Aspergillus fumigatus and Aspergillosis

Etiology/Bacteriology
Taxonomy
Superkingdom = Eukaryota | Kingdom = Fungi | Subkingdom = Dikarya | Phylum = Ascomycota | Subphylum = Pezizomycotina | Class = Eurotiomycetes | Subclass = Eurotiomycetidae | Order = Eurotiales | Family = Aspergillaceae | Genus = Aspergillus | Species = A. fumigatus[1]
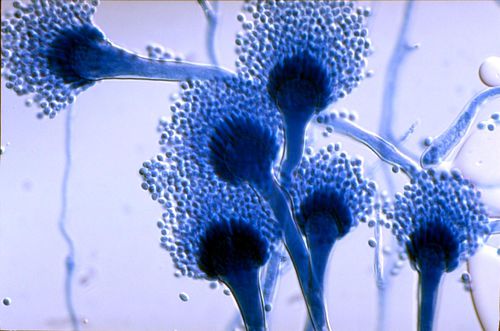
Description
Aspergillus fumigatus, a saprophytic fungus, can opportunistically cause a multitude of diseases in humans [2]. A. fumigatus, which primarily lives in soil and decaying vegetation, can be dispersed through the air as asexual spores, known as conidia. Because of this, humans usually get infected with the fungus by inhaling these conidia. In a given day someone inhales an average of 200 A. fumigatus spores [2]. In heathy individuals, the innate immune system kills all of the conidia that the body encounters; however, in immunocompromised individuals A. fumigatus infection is a serious concern.
Invasive aspergillosis (IA), which is primarily caused by A. fumigatus, is very severe and life-threatening infectious disease [3]. If left untreated, it is almost nearly deadly, usually resulting in intense pneumonia [16]. The innate immune system usually removes all the A. fumigatus conidia; however, in imunocompromised patients, such as those experiencing neutropenia, caused by chemotherapy, or those on prolonged cortocoidsteroids due to organ transplant, are at greater risk of developing the infection [2].
Clinical Features
Symptoms
Symptoms of invasive aspergillosis (IA) are wide ranging, but patients generally experience chest pain, cough, malaise, weight loss, dyspnea and fever [15]. However, patients could experience any number of these symptoms. For example, individuals with AI who were previously treated with corticosteroids do not have elevated temperatures. If left untreated symptoms vary depending on where the infection has spread [16]. If left untreated, patients with IA will inevitably develop fatal cases of pneumonia.
High Risk Groups
Groups at risk of developing invasive aspergillosis (IA) include patients recieving hematopoietic stem cell transplants or solid-organ transplants [16]. Patients that went through irradiation therapy or who suffer from neutropenia, which is usually caused by chemotherapy, are also at risk [2]. Corticosteroid therapy, which is used to treat graft-versus-host disease, is also a common cause of IA. People born with autoimmune diseases like chronic granulomatous disease (CGD), who can not make reactive oxygen species, can also develop IA [15].
Treatment
Today, the most effective drug used in primary treatment of IA is voriconazole [16]. Although, drug resistance to azoles is of increasing concern, with up to five percent of cases showing signs of resistance [17]. Drug combinations of voriconazole and D-AMB or other anti-fungals are not uncommon [16]. However, voriconazole and D-AMB are the only drugs licensed for primary treatment of IA in the United States. In all cases, drug monitoring is necessary due to the variability in effectiveness in different patients. In rare cases, surgery is used to remove the infected tissue, although this is risky since patients with IA are already very ill. As a preventative measure, patients at high risk of developing IA can be given anti-fungal drugs like aerosolized liposomal amphotericin B [18]. The key to treatment of invasive aspergillosis (IA) is early detection [15]. In one study, the mortality rate of patients receiving eight or less days of anti-fungal drugs was one hundred percent.
