Tuberculosis in Children in Developing Countries: Difference between revisions
| Line 28: | Line 28: | ||
<br>Include some current research in each section.<br> | <br>Include some current research in each section.<br> | ||
Recent research in Africa has confirmed the likelihood that a child will contract pulmonary Tuberculosis if an adult in the household carries the disease. The children were studied in South Africa where there is a low average economic income and high prevalence of Tuberculosis [2]. Initially, 53% of the 125 children were infected with the bacteria but only 11% had developed Tuberculosis disease. [2]. After the 30 month period the number infected with Tuberculosis stayed fairly constant at 54% while the number with the disease rose to 24% [2]. The results proved that children have a 76% chance of being infected with Tuberculosis if they live with an adult with a smear positive Tuberculosis case [2]. During this particular study, treatments for Tuberculosis infection were also studied. The children who had never been treated for a Tuberculosis infection were given a chemoprophylaxis, which is a preventative treatment for Tuberculosis [2]. If a child had received previous chemoprophylaxis treatments, he or she was given a different 4 to 5 drug combination to treat the tuberculosis. The chemoprophylaxis treatment required the child’s parents or caregivers to take them to the clinic 5 days per week for treatment and observed therapy [2]. This kind of treatment proved to be successful because of the 41 children that received chemoprophylaxis treatment, 29 children tested negative for tuberculosis [2]. Public health organizations and workers should promote funding for preventative medications for children because they were effective in protecting children who were continually exposed to tuberculosis. However there are a number of limitations for developing countries in preventing tuberculosis infections. In order for treatment to be effective, parents or caregivers must bring their children to a clinic very frequently which is often difficult due limitations such as type of employment and transportation availability. In addition, many of the drugs required for preventative chemoprophylaxis are quite expensive and their use in developing nations would require funding from a higher income country or non-governmental organization. | Recent research in Africa has confirmed the likelihood that a child will contract pulmonary Tuberculosis if an adult in the household carries the disease. The children were studied in South Africa where there is a low average economic income and high prevalence of Tuberculosis [2]. Initially, 53% of the 125 children were infected with the bacteria but only 11% had developed Tuberculosis disease. [2]. After the 30 month period the number infected with Tuberculosis stayed fairly constant at 54% while the number with the disease rose to 24% [2]. The results proved that children have a 76% chance of being infected with Tuberculosis if they live with an adult with a smear positive Tuberculosis case [2]. During this particular study, treatments for Tuberculosis infection were also studied. The children who had never been treated for a Tuberculosis infection were given a chemoprophylaxis, which is a preventative treatment for Tuberculosis [2]. If a child had received previous chemoprophylaxis treatments, he or she was given a different 4 to 5 drug combination to treat the tuberculosis. The chemoprophylaxis treatment required the child’s parents or caregivers to take them to the clinic 5 days per week for treatment and observed therapy [2]. This kind of treatment proved to be successful because of the 41 children that received chemoprophylaxis treatment, 29 children tested negative for tuberculosis [2]. Public health organizations and workers should promote funding for preventative medications for children because they were effective in protecting children who were continually exposed to tuberculosis. However there are a number of limitations for developing countries in preventing tuberculosis infections. In order for treatment to be effective, parents or caregivers must bring their children to a clinic very frequently which is often difficult due limitations such as type of employment and transportation availability. In addition, many of the drugs required for preventative chemoprophylaxis are quite expensive and their use in developing nations would require funding from a higher income country or non-governmental organization. | ||
