The Role of Clostridium perfringens Toxins in Gas Gangrene
What is Gas Gangrene and What Causes It?
By Marysol Arce

Gas gangrene is caused by a rod shaped, gram positive, spore forming bacterium called Clostridium perfringens. The bacterium lives in anaerobic environments like the soil and inside the gut of humans and animals (Williamson and Titball 1993). Clostridium perfringens is currently known to have five different strains, marked as: A, B, C, D, and E (Sakurai et al. 2004). The different strains are classified based on which toxins they produce: alpha toxin, beta toxin, epsilon toxin, and/or iota toxins (Shimizu et al. 2001). The Clostridium perfringens A strain is of the most importance because it causes gas gangrene, or myonecrosis, in humans. Gangrene is the death of body tissue and usually seen in elderly people or diabetic people. Open wounds or trauma into deep tissue that become infected by bacteria also become gangrenous. Gas gangrene is an especially dangerous form because it spreads quickly throughout the body if left untreated, and can be fatal. C. perfringens produces toxins that kills cells and releases gas, leaving parts of the body black, purple, and covered with blisters. The A strain of the C. perfringens bacterium produces two important toxins that enable the spread of the bacterium and tissue death: the alpha toxin and perfringolysin O (O’Brien and Melville 2004). The alpha toxin, also known as CPA or PLC, is a crucial virulence factor for this bacterium because gas gangrene cannot occur without it. However, the alpha toxin and perfringolysin O (PFO) work synergistically to accomplish the spread of infection [1]. The toxins can cause septic shock (when infection leads to very low blood pressure) and hypoxia (reduced amounts of oxygen to body tissues). It even causes organ failure and muscle degeneration due to the lack of oxygen and reduced blood flow. The degeneration of the muscle and tissue releases gas that builds up under the skin and makes the area blister and bubble. The appearance of these blisters in various parts of the body usually indicates that the infection has progressed very far and that the tissue is decomposing. The body’s immune system is also rendered helpless because the toxins make the leukocytes clump together and clog in the blood vessels (leukostasis), unabling them to get to the site of infection (Stevens and Bryant 2002). The toxins also cause further blood vessel dysfunction, like vascular leakage which is what makes swelling a big characteristic of this disease.
Clostridium perfringens genome
The bacterium Clostridium perfringens’ genome is a lone circular chromosome with additional plasmids that are extra-chromosomal, meaning that there is other DNA found outside of the nucleus (Verherstraeten et al. 2015). It is made up of 2,660 regions that encode proteins and 10 ribosomal RNA genes (Shimizu et al. 2002). The genome also possesses the anaerobic fermentation enzymes usually found in bacterium that allow for gas production. However, it does not have any tricarboxylic acid (TCA) cycle enzymes or for a respiration mechanism. Many saccharolytic enzymes are present but most of the enzymes needed in amino acid biosynthesis are not present in the genome. There are at least 20 genes that encode virulence factors for the bacterium and 5 hyaluronidase genes, which encode enzymes that degrade hyaluronic acid, that also add to C. perfringens virulence (Shimizu et al 2001). There are also 4 regulons that regulate the pathogenicity, the ability of the organism to cause disease, of the bacterium. Clostridium perfringens utilizes and gains many different crucial materials needed to perform their function from the host cells by producing many degradative toxins and enzymes. To obtain what they need, the bacterium uses these toxins and enzymes to destroy the host’s tissues and cells. The two critical toxins of C. perfringens A strain, alpha toxin and perfringolysin O, are both chromosomally encoded (Li et al. 2013).
Other examples:
Bold
Italic
Subscript: H2O
Superscript: Fe3+
Introduce the topic of your paper. What is your research question? What experiments have addressed your question? Applications for medicine and/or environment?
A citation code consists of a hyperlinked reference within "ref" begin and end codes.