Pathogenesis
Life Cycle
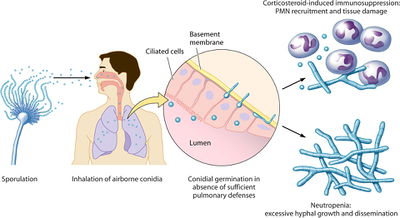
Aspergillus fumigatus seems to live a fairly simple infectious life cycle, as seen in Figure 1 [2]. Asexual sporulation results in the inhalation of tiny spores, called conidia. In immunosuppressed patients, these conidia begin to germinate, leading to the formation of hyphae. Expecially true in patients with neutropenia, hyphae will continue to grow, until dissemination occurs. Recently, it has been shown that Aspergillus fumigatus do indeed participate in sexual reproduction [9]. The A. fumigatus life cycle may resemble the closely related A. nidulans, which is shown in Figure 2 [10].

Transmission
Aspergillus fumigatus is primarily transmitted through the inhalation of fungal spores, called conidia [2]. A. fumigatus conidia can be found ubiquitously in both indoor and outdoor environments, so people are continuously inhaling the fungi. The continued presence of A. fumigatus is usually not a problem; however, without proper respiratory tract immune defenses infection can occur.
Invasion of Host Lung Epithelium
Conidia can begin to infect epithelial cells in several ways, the easiest of which is through the targeting of damaged cells [8]. Epithelial cells that have been damaged by immunosuppressive therapies, such as irradiation and chemotherapy, aid in conidial colonization. Corticosteroids and other anti-inflammatory medication also increase the risk of conidial colonization of the epithelia. In order for Aspergillus fumigatus to colonize the respiratory tract, it must first evade the innate immune system, which is usually very effective at removing the pathogen in healthy individuals [2]. Gliotoxin, helvolic acid, and fumagillin are believed to help slow ciliary beat frequency, which likely interferes with mucociliary clearance. A. fumigatus conidia that survive mucociliary clearance bind to damaged respiratory epithelial cells and the basement membrane using sialic acid residues [4]. Sialic acid residues are likely required for parthenogenesis, since pathogenic species of aspergilli have more sialic acid residues. After binding to the epithelial cells, the conidia are engulfed into a phagosome where the conidia can begin to germinate [5]. A. fumigatus has also been shown to inhibit apoptosis in a variety of epithelial cells. A variety of proteases secreted by A. fumigatus help it to colonize neighboring healthy lung tissue [2]. Elastase is particularity important for the degradation of host tissues since elastin makes up a large percentage of the tissues in the lungs.
Macrophage Evasion
Patients in at risk groups for AI have reduced alveolar macrophage effector functions, which contributes to A. fumigatus's capacity to evade macrophage killing [2].A. fumigatus triggers an inflammatory response only after its conidia begin germinating [6]. Macrophages can only recognize A. fumigatus conidia when beta(1,3)-glucan is displayed on the surface the conidial surface. This carbohydrate, which is hidden behind an outer layer of the cell wall, binds to dectin-1 on the surface of alveolar macrophages, triggering phagocytosis, macrophage activation, and inflammation. Resting conidia can also resist macrophage killing thanks to the pigment melanin and other enzymes such as superoxide dismutases, which act as reactive oxygen species (ROS) scavengers [2].
Dissemination
As Aspergillus fumigatus hyphae grow, they begin to invade host endothelial cells, which line the blood vessels near the lungs [13]. Initially, the hyphae are located on the outside of the vessel and move through the cells towards the interior of the blood vessel. When the hyphae reach the blood, fragments can break off and begin circulating in the blood stream. Once in the blood, these hyphal fragments can adhere to the luminal side of other endothelial cells and grow towards the abluminal side. This differential hyphael growth, towards and away from the lumen, is accomplished using different mechanisms. Hyphael growth into a blood vessel without triggering the growth of endothelial cell pseudopods [14]. Also, growth towards the lumen caused less host cell tissue damage than growth leaving the blood vessel. Aspergillus fumigatus dissemination is clearly very serious. After the pathogen gains access to the blood stream, it is nearly impossible to stop it from growing all over the body.
