impotence of common antibiotics underscores the importance of determining alternative antimicrobial treatments for MRSA. One area of interest involves the use of plant essential oils. Studies indicate the effectiveness of tea tree oil as treatment for infections of drug-resistant bacteria, including methicillin-resistant Staphylococcus aureus, or MRSA.
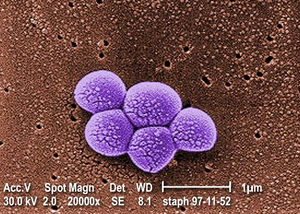
Staphyloccocus aureus, also known as staph bacteria or MRSA, is a Gram-positive coccus-shaped anaerobic bacterium. MRSA is a type of staph bacteria that is resistant to beta-lactam antibiotics, such as penicillin, amoxicillin, oxacillin, and methicillin. MRSA often colonizes on the skin or nostrils of healthy individuals, and is relatively harmless at these sites. If S. aureus enters the body (e.g., wounds, cuts), it may cause infections. In such instances, the MRSA infection may range from mild (e.g., pimples)to life-threatening (e.g., infection of bloodstream, joints, or bones). MRSA is spread through contact and most commonly contracted in public settings, namely hospitals.
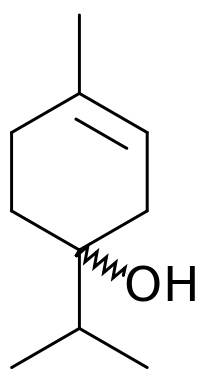
Tea tree oil (TTO) is the essential oil derived through steam distillation from the Australian native plant Melaleuca alternifolia. Tea tree oil has been used for centuries as a topical antiseptic. TTO has antibacterial, antifungal, antiviral, and anti-inflammatory properties in vitro.2 Although historical anecdotes endorse TTO's medicinal properties, few clinical studies have been conducted to support such evidence. Clinical studies, however few, indicate that tea tree oil can treat skin infection caused by MRSA. According to the Centers for Disease Control and Prevention (CDC), MRSA is a public health problem as it is commonly contracted in healthcare and community settings. Tea tree oil's bacteriocidal and bacteriostatic effects make this plant extract a plausible addition or supplement to a MRSA treatment plan. Tea tree oil's anti-microbial properties are attributed to its composition of a chemical class known as terpenes, specifically terpinen-4-ol.
Tea Tree Oil Composition and Chemistry
Commercially available tea tree oil (TTO) is a composition of nearly 100 chemical compounds determined by gas chromatography-mass spectrometry.1 TTO is primarily composed of a class of chemicals called terpenes. Specifically, monoterpenes, sesquiterpenes, and other terpene alcohols dominate this composition. Terpenes are volatile, aromatic hydrocarbons and are typically soluble with nonpolar solvents.2 While research indicates that terpene alcohols are generally effective anti-microbial agents, terpinen-4-ol is the specific terpenic compound believed primarily responsible for TTO's anti-microbial activity.2
TTO composition is internationally regulated and may be commercially available in various chemotypes, including the terpinen-4-ol chemotype where terpinen-4-ol comprises between 30 to 40% of TTO's commercial composition.2 International regulation of TTO's chemical properties calls for this relatively high composition of terpinen-4-ol in commercial production due to its historical medicinal properties. Other terpenic compounds in TTO include 1,8-cineole, terpinolene, and α-terpineol. These compounds also have medicinal properties that are less reputable than those of terpinen-4-ol.
Topical Treatment and Effectiveness
Tea tree oil (TTO) may be included in commercial products, such as body wash, skin cream, and nasal ointment, and can used to treat MRSA. The clinical efficacy of TTO body wash and creams as a decolonization agent for MRSA has been supported, albeit with no statistical significance. Researchers have found that TTO can reduce or prevent MRSA colonization as well as the standard treatment. This suggests that TTO may be considered an alternative or supplement to a MRSA eradication regimen.
Caelli et al.'s (2000) pilot study study compared the effectiveness of TTO to that of routine care treatments, as measured by survivor MRSA concentrations on the skin and within the nose. In the Caelli Lab's clinical study, 30 MRSA-affected adult hospital inpatients were randomly assigned to receive either the routine care (2% mupirocin nasal ointment and triclosan body wash) or tea tree oil regimen (4% TTO nasal ointment and 5% TTO body wash) for at least three days. Caelli et al. found that the tea tree oil regimen performed better (i.e., reduced or eradicated MRSA) in more subjects than the routine regimen, although these results were not statistically significant due to small sample size.