[2]
Alpha Toxin (PLC)
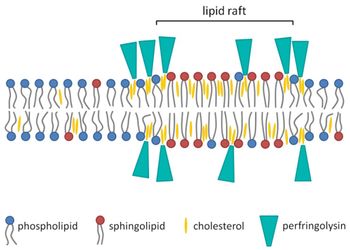
All strains of C. perfringens can produce the alpha toxin, also known as Clostridium perfringens alpha toxin (CPA) or by its main enzyme, phospholipase C (PLC) (Li et al. 2013). The alpha toxin is the most toxic enzyme that is produced by the A strain, and is also a crucial virulence factor. It has phospholipase C and sphingomyelinase that hydrolyzes phosphatidylcholine (PC) and sphingomyelin (SM), two very important components of a eukaryotic cell membrane (Awad et al. 2001). Alpha toxin degrades PC and SM in membranes and disrupts membranes, leading to cell lysis. For the alpha toxin to break down the host cell’s membrane, it promotes carboxyfluorescein (CF) leakage and phosphorylcholine release from the host’s liposomes which are made up of either PC or SM (Sakurai et al. 2004). By cleaving molecules from the exterior of the host cell's phospholipid bilayers and interrupting the membrane’s functions, it then promotes cell lysis and ultimately death. The alpha toxin’s membrane-damaging ability is also dependent of the membrane’s fluidity. Other actions caused by the toxin are hemolysis (rupture of red blood cells), dermonecrosis (death of skin tissue due to lack of blood flow), and lethality (Sakurai et al. 2004). The alpha toxin promotes endothelial cells (cells that line the inside of blood vessels) to be produced by intercellular mediators. In addition, it also promotes the production of the intercellular adhesion molecule 1, an endothelial leukocyte adhesion model, and a platelet activating factor (Sakurai et al. 2004). The toxin induces the relocation of the platelet fibrinogen receptor from the inside of the platelet to its membrane. This relocation then triggers the formation of more platelets and platelet aggregates (Sakurai et al. 2004). These actions contribute greatly to an elevated vascular permeability and leads to edema, defined by the buildup of fluid in the tissues. Essentially, the alpha toxin is able to escape the leukocytes and move out of the blood vessels and into the cells. The leukocytes are unable to move or stop the infection because they are stuck with the platelets and can only watch while the toxin kills the tissues. Researchers have also discovered that the activation of the sphingomyelin (SM) cycle is a fundamental event within the signal transduction pathway that takes part in cellular proliferation, differentiation, and apoptosis (Sakurai et al. 2004). A crystallography of alpha toxin reveals its structure to be composed of two domains: the N domain and the C domain. The N domain is composed of 9 ⍺-helices that are tightly packed together. The C domain consists of an 8 stranded antiparallel β-sandwich motif (Sakurai et al. 2004). The N domain also includes 3 divalent cations that contain zinc ions in the active site (Sakurai et al. 2004). Zinc is highly important for the alpha toxin because it is essential for the toxin’s activity in vivo and has also been found to enhance alpha toxin production in vitro (Stevens and Bryant 2002). Amino acid residues participate in zinc coordination and prove necessary for the toxin’s enzymatic activities (Sakurai et al. 2004). The C domain of alpha toxin also performs the most important part when lysing the host cells. The C domain is the part of the alpha toxin that is inserted into the host cell’s phospholipid bilayer to disrupt the membrane (Sakurai et al. 2004). The two domains are also highly crucial in hemolysis, the destroying of erythrocytes, or red blood cells. The N domain itself cannot bind or lyse the them; the C domain must be the one to bind to the red blood cell’s membrane (Nagahama et al. 2002). Then by combining the N domain and C domain, the alpha toxin gets it hemolytic power. To summarize, the alpha toxin elicits biological activities and processes that are inherent to tissues and cells. First, the toxin attaches to the binding site on the exterior of the membrane, then the C domain inserts itself into the host membrane. Next, the N domain follows: attacking and hydrolyzing the PC and SM within the membrane. The hydrolysis stimulates the signal transduction pathway through activation of phospholipase C and / or SMase (Sakurai et al. 2004).
Include some current research, with at least one figure showing data.
Every point of information REQUIRES CITATION using the citation tool shown above.
All strains of C. perfringens produce the alpha toxin, also called CPA or PLC. The alpha toxin cleaves molecules from the surface the host cell's’ phospholipid bilayers and disrupts the membrane’s functions, which then promotes cell lysis and death.

Perfringolysin O (PFO)
All strains of C. perfringens can produce the toxin perfringolysin O (PFO). The structure of PFO is a signal peptide that is secreted by the general secretory pathway (GSP) in the bacterium. When this signal peptide passes through the cell membrane, it is cleaved, resulting in an water-soluble monomer in the extracellular space. This toxin is part of a pore-forming toxin family, the cholesterol-dependent cytolysin (CDC) family (Verherstraeten et al. 2015). The PFO that was secreted as the water-soluble monomer can only recognize and bind to cholesterol in the plasma membrane (Verherstraeten et al. 2015). Cholesterol is common component of animal cells and is required for the toxin to perform its function. Once recognizing and attaching to cholesterol in the membrane, PFO oligomerizes at the host cell’s exterior and constructs a pore complex. Next it inserts itself into the cell membrane to form a large pore (Li et al. 2013). The formation of this large pore disrupts the cell membrane, which causes cell lysis and cell death. But has been thought that cell lysis is not the main biological effect of this toxin on C. perfringens affected tissue (Li et al. 2013). PFO, as well as the alpha toxin, prevent white blood cell from arriving at the site of infection. Because the body’s immune system is not able to fight the bacterium at the site of infection, the toxin aids in the decay of flesh and tissue. Although the alpha toxin is critical to the virulence, PFO is not. Even though it may not be essential, it is synergistic with the alpha toxin. Both act together and boost the effect of the disease to speed up necrosis. If the host’s cells are lysed it makes it easier for the bacterium to infiltrate the cell and speeds up the process of necrosis. PFO is also like a double edged sword: it has a separate function in different stages of gas gangrene infection. In the early stages of infection, it causes macrophage cytotoxicity (O’Brien and Melville 2004). In the later stages of infection, it causes thrombosis, which is the clotting of blood cells in the blood vessels (Awad et al. 2001). Although PFO plays a big role in thrombosis, the alpha toxin does as well, and the two work synergistically (described further in the section: Synergy of Alpha Toxin and Perfringolysin O to Spread Gas Gangrene). To summarize PFO’s mechanism in cell lysis and furthering the infection, there are four main steps. First, the toxin binds to the cholesterol inside membranes. Second, it inserts itself into the membrane. Third, it oligomerizes, and fourth, it forms a pore that disrupts the cell (Shimada et al. 1999).
