Toxoplasmosis
From: http://www.oculist.net/downaton502/prof/ebook/duanes/pages/v4/v4c046.html

From: http://www.economist.com/node/16271339
Description/Etiology/Taxonomy
Toxoplasma gondii is an obligate, intracellular parasitic protozoan that infects most species of warm blooded animals, including humans, and is the causative agent of the disease Toxoplasmosis. While T. gondii may infect humans and cause disease, the only host in which the protozoa may complete its life cycle are family Felidae, more commonly known as domestic cats and their relatives. [1]
Taxonomy of Toxoplasma gondii
Domain: Eukaryota
Kingdom:Chromalveolata
Superphylum: Alveolata
Phylum: Apicomplexa
Class: Conoidasida
Subclass: Coccidiasina
Order: Eucoccidiorida
Family: Sarcocystidae
Subfamily: Toxoplasmatinae
Genus: Toxoplasma
Species: Toxoplasma gondii
Pathogenesis
Transmission
Lifecycle
The only hosts in which Toxoplasma gondii can mature and reproduce are members of the family Felidae. Infected domestic cats (and those related to them) will shed large numbers of unsporulated oocysts in their feces for approximately one to two weeks. Oocysts released into the environment take from one to five days to form spores and become capable of causing infection. Intermediate hosts, commonly birds and rodents as they are typical prey of felines, may then become infected by consuming materials contaminated with T. gondii spores. After ingestion, oocysts develop into tachyzoites which localize in neural and muscle tissues to develop into cyst bradyzoites. Members of the family Felidae become infected after consuming intermediate hosts that have these cysts in their tissues. Additionally, other animals may become infected with cysts after ingesting T. gondii spores from the environment. [1]
Infecting humans
Humans may become infected with Toxoplasma gondii by a variety of routes. The most common methods of infection include: consuming undercooked meat of animals that had tissue cysts, consuming food or water contaminated with infected cat feces, consuming food or water contaminated by infected environmental samples (e.g. soil, cat litter), receiving a blood transfusion or organ transplant from individuals harboring tissue cysts, and infection of a fetus transplacentally from the mother. Unlike its lifecycle in felines and intermediate hosts, T. gondii commonly forms cysts in the skeletal muscle, brain, eyes, and myocardium of the human host. Additionally, rather than being shed in feces like the feline host, the cysts in a human host may remain for the entire life of the human host. [1]
Colonization
Infectious dose/Incubation period
Virulence factors
Clinical features
Diagnosis
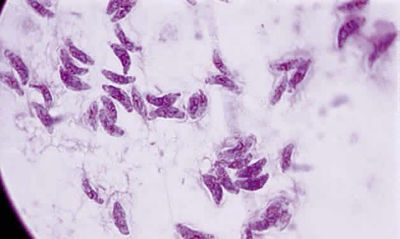
Diagnosis of Toxoplasmosis is generally achieved via serology, or the examination of plasma or other bodily fluids to determine whether the body has produced antibodies in response to a specific antigen. Additionally, Toxoplasmosis may be diagnosed via the identification of T.gondii cysts in a tissue sample taken from a suspected infected individual. Diagnosis of Toxoplasmosis infection before birth may be determined by confirming the presence of T. gondii DNA in amniotic fluid. [1]
Treatment
Prevention
Host Immune Response
References
SAMPLE REFERENCES
1 Centers for Disease Control (CDC). General Information Salmonella.Page last updated: April 5, 2012
2 Shannon E. Majowicz, Jennie Musto, Elaine Scallan, Frederick J. Angulo, Martyn Kirk, Sarah J. O'Brien, Timothy F. Jones, Aamir Fazil, Robert M. Hoekstra The Global Burden of Nontyphoidal Salmonella Gastroenteritis.Oxford Journals. Medicine Clinical Infectious Diseases. Food Safety. Volume 50, Issue 6Pp. 882-889.
3 Centers for Disease Control (CDC). Multistate Outbreak of Salmonella Typhimurium and Salmonella Newport Infections Linked to Cantaloupe (Final Update). Posted October 5, 2012 3:15 PM ET
4 Mayo Clinic Staff. Salmonella infection. April 16, 2011.
5 Marler Clark. PHow is Salmonella Infection Diagnosed? 2005-2013.
6 Juan Miguel Morata. Different Types of Agar.
7 National Institue of Allergy and Infectious Diseases Staff. Salmonellosis.
8 Wikipedia entry: Salmonella. page was last modified on 16 July 2013
9 Giannella RA. Salmonella. In: Baron S, editor "'Medical Microbiology. 4th edition. Galveston (TX): University of Texas Medical Branch at Galveston; 1996. Chapter 21
Created by Magdalene C. Shaughnessy, student of Tyrrell Conway at the University of Oklahoma
