Tuberculosis disease: Difference between revisions
| Line 40: | Line 40: | ||
<li> <b>A thorough physical examination:</b> </li> This can allow for health care providers to asses overall health and knowledge that will lead to the treatment, if the patient is determined to be infected with <i>Mycobacterium tuberculosis</i>. | <li> <b>A thorough physical examination:</b> </li> This can allow for health care providers to asses overall health and knowledge that will lead to the treatment, if the patient is determined to be infected with <i>Mycobacterium tuberculosis</i>. | ||
<li> <b>Testing for the presence of <i> Mycobacterium tuberculosis</i>:</b> </li> The two most common tests are the Mantoux tuberculin skin test (TST) and the TB blood test. The TST is accomplished by injecting 1/10th of a milliliter (mL) of tuberculin is injected into the patient’s skin, usually in the mid forearm. 48-72 after the injection, a health care provider reads the test and documents the results. If there is no reaction, the test is considered negative, however if redness and swelling occur the presentation of the reaction determines if a test is considered positive or not. | <li> <b>Testing for the presence of <i> Mycobacterium tuberculosis</i>:</b> </li> The two most common tests are the Mantoux tuberculin skin test (TST) and the TB blood test. The TST is accomplished by injecting 1/10th of a milliliter (mL) of tuberculin is injected into the patient’s skin, usually in the mid forearm. 48-72 after the injection, a health care provider reads the test and documents the results. If there is no reaction, the test is considered negative, however if redness and swelling occur the presentation of the reaction determines if a test is considered positive or not. | ||
5 mm of hard swelling will be considered positive if the patient: | 5 mm of hard swelling will be considered positive if the patient: | ||
<ul> | <ul> | ||
| Line 61: | Line 60: | ||
</ul> | </ul> | ||
Any test with results 15 mm or larger of hard swelling will be considered positive whether is patient is at risk or not. | Any test with results 15 mm or larger of hard swelling will be considered positive whether is patient is at risk or not. | ||
<li> <b>Chest X-Ray or more in depth studies if needed:<b> </li> This is not a test that can allow a physician to diagnose a patient with TB, but can rule out pulmonary TB if a patient has presented with a positive TST or blood test. | <li> <b>Chest X-Ray or more in depth studies if needed:</b> </li> This is not a test that can allow a physician to diagnose a patient with TB, but can rule out pulmonary TB if a patient has presented with a positive TST or blood test. | ||
<li> <b>Culturing of the samples taken from the patient:</b></li>This method of culturing the bacteria is the only definitive way to diagnose a patient with a <i> Mycobacterium tuberculosis </i> infection. All positive results of this test must be reported to the primary care physician and the state. | <li> <b>Culturing of the samples taken from the patient:</b></li>This method of culturing the bacteria is the only definitive way to diagnose a patient with a <i> Mycobacterium tuberculosis </i> infection. All positive results of this test must be reported to the primary care physician and the state. | ||
<li><b> Testing the <i> Mycobacterium tuberculosis</i> for drug resistance, due to possibility of having drug resistant tuberculosis (MDR TB) or worse, extremely drug resistant tuberculosis (XDR TB):</b></li> This is incredibly important because if the <i>M. tuberculosis </i> strain is resistant, then an appropriate regiment needs to be prescribed to the patient to ensure the best scenario of curing the patient. | <li><b> Testing the <i> Mycobacterium tuberculosis</i> for drug resistance, due to possibility of having drug resistant tuberculosis (MDR TB) or worse, extremely drug resistant tuberculosis (XDR TB):</b></li> This is incredibly important because if the <i>M. tuberculosis </i> strain is resistant, then an appropriate regiment needs to be prescribed to the patient to ensure the best scenario of curing the patient. | ||
