Amoebiasis
Introduction
Background Information
First identified by Hippocrates around 300 B.C. by describing a patient with dysentery and fever, amoebiasis is a gastrointestinal infection due to the amoeba, Entamoeba histolytica. Later developments came in 1855 when it was suggested that the disease might have a parasitic origin. Finally, E. histolytica was identified from a stool sample in 1875 by Fredor Losch. Throughout the world, amoebiasis is the second leading cause of death from a parasitic disease with an estimated 50 million cases per year and 100,000 deaths per year. However, most of these cases occur in the developing world. Although it is the second leading cause of death from parasitic diseases, about 90% of the people exposed to E. histolytica are asymptomatic or report very mild symptoms. [5]

E. histolytica secretes proteinases that do considerable damage to their host. They produce proteolytic enzymes and cysteine proteases that aid in their ability to invade tissues. They can dissolve the tissues of the host and can kill the host cells on contact. The proteinases immobilize the cells and cause them to lose their cytoplasmic granules and structures. Finally, the nucleus of the cell will disintegrate. E. histolyticacan also engulf the red blood cells of the host. [3]
For those that do experience the symptoms associated with the Entamoeba histolytica infection, the onset is variable; they can occur gradually or very quickly. Gradual symptoms most often include a slow onset of colitis, or inflammation of the colon. Associated with colitis is diarrhoea and abdominal pain. Diarrhoea usually begins mildly and develops into diarrhoea that contains blood and mucous. Other signs of colitis are nausea, headache, and sometimes fever, but fever only occurs in less than forty percent of individuals. On the other hand, symptoms that occur quickly and intensely include semi liquid stools that contain blood and mucous. Abdominal pain can range from mild to severe, frequently accompanied by a tender liver. Rarer progressions of the disease include brain abscesses and respiratory issues.

Prognosis
Mortality rates from the infection also vary widely depending on what organs E. histolytica attacks. If the individual develops fulminant amoebic colitis, there is an associated mortality rate of between 55% to 87.5%. If amoebic liver-abscess occurs, which is also the most common path the disease takes outside of the intestines, mortality rates are generally from 1-3%. Death comes quickly to about half of individuals who develop amoebic brain abscesses.
Transmission
Entamoeba histolytica can be transmitted a number of ways, but most commonly is it transferred from fecal matter, where E. histolytica cysts are present, to oral ingestion. It is also transmitted from contaminated food or water sources, which are common in places such as Mexico, Central America, and South Asia. Some researchers have suggested a zoonosis pathway may also exist, but further studies still need to be conducted to prove this. [3]
Entamoeba histolytica Structure and Lifecycle
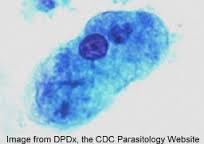
While existing in the cyst stage of its life cycle, E. histolytica tend to have a diameter of 10–15μm and are round in shape. Within a chitinous refractile wall are four nuclei, glycogen, and chromatoid bodies (ribosomal assemblies). As a trophozoite, E. histolytica are generally larger, of around 10 to 50μm in diameter. Unlike in the cyst form, the trophozoites are capable of moving spontaneously, gaining the energy for this process through anaerobically converting glucose and pyruvate to ethanol.
Once ingested by a human or a non-human primate, who are the natural hosts to the parasite, the E. histolytica cysts travel to the small intestine and become trophozoites in either the terminal ileum or colon (each cyst will produce eight trophozoites). Cysts can exist outside the human body for long periods of time (from days or even up to months in damp conditions and ideal temperatures). Unlike cysts, trophozoites cannot survive outside of this preferred environment, and will degrade very quickly if exposed to an outside environment. The incubation period of the amoeba can vary from a couple of days to as long as a year. Nonetheless, once in the small intestine, the trophozoites will attack the intestinal epithelial cells of the gastrointestinal tract. Not only do they invade the gastrointestinal track, but trophozoites can also migrate to other organs of the body and cause infection there as well. Once in the colon of its host, the trophozoites will encyst again and exit the body through the stool. [5]
Treatment
The first successful treatment came about in 1912. Leonard Rogers used emetine. [5] Today, those identified as infected by E. histolytica are treated with two types of drugs. The first is an amoebicidal agent as well as a luminal-acting cysticidal agent. Physicians will usually use a CT to monitor the abdomen of an infected individual and use a catheter to drain fluid. People with the identified infection that do not show symptoms should still be put on a luminal agent since they pose a health risk to others. [2] Furthermore, 4-10% of asymptomatic people will develop symptoms within a year of the infection. [3]
Development of Diagnoses Methods
It is important to have as precise methods as possible in detecting E. histolytica in order to determine the extent of the amoebiasis infection. Furthermore, the more that is understood about E. histolytica, the better researchers are able to develop treatments. Currently, the methods that are most commonly used to detect the presence of the parasite are ELISA (enzyme-linked immunosorbent assay) or IHA (indirect hemagglutination assay).
