Tuberculosis disease

Etiology/Bacteriology
Taxonomy
Kingdom: Bacteria
Phylum: Actinobacteria
Class: Actinobacteria
Order: Actinomycetales
Family: Mycobacteriaceae
Genus: Mycobacterium
Species: tuberculosis
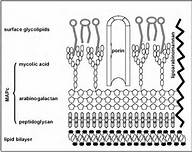
Description
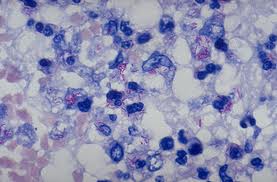
Pathogenesis
Transmission
Infectious Dose, Incubation, and Colonization
Epidemiology
Virulence Factors
Clinical Features and Symptoms
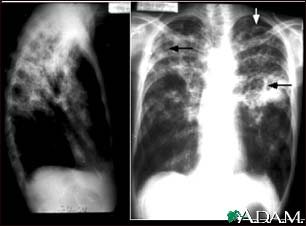
Diagnosis
Treatment
There are multiple treatments for tuberculosis, because the patient could be diagnosed with a latent TB infection or TB disease. Only if the risk of TB outweighs those of the antibiotics is a patient treated. If it is decided that action is needed TB is treated with the antibiotics isoniazid (INH), rifampin (RIF), and rifapentine (RPT). There are four different treatment routines that include isoniazid daily for nine months, isoniazid daily for six months, isoniazid and rifapentine once a week for three months, or rifampin daily for 4 months. The regiment of isoniazid and rifapentine is one that is to be taken along with directly observed therapy (DOT), due to the high risk of liver damage and death. Due to the tragic side effects, the grouping of isoniazid and rifapentine is strongly discouraged and rarely prescribed. Tuberculosis disease is treated with the four antibiotics isoniazid (INH), rifampin (RIF), ethambutol (EMB), and pyrazinamide (PZA). The treatment for pulmonary TB has two steps, starting with a combination of isoniazid, rifampicin, pyrazinamide, and ethambutol once a day for two months. The next four months of treatment consist of the patient taking only isoniazid and rifampicin for another four months. Extrapulmonary TB is treated with the same antibiotics used for pulmonary TB; INH, RIF, EMB, and PZA. The length of time needed to cure this form of TB is longer, therefore, antibiotics are prescribed to be taken during a twelve month span. If M. tuberculosis is to colonize in the patient’s brain, a corticosteroid will be prescribed for approximately a month in addition to the antibiotic regiment. This corticosteroid is prescribed to control the swelling around the brain as a result of the TB. It is crucial that patients take every dose of antibiotics as instructed for the indicated amount of time to be sure all the bacteria is killed and resistance does not occur.
Prevention
There is currently a vaccine, Bacillua Calmette-Guerin (BCG), which aims protect certain groups from the disease, although is 100% effective. The criteria for this vaccine varies depending on the country one resides. In the United States, a vaccine is not given until the set guidelines have been met and the patient has been seen by a doctor considered an expert with the TB disease. The guidelines broken down into two categories for the United States are:
Children
- An accredited hospital has recorded the patient is TB positive, through the reading of a skin test
- The child must remain in contact with persons diagnosed with TB that are not or inadequately treated for the disease
- The child must remain in contact with persons that were infected with Mycobacterium tuberculosis that is resistant to the antibiotics isoniazid and rifampin
Health Care Workers The consideration for this vaccine is only on an individual basis, in which the person
- Is in contact with a large population of TB patients infected with Mycobacterium tuberculosis that is resistant to isoniazid and rifampin
- Drug-resistant TB is being transmitted between health care workers
- Widespread preventative measures against the spread of TB have been implemented, but deemed unsuccessful
Most patients vaccinated with the BCG vaccine will proved a positive TB skin test, due to their immunological memory and the exposure of Mycobacterium tuberculosis.
In most cases the prevention of TB is related to how the disease is controlled. There are many different measures that need to be controlled when a TB prevention plan is put into effect.
Host Immune Response
Tuberculosis acts in a two-step mechanism that begins with a primary infection and as the host deteriorates the secondary disease can occur. When infected with the Mycobacterium tuberculosis a healthy individual with a strong immune system presents asymptomatically or with mild flu like symptoms. Due to being of low to no risk, most patients are left with these bacteria growing and colonizing within their body. Pulmonary tuberculosis infections begin with the Mycobacterium tuberculosis invading and reproducing within the macrophages residing in the infected alveoli. As immune cells make their way to the lymph nodes, the adaptive immune response is initiated by T cells. At this point multiple sites of the body are experiencing the process of inflammation. Not much is known about the immune system and how Mycobacterium tuberculosis effects it.
References
1 Conway, Tyrrell. “Genus conway”. “Microbe Wiki” 2013. Volume 1. p. 1-2.
