Tuberculosis disease

Etiology/Bacteriology
Taxonomy
Kingdom: Bacteria
Phylum: Actinobacteria
Class: Actinobacteria
Order: Actinomycetales
Family: Mycobacteriaceae
Genus: Mycobacterium
Species: tuberculosis
Description
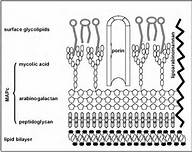
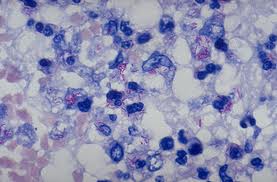
Mycobacterium tuberculosis is an acid fast, nonmotile, obligate anaerobe. These bacilli range in size from 2-4 µm and have an incredibly slow generation time of 15 to 20 hours. The genus of Mycobacterium is defined by the mycolic acids and waxes, which makes the bacterium resistant to many bactericidal agents. For this reason, the tuberculosis disease can be easily spread due to the difficulty in killing the bacteria. Mycobacterium tuberculosis is very diverse and provides different geographic areas with different disease symptoms [2].
Pathogenesis
Transmission
Much too contrary belief, the only method by which tuberculosis (TB) is spread, is through airborne particles from person to person. If a healthy human were to breathe in the bacteria that escaped the lungs of an infected individual who coughed, sneezed, or even spoke, they will contract the disease. With Mycobacterium tuberculosis being able to colonize and affect many different parts of the body, the only contagious form of the disease is pulmonary tuberculosis [3].
Infectious Dose, Incubation, and Colonization
Mycobacterium tuberculosis has an incredibly low infectious dose of less than 10 [3], as well as a long incubation period of two to twelve weeks [5]. Mycobacterium tuberculosis that infects the lungs is inhaled by the host and engulfed by the macrophages of the alveoli. These bacteria can now lay dormant or begin to reproduce inside the macrophages, which triggers the infection to occur.
Epidemiology
Tuberculosis is a disease that must be reported to the CDC when a positive diagnosis has been reached. It is due to this reason that the CDC has the exact numbers on incidences in the United States from 1953-2011. It has been stated that TB is one of the deadliest diseases in the world. According to the CDC, approximately one-third of the entire population is infected with Mycobacterium tuberculosis. There were close to 9 million people in the world diagnosed with TB disease in 2011, and 1.4 million deaths were related to tuberculosis infection or disease. Of these 9 million people with tuberculosis disease 10,528 were in the United States. With HIV leaving its host immunocompromised, they are unable to cope with this disease, leaving TB as the number one killer of HIV positive patients [3].
Virulence Factors
Clinical Features and Symptoms
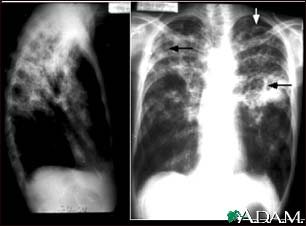
There are multiple forms of tuberculosis which is separated into two categories; pulmonary and extrapulmonary tuberculosis. It is important to note due to its slow development, TB symptoms can take months to years to begin. If the tuberculosis bacteria invades the body without causing symptoms it is considered latent, whereas active TB causes symptoms to arise.