Before the introduction of advanced methods, E. histolytica has historically been detected by looking at morphology under a microscope. It is difficult though, to detect morphological differences in protozoa because many of them look very similar. Furthermore, it hard to distinguish between E. histolytica and E. dispar using old methods as well. The only way one could distinguish between the two was if erythrophagocytosis, or the ingested RBCs in the trophozites of E. histolytica, was seen under a microscope. And even this method is not always conclusive as other amebic infections have RBCs, although they are not observed as frequently. Thus, it is important that new diagnosis techniques are being developed. In recent years there have been many advancements in detection.
Now, serological testing is more a useful and definitive way of testing for the presence of E. histolytica. This, coupled with antigen detection and PCR, may offer the best way to diagnose patients. ELISA (enzyme-linked immunosorbent assay) are becoming increasingly popular in diagnoses because symptomatic patients are thought to have high levels of specific antibodies, serum anti-lectin immunoglobulin G (IgG), associated with the E. histolytica infection. These antibodies can be detected within one week of the start of the symptoms. Although PCR and serological testing might be useful in the developed world, these resources are not as readily available in undeveloped countries. Thus, these are impractical methods for the parts of the world where the parasite is most prevalent and researchers are currently working on developing new methods to test for the the infection. [5]
Genomic Diversity of Amoebiasis
Research on the genome of E. histolytica is an emerging area of importance in understanding the virulence of the parasite. In fact, recent studies have proposed that it's genetic factors affect how infectious it is. The genomes of several strains of E. histolytica have been sequenced, which yielded interesting data about the amoeba. For example, it was discovered that about 75% of the genome consists of A and T nucleotides. Furthermore, among the strains sequenced nucleotide differences were low (single-nucleotide polymorphism ranged from 0.312 to 0.857 SNPs per kilobase). Conversely, other studies have found high diversity in the nucleotide repeats that separate tRNA genes or genes like that coding for SREHP, a protein consisting of a large amount of serine. However, gene copy number is diverse, suggesting that this could be an important part of the variety of virulence seen from the parasite.
Recent research provides evidence that E. histolytica reproduces sexually, a phenomena that has not yet been observed in the genus, Entamoeba. It was discovered that the particular strain of E. histolytica, HM-1:IMSS, contains most of the genes that contribute to meiosis. Thus, sexual reproduction probably provides a significant amount of the diversity observed in the genomes of the strains through events such as recombination and reassortment of alleles. [1]
Conclusion
Amoebiasis is an infection affecting millions of people a year. It is important that research be focused in diagnosing patients in places like India, tropical regions of Africa, Mexico, and other areas of Central America, where it is most commonly seen and where contaminated food and water are commonplace. [5] It is important that the drug regiments are made available to these nations which will dramatically decrease the number of deaths that E. histolytica causes.
References
[2] Powell, S. J. "New developments in the therapy of amoebiasis"
[4] Stanley, S. L."The Lancet" "Amoebiasis" March 2003 Volume 361, Issue 9362, p. 1025–1034.
[5] Petri, W., Tanyuskel, M. ""Laboratory Diagnosis of Amebiasis"
Edited by Kelsey Hauser, student of Joan Slonczewski for BIOL 116 Information in Living Systems, 2013, Kenyon College.