Multidrug-resistant tuberculosis in India is becoming a major global health issue because nearly 2 million new cases are detected each year [1]. Many adults have been carefully observed and given short course treatments known as DOTS (directly observed treatment)[1]. However, there has been little done in India to prevent and treat tuberculosis infection in children. It is likely that children in larger cities in India, such as Mumbai, live in overcrowded conditions and are frequently subjected to tuberculosis and multidrug -resistant strains of tuberculosis [1]. Since children often test negative for acid-fast bacilli, it is difficult for public health workers to determine how many are living with tuberculosis [10]. Economic limitations prevent children from receiving more diagnostic tests to determine if they have tuberculosis. Another factor that is affecting the development of multidrug-resistant tuberculosis in children is AIDS. HIV and AIDS make any individual more likely to acquire a tuberculosis infection [1]. Researchers have found that most individuals are not able to purchase antiretroviral therapy for their children but may be able to afford a combination of drugs that help fight tuberculosis [1]. The most common drug mixture includes isoniazid, rifampicin, pyrazinamide, and ethambutol [1]. This treatment option will help prevent tuberculosis from developing in children with HIV or AIDS, but will not protect them from multidrug-resistant tuberculosis [1]. Other public health strategies for the prevention of tuberculosis in children involves steps to reduce the maternal transmission of HIV [ 1]. If the number of pediatric cases of HIV could be reduced, a child’s likelihood of developing tuberculosis would be greatly reduced. | Multidrug-resistant tuberculosis in India is becoming a major global health issue because nearly 2 million new cases are detected each year [1]. Many adults have been carefully observed and given short course treatments known as DOTS (directly observed treatment)[1]. However, there has been little done in India to prevent and treat tuberculosis infection in children. It is likely that children in larger cities in India, such as Mumbai, live in overcrowded conditions and are frequently subjected to tuberculosis and multidrug -resistant strains of tuberculosis [1]. Since children often test negative for acid-fast bacilli, it is difficult for public health workers to determine how many are living with tuberculosis [10]. Economic limitations prevent children from receiving more diagnostic tests to determine if they have tuberculosis. Another factor that is affecting the development of multidrug-resistant tuberculosis in children is AIDS. HIV and AIDS make any individual more likely to acquire a tuberculosis infection [1]. Researchers have found that most individuals are not able to purchase antiretroviral therapy for their children but may be able to afford a combination of drugs that help fight tuberculosis [1]. The most common drug mixture includes isoniazid, rifampicin, pyrazinamide, and ethambutol [1]. This treatment option will help prevent tuberculosis from developing in children with HIV or AIDS, but will not protect them from multidrug-resistant tuberculosis [1]. Other public health strategies for the prevention of tuberculosis in children involves steps to reduce the maternal transmission of HIV [ 1]. If the number of pediatric cases of HIV could be reduced, a child’s likelihood of developing tuberculosis would be greatly reduced. | ||
Revision as of 20:03, 5 December 2009
Introduction
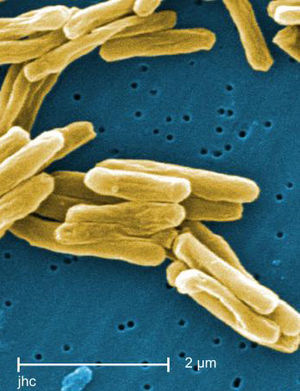
Tuberculosis is caused by the bacteria Mycobacterium tuberculosis and is a highly contagious disease. Today, most Tuberculosis cases are found in low -income regions like Southeast Asia and Africa. Southeast Asia has one of the highest incidence rates of Tuberculosis and contains nearly 34% of all cases worldwide [5]. It is also estimated that in every 100,00 people living in Sub-Saharan Africa 350 are living with Tuberculosis [5]. The presence of Tuberculosis in children is an important indicator of the overall status of health in a particular country. In most cases, Tuberculosis in children can be traced back to an adult host [4]. In many developed nations, Tuberculosis can be treated fairly easily with antibiotics. However, emerging strains of multi-drug resistant stands of Tuberculosis pose a major treat to the health of all populations, especially children. Public health strategies are crucial to controlling Tuberculosis because access in developing countries to effective antibiotics is limited. Children react different to Tuberculosis because their immune systems are still in a developmental state [4]. It is crucial that Tuberculosis in children is carefully controlled in developing countries so that a drug resistant strain does not cause another major worldwide epidemic.
To start your own paper: Type your page title into the Search box. (Be sure to spell correctly.) Press "Go." The site will offer you the opportunity to "Create this page."
Next, use the "edit" tab to reveal the coded file of BIOL 191 Paper 2009. Select all and copy; paste into the edit window of your own page. (Do not try to edit the class page.)
Introduce the topic of your paper. What public health question do you raise? Whose health is affected; in what country or location? What disease organisms are involved?
Below are some sample codes that will be useful for your paper.
To upload an image: Use "Upload File" (in margin at left)
To make the image appear, you need to embed image insertion code (see sample at right). The insertion code consists of:
Double brackets: [[
Filename: PHIL_1181_lores.jpg
Thumbnail status: |thumb|
Pixel size: |300px|
Placement on page: |right|
Legend/credit: Electron micrograph of the Ebola Zaire virus. This was the first photo ever taken of the virus, on 10/13/1976. By Dr. F.A. Murphy, now at U.C. Davis, then at the CDC.