Pulmonary TB symptoms include:
- More than three weeks of chronic coughing in which phlegm is present. It is not abnormal for blood to be present in the phlegm
- Shortness of breath, which will continue to worsen as the disease worsens
- Weight loss due to a loss of appetite
- Excessive sweating while sleeping
- Intense lack of energy
- Body aches and pains that have occurred for greater than three weeks
Extrapulmonary TB diseases and symptoms include:
Lymph Node Tuberculosis
- Painless lymph node swelling; any nodes in the body can be affected, but the most common place is the neck
- The constant swelling of the lymph nodes causes the fluid to eventually leak through the barrier of the skin
Skeletal Tuberculosis (Pott’s Disease)
- Painful bones
- The infected bone will begin to weaken and become curved
- Absence of feeling and movement in the diseased bone
- Due to the bone being weakened, it has a high risk of being fractured
Gastrointestinal Tuberculosis
- Diarrhea
- Bleeding from the rectum
- Pain in the abdominal region
Genitourinary Tuberculosis
- Urethral burning while urinating
- Presence of blood in urine
- Persistent need to urinate
- Aches and pain in the groin
Central Nervous System Tuberculosis
- Presence of headaches
- Brain swelling
- Neck stiffness
- Illness
- Decrease in vision
- Deterioration in mental awareness
- Onset of seizures [1]
Diagnosis
If the patient is experiencing the symptoms described above it is highly likely they will be tested for the presence of Mycobacterium tuberculosis in their body. The evaluation process for a disease as serious as tuberculosis is a daunting one, but physicians need to be absolutely sure to produce a proper diagnosis. The steps for diagnosing a patient presenting with symptoms similar to TB include:
- Obtaining the patients’ medical history: Health care providers must determine if the patient has been exposed to TB, as well as illnesses that leave the patient immunodeficient. Demographic, such as age and occupation are important factors in determine if the patient is in an at risk group for contracting TB.
- A thorough physical examination: This can allow for health care providers to asses overall health and knowledge that will lead to the treatment, if the patient is determined to be infected with Mycobacterium tuberculosis.
- Testing for the presence of Mycobacterium tuberculosis: The two most common tests are the Mantoux tuberculin skin test (TST) and the TB blood test. The TST is accomplished by injecting 1/10th of a milliliter (mL) of tuberculin is injected into the patient’s skin, usually in the mid forearm. 48-72 after the injection, a health care provider reads the test and documents the results. If there is no reaction, the test is considered negative, however if redness and swelling occur the presentation of the reaction determines if a test is considered positive or not. 5 mm of hard swelling will be considered positive if the patient:
- Has been diagnosed with HIV
- Is immunodeficient
- Has ever had an organ transplant
- Has come into contact with someone who has active TB
- Has worsening chest X-Rays
- Has presented with a negative test within 2 years
- Has a condition that increases their chances of contracting TB
- Is a health care professional
- Is an intravenous (IV) drug user
- Immigrants from a country with a high rate of TB who moved to the United States less than 5 years ago
- Is under the age of four years old
- Is exposed to high risk adults, and are infants, children, or teenagers
- Is frequently in an area of high TB risk, such as homeless shelters and jails
- Chest X-Ray or more in depth studies if needed: This is not a test that can allow a physician to diagnose a patient with TB, but can rule out pulmonary TB if a patient has presented with a positive TST or blood test.
- Culturing of the samples taken from the patient: This method of culturing the bacteria is the only definitive way to diagnose a patient with a Mycobacterium tuberculosis infection. All positive results of this test must be reported to the primary care physician and the state.
- Testing the Mycobacterium tuberculosis for drug resistance, due to possibility of having drug resistant tuberculosis (MDR TB) or worse, extremely drug resistant tuberculosis (XDR TB): This is incredibly important because if the M. tuberculosis strain is resistant, then an appropriate regiment needs to be prescribed to the patient to ensure the best scenario of curing the disease [3].
10 mm or greater of hard swelling will be considered positive if the patient:
Any test with results 15 mm or larger of hard swelling will be considered positive whether is patient is at risk or not [4].
Treatment
Prevention
Host Immune Response
References
1 Conway, Tyrrell. “Genus conway”. “Microbe Wiki” 2013. Volume 1. p. 1-2.
2 NHS General Information on Tuberculosis
3 Ozimek, Maleana Mycobacterium tuberculosis
4 CDC General Information on Tuberculosis
5 PPD skin test Medline Plus
6 Exposure to Tuberculosis Vanderbilt Occupational Health Clinic
7 Davidson College Pathogen Life Cycle
Created by Jennifer Gallup, student of Tyrrell Conway at the University of Oklahoma.