Host Immune Response

As seen in figure 3, Aspergillus fumigatus is an opportunistic pathogen that only infects patients with compromised immune systems [2]. Usually, patients with a robust innate immune response are able to destroy the A. fumigatus pathogen without any problems. However, patients in the high risk groups, are especially susceptible to A. fumigatus infection and should take precautions against getting aspergillosis.
Innate Immune Response
A. Fumigatus begins its life cycle with asexual reproduction, producing airborne spores, called conidia [2]. If these spores are inhaled by individual with a properly working immune system, the spores rarely make it all the way to the bronchioles and alveoli. The conidia first encounter the mucosa that lines the respiratory tract, where complement is activated. The overwhelming majority of the spores are removed via mucociliary clearance. those that survive make their way to the aveoli where they are phagocytized by aveolar macrophages. Alveolar macrophages are the main phagocytic cells in the respiratory tract [2]. When PRRs on the surface of the macrophages recognize pathogen-associated molecular patterns (PAMPs) on the surface of the conidia, an inflammatory response is triggered. One PRR, dectin-1, recognizes the fungal cell wall carbohydrate beta(1,3)-glucan. Dectin-1 cannot recognize resting conidia however, since beta(1,3)-glucan is hidden behind another layer of the cell wall until germination begins [6]. By only recognizing beta(1,3)-glucan, the innate immune system can ensure that an inflammatory response is only triggered by actively germinating spores, which are more likely to be pathogenic. After engulfing the pathogen, the alveolar macrophage uses reactive oxidant species (ROS) to kill the conidia [7]. After macrophage activation, polymorphonuclear neutrophils (PMN) are recruited to the infection site [8]. Interaction between these neutrophils and A. fumigatus hyphea result in the secreation of ROS and other enzymes to help destroy the pathogen. Neutrophils are not very effective at killing conidia, but some studies have suggested that they help inhibit conidial germination by forming aggregates in the lung [2]. Recruitment of natural killer (NK) cells by chemokines is also critical to the host innate immune response to A. fumigatus infection [12]. These cells act similarly to cytotoxic T cells, seeking out infected cells and directly killing them. All together, the innate immune system is responsible for the majority of the host defenses against Aspergillus fumigatus and invasive aspergillosis.
Adaptive Immune Response
The adaptive immune response to Aspergillus fumigatus infection begins in the respiratory mucus, where dendritic cells first come into contact with the pathogen [11]. Unlike macrophages, which can only engulf conidia, dendritic cells phagocytize both A. fumigatus conidia and hyphae. Dendritic cells phagocytize conidia and hyphae through coiling phagocytosis and zipper-type phagocytosis mechanisms, respectably. After phagocytizing conidia, a dendritic cell will begin producing the cytokine IL-12. Alternatively, it will produce cytokines IL-4 and IL-10 after engulfing hyphae. Dendritic cells then travel to the nearest peripheral lymphoid organ, where they meet up with a naive T cell. The differential production of cytokines help control what type of helper T cell the naive T cell will become. Production of IL-12 induces maturation into a T helper I cell, while IL-4 and IL-10 signal the cell to differentiate into a T helper II cell.
References
1. UniProt. Taxonomy: Species Aspergillus fumigatus. Available at http://www.uniprot.org/taxonomy/746128.
2. Dagenais T. and Keller N. Pathogenesis of Aspergillus fumigatus in Invasive Aspergillosis. Clin Microbial Rev. doi: 10.1128/CMR.00055-08. http://cmr.asm.org/content/22/3/447.full.
3. Tekaia F. and Latge JP. Aspergillus fumigatus: saprophyte or pathogen?. Current Opinion in Microbiology. doi: 10.1016/j.mib.2005.06.017. http://www.sciencedirect.com/science/article/pii/S1369527405000925.