How Do These Toxins Help C. perfringens Persist and Spread in the Body?
Alpha Toxin and PFO Allow C. perfringens to Escape from Macrophages and the Immune System C. perfringens is able to avoid and escape its host’s the immune system’s phagocytic cells, especially polymorphonuclear cells (PMNs). Because gas gangrene develops until it can finally be seen, which usually means the infection is severe, it shows that the macrophages and other white blood cells cannot kill the bacterium efficiently (O’Brien and Melville 2004). The ineffectiveness of the phagocytic cells like PMNs is attributed to the alpha toxin and perfringolysin O (PFO). Purified PFO has been seen to have cytotoxicity to PMNs in vitro while purified alpha toxin (PLC) has been seen to have little cytotoxicity to PMNs in vitro (O’Brien and Melville 2004). Therefore, although both toxins play a role in the weakening of the body’s immune response, PFO might have a greater cytotoxic effect on macrophages than the alpha toxin. C. perfringens also shares similarities with pathogens like species of Listeria and Shigella, which escape the phagosome of macrophages and replicate in the cytoplasm. Although the ability of the bacterium to escape phagosomes is known, it is unclear if it is able to replicate in the cytoplasm (O’Brien and Melville 2004). Both the alpha toxin and PFO are membrane-active toxins which make them helpful in escaping the phagosome. Because PFO oligomerizes to construct large pores on cholesterol-possessing membranes, it could have the ability to lyse the phagosome’s membrane and allow for escape. But the alpha toxin has a lower ability of mediating phagosomal escape. Therefore, the alpha toxin alone cannot mediate escape and survival inside the macrophages (O’Brien and Melville 2004). Both the alpha toxin and the PFO must work together to yield the best, most efficient means of phagosomal escape.
Host Defense Against C. Perfringens and Host Surrender to C. Perfringens The host has a weak defense against C. perfringens and is more easily overtaken as time passes. In the earliest stages of infection, the primary host defense is most likely the phagocytes of the innate immune system, which are primarily macrophages and polymorphonuclear cells (PMNs). As the infection progresses to its later stages where the bacteria have proliferated enough so that the gas gangrene is visible, there is a significant scarcity of phagocytes near the where the bacterium are. A lack of oxygen in the wound area also aids in the growth of anaerobic C. perfringens, which is helpful to gas gangrene because it usually begins in dead tissue.
Synergy of Alpha Toxin and Perfringolysin O to Spread Gas Gangrene
The alpha toxin is a requirement for: tissue necrosis, the obstruction of polymorphonuclear leukocytes (PMNL) increase into the infection site, and development of thrombosis (Awad et al. 2001). Thrombosis, or blood clotting, is especially important for gas gangrene to resist the immune system’s attack because it reduces the oxygen tension in tissues. This provides a suitable environment for anaerobic C. perfringens to grow. It is has been discovered that purified alpha toxin induces aggregation of platelets in the blood vessels. Because the platelets are clumped together and blocking the way in the blood vessels, the leukocytes cannot pass through and travel to the infected tissues to fight the infection. Therefore, the alpha toxin plays a major part by reducing blood flow and fighting the host’s immune system to enable further infection. PFO, like the alpha toxin, plays a similar role in the build up of leukocytes inside blood vessels and the extracellular space of host tissues (Stevens and Bryant 2002). PFO causes a heightened expression of adhesion molecules like those of leukocytes, and the platelet activating factor of human endothelial cells (Verherstraeten et al. 2015). This increase in expression the platelet activating factor and the endothelial cell adhesion factor contribute to platelet-leukocyte masses sticking onto the lining of the blood vessels and blocking them. Again, if the blood vessels become blocked, it leads to thrombosis and reduced blood flow. Without oxygen going to the tissues, anaerobic C. perfringens can flourish and further necrosis. Perfringolysin O also furthers the spread of infection by lysing red blood cells. Red blood cells are important machinery of humans that carry oxygen through the blood vessels to our tissues. If our red blood cells are destroyed or lysed by PFO, there will be no way for oxygen to travel to parts of our body and our cells will die. In this way, PFO has two mechanisms to prevent the immune system from fighting the infection: by blocking blood vessels so that white blood cells cannot travel to the infection and by lysing the very cells that carry the necessary oxygen we need to function. Awad and colleagues held an experiment where they infected mice with the wild type strain of C. perfringens bacteria that produced the typical symptoms of gas gangrene with thrombosis and vascular leukostasis. Then they infected another group of mice with a strain that was void of the genes that enabled production of alpha toxin and PFO. This group of mice showed very little symptoms of gas gangrene and little to no leukostasis in the blood vessels was seen. The leukocytes were able to travel to the infected tissues and fight the infection. They concluded from this experiment that both toxins are needed to work synergistically to allow the bacterium to evade the immune system and survive inside the host (Awad et al. 2001).