Closed double brackets: ]]
Other examples:
Bold
Italic
Subscript: H2O
Superscript: Fe3+
Diagnosis
Include some current research in each section.
Treatment
Include some current research in each section.
Public Health Strategies and Case Studies
Include some current research in each section.
Recent research in Africa has confirmed the likelihood that a child will contract pulmonary Tuberculosis if an adult in the household carries the disease. The children were studied in South Africa where there is a low average economic income and high prevalence of Tuberculosis [2]. Initially, 53% of the 125 children were infected with the bacteria but only 11% had developed Tuberculosis disease. [2]. After the 30 month period the number infected with Tuberculosis stayed fairly constant at 54% while the number with the disease rose to 24% [2]. The results proved that children have a 76% chance of being infected with Tuberculosis if they live with an adult with a smear positive Tuberculosis case [2]. During this particular study, treatments for Tuberculosis infection were also studied. The children who had never been treated for a Tuberculosis infection were given a chemoprophylaxis, which is a preventative treatment for Tuberculosis [2]. If a child had received previous chemoprophylaxis treatments, he or she was given a different 4 to 5 drug combination to treat the tuberculosis. The chemoprophylaxis treatment required the child’s parents or caregivers to take them to the clinic 5 days per week for treatment and observed therapy [2]. This kind of treatment proved to be successful because of the 41 children that received chemoprophylaxis treatment, 29 children tested negative for tuberculosis [2]. Public health organizations and workers should promote funding for preventative medications for children because they were effective in protecting children who were continually exposed to tuberculosis. However there are a number of limitations for developing countries in preventing tuberculosis infections. In order for treatment to be effective, parents or caregivers must bring their children to a clinic very frequently which is often difficult due limitations such as type of employment and transportation availability. In addition, many of the drugs required for preventative chemoprophylaxis are quite expensive and their use in developing nations would require funding from a higher income country or non-governmental organization.
Multidrug-resistant tuberculosis in India is becoming a major global health issue because nearly 2 million new cases are detected each year [1]. Many adults have been carefully observed and given short course treatments known as DOTS (directly observed treatment)[1]. However, there has been little done in India to prevent and treat tuberculosis infection in children. It is likely that children in larger cities in India, such as Mumbai, live in overcrowded conditions and are frequently subjected to tuberculosis and multidrug -resistant strains of tuberculosis [1]. Since children often test negative for acid-fast bacilli, it is difficult for public health workers to determine how many are living with tuberculosis [10]. Economic limitations prevent children from receiving more diagnostic tests to determine if they have tuberculosis. Another factor that is affecting the development of multidrug-resistant tuberculosis in children is AIDS. HIV and AIDS make any individual more likely to acquire a tuberculosis infection [1]. Researchers have found that most individuals are not able to purchase antiretroviral therapy for their children but may be able to afford a combination of drugs that help fight tuberculosis [1]. The most common drug mixture includes isoniazid, rifampicin, pyrazinamide, and ethambutol [1]. This treatment option will help prevent tuberculosis from developing in children with HIV or AIDS, but will not protect them from multidrug-resistant tuberculosis [1]. Other public health strategies for the prevention of tuberculosis in children involves steps to reduce the maternal transmission of HIV [ 1]. If the number of pediatric cases of HIV could be reduced, a child’s likelihood of developing tuberculosis would be greatly reduced.
Conclusion
Overall paper length should be approximately 2,000 to 2,500 words.
Include at least two data figures.
Use professional sources, including at least two research studies.
References
[1] "Children and Multi-drug Resistant Tuberculosis in Mumbai (Bombay), India" Centers for Disease Control and Prevention
[2] Schaaf, Simon H., Robert P. Gie, Magdalene Kennedy, Nulda Beyers, Peter B. Hesseling and Peter R. Donald. " Evaluation of Young Children with Adult Multidrug Resistant Tuberculosis: A 30 Month Followup" 2002;109;765-771Pediatrics.
[3] Shingadia D, Novelli V. "Diagnosis and treatment of tuberculosis in children" Department of Academic Child Health, St Barthlomews and The London Medical and Dental School, Queen Mary, University of London, UK
[4] "Tuberculosis" Baylor School of Medicine.
[5] "Tuberculosis" World Health Organization
[6] "TUBERCULOSIS IN A CHILD – SEARCH FOR THE INFECTED ADULT NEARBY" Eurosurveillance
Edited by student of Joan Slonczewski for BIOL 191 Microbiology, 2009, Kenyon College.