4. Washylnka J., Simmer M., and Moore, M. Differences in sialic acid density in pathogenic and non-pathogenic Aspergillus species. Microbiology. http://mic.sgmjournals.org/content/journal/micro/10.1099/00221287-147-4-869?crawler=true&mimetype=application/pdf.
5. Washylnka J., and Moore M. Aspergillus fumigatus conidia survive and germinate in acidic organelles of A549 epithelial cells. J. Cell Sci.. http://jcs.biologists.org/content/116/8/1579.long.
6. Hohl T, et al. Aspergillus fumigatus Triggers Inflammatory Responses by Stage-Specific beta-Glucan Display. PLoS Pathog. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1287910/.
7. Philippe B, et al. Killing of Aspergillus fumigatus by Alveolar Macrophages Is Mediated by Reactive Oxidant Intermediates. Infection and Immunity. doi: 10.1128/IAI.71.6.3034-3042.2003. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC155721/.
8. Latge JP. Aspergillus fumigatus, a saprotrophic pathogenic fungus. Mycologist. doi: 10.1017/S0269915X0300209X. http://www.davidmoore.org.uk/Assets/fungi4schools/Reprints/Mycologist_articles/Post-16/Medical/V17pp056-061asp-fumigatus.pdf.
9. O'Gorman C, Fuller H, and Dyer P. Discovery of a sexual cycle in the opportunistic fungal pathogen Aspergillus fumigatus. Nature. doi: 10.1038/nature07528. http://www.nature.com/nature/journal/v457/n7228/full/nature07528.html.
10. Casselton L and Zolan M. The art and design of genetic screens: filamentous fungi. Nat Rev Genetics. doi: 10.1038/nrg889. http://www.nature.com/nrg/journal/v3/n9/full/nrg889.html.
11. Bozza S, et al. Dendritic Cells Transport Conidia and Hyphae of Aspergillus fumigatus from the Airways to the Draining Lymph Nodes and Initiate Disparate Th Responses to the Fungus. J Immunol. doi: 10.4049/jimmunol.168.3.1362. http://www.jimmunol.org/content/168/3/1362.long
12. Morrison B, et al. Chemokine-mediated recruitment of NK cells is a critical host defense mechanism in invasive aspergillosis. J Clin Invest. doi: 10.1172/JCI200318125. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC296992/.
13. Kamai Y, et al. Interactions of Aspergillus fumigatus with vascular endothelial cells. Med Mycol. doi: 10.1080/13693780600897989. http://mmy.oxfordjournals.org/content/44/Supplement_1/S115.full.pdf+html.
14. Kamai Y, et al. Polarized Response of Endothelial Cells to Invasion by Aspergillus fumigatus. Cell Microbiol. doi: 10.1111/j.1462-5822.2008.01247.x. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3393649/.
15. Latge JP. Aspergillus fumigatus and Aspergillosis. Clin Microbial Rev. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC88920/.
16. Walsh T, et al. Treatment of Aspergillosis: Clinical Practice Guidelines of the Infectious Diseases Society of America. Clin Infect Dis. doi: 10.1086/525258. http://cid.oxfordjournals.org/content/46/3/327.1.full#sec-1.
17. Howard S, et al. Frequency and Evoluton of Azole Resistance in Aspergillus fumigatus Associated with Treatment Failure. Emerg Infect Dis. doi: 10.3201/eid1507.090043. http://wwwnc.cdc.gov/eid/article/15/7/09-0043_article.
18. Rijnders B, et al. Aerosolized Liposomal Amphotericin B for the Prevention of Invasive Pulmonary Aspergillosis during Prolonged Neutropenia: A Randomized, Placebo-Controlled Trial. Clin Infect Dis. doi: 10.1086/586739. http://cid.oxfordjournals.org/content/46/9/1401.full.pdf+html.
Created by William Mangin, student of Tyrrell Conway at the University of Oklahoma.