Role of the Alpha Toxin and Perfringolysin O in: Cytotoxicity Towards Macrophages and the Ability to Escape From Phagosomes of Macrophages
PFO was discovered to have an essential part in both cytotoxicity and escape of macrophages, therefore making it a crucial virulence factor of gas gangrene, helping the bacterium resist being killed by macrophages. In O’Brien and Melville’s experiment, they examined the role of PFO in the early stages of gas gangrene infection, at a time when the number of bacteria present was few relative to the number of phagocytic cells. They found that for the C. perfringens bacterium to persist in the host’s tissues, PFO was equally mandatory as the alpha toxin. This supports the crucial role PFO plays in the early stages of gas gangrene infection, where the ratio of bacterial cells to phagocytic cells is relatively low (O’Brien and Melville 2004). Once the bacterium resists being killed by the macrophages and PMNs early into the infection, it is able to continue its spread deeper in the tissues. We can conclude that PFO is more crucial than the alpha toxin, although having both would be a bigger advantage in the spread of the infection than having just one toxin. PFO is the more important factor of cytotoxicity of the two (Verherstraeten et al. 2015).
Treatments Against Gas Gangrene
Gas gangrene is much easier to treat if caught early, but symptoms may not be visible until severe stages. One mode of treatment is antibiotic therapy. The most common antibiotics used are penicillin and clindamycin, and both are usually used simultaneously. There have also been recent studies conducted that protein synthesis inhibitors might be more effective ways of treatment than antibiotics. If doctors are able to block the synthesis of C. perfringens alpha toxin and perfringolysin O, they can reduce the amount of toxins inside the patient’s body and therefore lessen the effects of these toxins. People affected by gas gangrene are also usually affected by organ failure. They need intensive care due to necrosis affecting organs. Another mode of treatment is hyperbaric oxygen therapy, or HBO therapy. Although it has been used in the U.S. for gas gangrene treatment for a long time, it is controversial. The treatment involves administering 100% oxygen to patients for prolonged periods of time. Studies for this type of treatment on gas gangrene have reported that it inhibits alpha toxin production and makes the living and dead tissue more visible from each other. Therefore, this treatment is most likely better to use before surgery, excision, or amputation. There are however some risks like trauma resulting from pressure and oxygen toxicity. Ultimately, if gas gangrene of a patient cannot be treated with any of these methods, they will have to undergo surgery and/or amputation. The necrotic tissue must be cut off and physically removed so that it does not spread further in the body. If whole limbs are necrotic, they must be amputated. Removal of parts of the body is much better than letting the infection spread more and leading to death.
Gas Gangrene in Animals
Gas gangrene is not just limited to humans. Many agricultural animals like cattle, sheep, and horses can also suffer from it. Their symptoms are similar to humans: edema, emphysema, skin discoloration, and toxemia (Li et al. 2013). It is assumed that the main virulence factors for gas gangrene in animals is the alpha toxin (CPA) and perfringolysin O (PFO) like humans because of the similarity in symptoms (Li et al. 2013).
References
- ↑ Awad, Milena M., Darren M. Ellemor, Richard L. Boyd, John J. Emmins, and Julian I. Rood. "Synergistic Effects of Alpha-Toxin and Perfringolysin O in Clostridium Perfringens-Mediated Gas Gangrene." 2001. Infection and Immunity 69(12):7904-910. DOI: 10.1128/IAI.69.12.7904–7910.2001
- ↑ Zhao, Ge, Marcia L. Usui, Soyeon I. Lippman, Garth A. James, Philip S. Stewart, Philip Fleckman, and John E. Olerud. "Biofilms and Inflammation in Chronic Wounds." 2013. Advances In Wound Care 2(7):389-399. DOI: 10.1089/wound.2012.0381