Revision as of 15:55, 21 July 2013

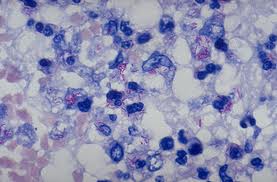
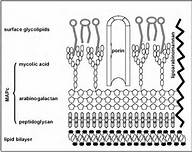
Etiology/Bacteriology
Taxonomy
Kingdom: Bacteria
Phylum: Actinobacteria
Class: Actinobacteria
Order: Actinomycetales
Family: Mycobacteriaceae
Genus: Mycobacterium
Species: tuberculosis
Description
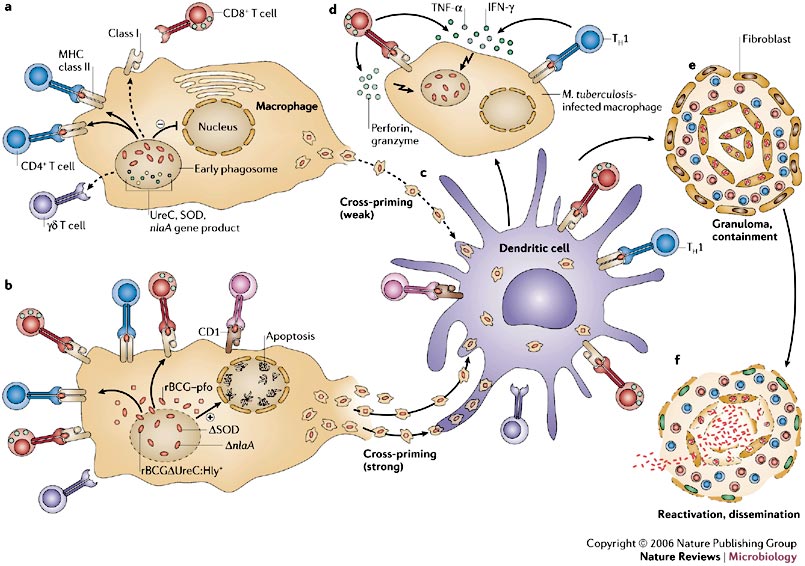
Pathogenesis
Transmission
Infectious Dose, Incubation, and Colonization
Epidemiology
Virulence Factors
Clinical Features and Symptoms

Diagnosis
If the patient is experiencing the symptoms described above it is highly likely they will be tested for the presence of Mycobacterium tuberculosis in their body. The evaluation process for a disease as serious as tuberculosis is a daunting one, but physicians need to be absolutely sure to produce a proper diagnosis. The steps for diagnosing a patient presenting with symptoms similar to TB include:
- Obtaining the patients’ medical history: Health care providers must determine if the patient has been exposed to TB, as well as illnesses that leave the patient immunodeficient. Demographic, such as age and occupation are important factors in determine if the patient is in an at risk group for contracting TB.
- A thorough physical examination: This can allow for health care providers to asses overall health and knowledge that will lead to the treatment, if the patient is determined to be infected with Mycobacterium tuberculosis.
- Testing for the presence of Mycobacterium tuberculosis: The two most common tests are the Mantoux tuberculin skin test (TST) and the TB blood test. The TST is accomplished by injecting 1/10th of a milliliter (mL) of tuberculin is injected into the patient’s skin, usually in the mid forearm. 48-72 after the injection, a health care provider reads the test and documents the results. If there is no reaction, the test is considered negative, however if redness and swelling occur the presentation of the reaction determines if a test is considered positive or not. 5 mm of hard swelling will be considered positive if the patient:
- Has been diagnosed with HIV
- Is immunodeficient
- Has ever had an organ transplant
- Has come into contact with someone who has active TB
- Has worsening chest X-Rays
- Has presented with a negative test within 2 years
- Has a condition that increases their chances of contracting TB
- Is a health care professional
- Is an intravenous (IV) drug user
- Immigrants from a country with a high rate of TB who moved to the United States less than 5 years ago
- Is under the age of four years old
- Is exposed to high risk adults, and are infants, children, or teenagers
- Is frequently in an area of high TB risk, such as homeless shelters and jails
- Chest X-Ray or more in depth studies if needed: This is not a test that can allow a physician to diagnose a patient with TB, but can rule out pulmonary TB if a patient has presented with a positive TST or blood test.
- Culturing of the samples taken from the patient: This method of culturing the bacteria is the only definitive way to diagnose a patient with a Mycobacterium tuberculosis infection. All positive results of this test must be reported to the primary care physician and the state.
- Testing the Mycobacterium tuberculosis for drug resistance, due to possibility of having drug resistant tuberculosis (MDR TB) or worse, extremely drug resistant tuberculosis (XDR TB): This is incredibly important because if the M. tuberculosis strain is resistant, then an appropriate regiment needs to be prescribed to the patient to ensure the best scenario of curing the patient.
10 mm or greater of hard swelling will be considered positive if the patient:
Any test with results 15 mm or larger of hard swelling will be considered positive whether is patient is at risk or not.
Treatment
Prevention
Host Immune Response
References
1 Conway, Tyrrell. “Genus conway”. “Microbe Wiki” 2013. Volume 1. p. 1-2.