A similar 2013 study conducted by Thompson et al. also found inconclusive results with 445 patients belonging to two intensive care units (ICU) in Northern Ireland.The Thompson Lab sought to determine whether the daily use of TTO body wash had a lower incidence of MRSA colonization. A randomized regimen of either Johnson's Baby Softwash (standard care) body wash or tea tree oil (5%) body wash was assigned to each patient. Patients continued treatment until they reached the study endpoints: detection of hospital-acquired MRSA, ICU discharge, or death. Thompson et al. reported that the TTO regimen did not significantly reduce new MRSA colonization in ICU patients, but claimed that TTO was safe and well-tolerated among patients.
Even though TTO does not seem to be any stronger than the standard decolonization agent for MRSA, it can be more effective at clearing MRSA symptoms. Dryden and Crouch (2004) deemed it to be sufficiently effective, safe, and well-tolerated to be considered part of a MRSA eradication regimen. They found that 5% TTO body wash and 10% TTO applied to skin and nose three times a day for five days and tea tree was more effective than standard treatment at clearing skin lesions, variations in skin texture or color, associated with MRSA.
Antimicrobial Activity: Cytoplasmic Membrane Damage
TTO is reported to disrupt S. aureus cell's membrane permeability. Researchers, Cox et al and Carson et al, examined TTO's effect on S. aureus physiology and found damage to the cytoplasmic membrane. A weakened barrier may allow for undesirable passage of material, such as ions or toxins, and potentially result in bacteriocide or bacteriostasis. The following studies examined the cytoplasmic membrane damage that TTO induces in MRSA.
Cox, S. D. et al (2000) found that exposure of MRSA to the minimum inhibitory concentration of TTO altered cell membrane structure.4 The minimum inhibitory concentration (MIC) is the lowest concentration of antimicrobial, in this case TTO, that will inhibit microbial growth. Cox et al accumulated evidence of cell membrane damage from a propidium iodide uptake assay and ion leakage measurements. As expected, cells that were not exposed to TTO displayed an intact cell membrane. Propidium iodide, a fluorescent nucleic acid staining solution, did not penetrate cells that were not exposed to TTO. Likewise, cells not exposed to TTO showed little potassium ion leakage. This showed that physiologically normal S. aureus cells would not uptake propidium iodide or leak potassium.
From the experiment, Cox et al found that TTO exposure resulted in propidium iodide uptake and potassium ion leakage, signs of a damaged cytoplasmic membrane. In particular, they observed that exposing cell suspensions of MRSA to the minimal inhibitory concentration of 0.25% (v/v) tea tree oil for 30 minutes increased cell permeability to propidium iodide relative to the controls. They also demonstrated that 30 minutes of exposure to TTO caused up to 20% cellular loss of potassium ions. They proposed that TTO components diffused through the cell wall and disrupted the phospholipid regions of cell membrane structures. The ensuing passage of propidium iodide and potassium ions indicated severe cytoplasmic membrane damage.
Carson, C. et al (2002) demonstrated cytoplasmic membrane damage through increased susceptibility to NaCl, loss of cytoplasmic material, and the formation of mesosomes in MRSA treated by TTO or one of its components: terpinen-4-ol, α-terpineol, 1,8-cineole.5 MRSA cells treated with TTO or one of its components were found to be more susceptible to sodium chloride (NaCl), a bacterial cell toxin. Treatment with TTO or its components reduced viability of survivor colonies to <30% viability on NaCl-treated plates. They proposed that the treatment likely damaged the S. aureus cell membrane and affected the bacterial cell's ability to exclude NaCl. Electron microscopy of terpinen-4-ol treated MRSA cells showed mesosome formation that was not observed in untreated cells. Mesosomes, invaginations of the cytoplasmic membrane, along with loss of cytoplasmic material, suggested that the TTO and its components compromised the S. aureus membrane.
Both Cox et al and Carson et al conducted different experiments to demonstrate TTO's devastating effect on the S. aureus cytoplasmic membrane. While much of TTO's mechanism remains unexplored, these studies indicate that TTO targets the cytoplasmic membrane.
Antibiotic Resistance
Include some current research in each topic, with at least one figure showing data.
Conclusion
Though cytoplasmic membrane damage is believed to be the major bacteriocidal effect, there are still many unexplored mechanisms of TTO effects on MRSA.
Overall paper length should be 3,000 words, with at least 3 figures.
References
http://www.nhs.uk/conditions/MRSA/Pages/Introduction.aspx
http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0004520/
http://www.nlm.nih.gov/medlineplus/druginfo/natural/113.html
http://epubs.scu.edu.au/cpcg_pubs/482/
http://openi.nlm.nih.gov/detailedresult.php?img=3258290_1472-6882-11-119-1&req=4
Edited by Karen Leung, a student of Nora Sullivan in BIOL187S (Microbial Life) in The Keck Science Department of the Claremont Colleges Spring 2013.