Clostridium botulinum, associated neurotoxins, and botulism
Clostridium botulinum, Neurotoxins, and Botulism
By Tyler Smith
Introduction to Clostridium botulinum
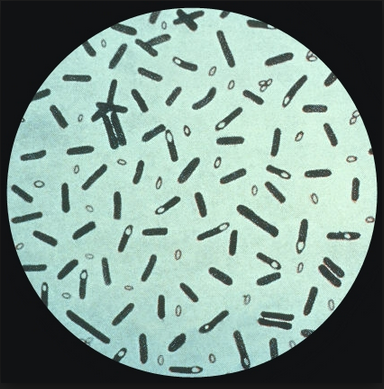
Clostridium botulinum is a Gram-positive staining, anaerobic bacterium. Clostridium botulinum is also rod-shaped, endospore-forming, and responsible for producing the neurotoxin that causes botulism. Clostridium botulinum is mostly found in marine-sediments and soils all over the world, as evidenced by cases of botulism that have been reported in Europe, North America, and Australia (Sugiyama 1980). It can also infiltrate and contaminate any plant or vegetable that is grown in such contaminated soils, which can be a mode through which people are infected with the neurotoxin. Furthermore, when introduced through a variety of ways, it can colonize the gastro-intestinal tracts of mammals, birds, and fish. Thus, Clostridium botulinum, as well as the disease it causes, are widespread and of great interest to scientists all over the world.
Clostridium botulinum causes the disease botulism, which was given the name after an outbreak of the disease in the 1700’s where all of the people who were infected had eaten from the same large sausage. In fact, the Latin word for “sausage” is “botulus”. Thus, when Emile van Ermengem published a description of the bacterium that causes the disease botulism, he called it Bacillus botulinus. However, since bacilli are predominantly aerobic microbes, and Clostridium botulinum is anaerobic, the bacterium was renamed to reflect its current place in nomenclature: Clostridium botulinum (Caya et al. 2004).
Clostridium botulinum can be isolated in pure culture on TSC (tryptose sulfite cycloserine) growth media in very little (>2%) oxygen. As an obligate anaerobe, Clostridium botulinum can actually survive small amounts of oxygen because it is equipped with an antioxidant defense enzyme, superoxide dismutase, which essentially protects the cells from damage due to oxygen exposure. As an endospore-forming organism, Clostridium botulinum is somewhat unique. Whereas most endospore-forming microbes form spores to preserve cells during long periods of unfavorable environments, Clostridium botulinum is only capable of forming spores in anaerobic environments in which it thrives. More interestingly, Clostridium botulinum can only produce the neurotoxin responsible for causing botulism during sporulation, which can only occur in favorable environments.
When somebody is infected with the botulism neurotoxin, the progression to death is very unpleasant. However, the neurotoxin is not contagious, and therefore cannot be transferred from one person through another through the air or closed skin. Ironically, the neurotoxin has also been used therapeutically in modern medicine for conditions characterized by muscle incontinence. This is because of the paralytic effect that the neurotoxin has, and, in controlled situations, it can be used therapeutically (Caya 2004). On the other hand, there is the threat that neurotoxins produced by Clostridium botulinum could be used as a method of bioterrorism. All of these topics are discussed below.
Neurotoxin Production and Pathology
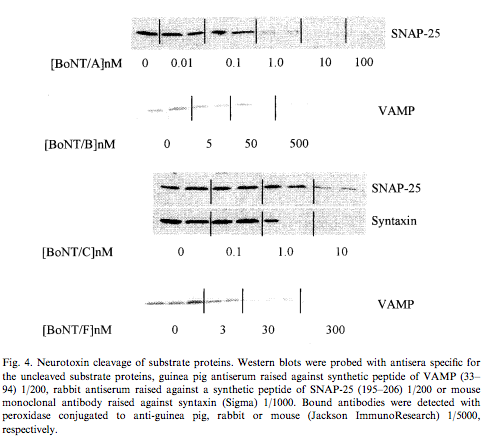
The neurotoxins produced by Clostridium botulinum are characterized as belonging to a group of proteins linked by disulphide chain bridges. Each protein consists of a lighter and heavier chains (50 kDa; 100 kDA) responsible for lysing membrane proteins and binding and delivering the toxins to the cytosol of the host neurons through specific membrane proteins, respectively (Oguma et al. 1995; Montecucco et al. 1996). There are three general modes through which a person could be infected with Clostridium botulinum, the neurotoxin it produces, and the resulting disease, botulism. Those three methods are food poisoning, wound botulism, and infant botulism (Sugiyama 1980). Infant botulism is just another form of food poisoning, since infants usually contract the disease through food they eat. However, while infants can contract the disease from any food that has been infected with Clostridium botulinum, the only food in which infants have eaten from and has been isolated with cultures of Clostridium botulinum is honey. In fact, some scientists have warned that the risk of developing botulism in infants outweighs any possible reward of feeding them honey until they are at least 12 months old. Wound botulism is a different form of botulism, however, where the botulism is contracted through an open wound. In wound botulism, the gastro-intestinal symptoms seen in food poisoning and infant botulism are not exhibited since the toxins are absorbed through the bloodstream. When the toxin is absorbed into the neuronal cytosol, the neurotoxins begin to lyse membrane proteins that are responsible for targeting synaptic vesicles to uptake material into the plasma membrane. There are several different neurotoxins produced by Clostridium botulinum, labeled A, B, C1, C2, D, E, F, and G. Each one has a different cleavage site on the substrates they attack, all work differently within the cells, and have different, unique toxicity levels. When the proteins are cleaved and lysed on the membranes, the result is that acetylcholine cannot be released. Acetylcholine is a neurotransmitter in many organisms that is responsible for activating skeletal muscles. Thus, when acetylcholine is not released, the results are often deadly (Montecucco 1996). The botulism neurotoxin also inhibits the release of neuropeptides, which neurons essentially use for communication. These molecules are used in a wide range of activities within an organism, and their inhibition can be very costly.
Symptoms
Botulism is characterized by many symptoms. Early symptoms include nausea, gastric distress, diarrhea, and constipation. More symptoms include weakening and drooping of the eyelids, vision troubles, loss of facial muscle movements, loss of the ability to swallow, and the loss of the ability to talk. Further spread of the toxin throughout the body can lead to decreases in the neuromuscular ability to move extremities as well as difficulty with respiration. Most deaths associated with botulism are the result of respiratory failure caused by the neurotoxins spreading throughout the body. These symptoms spread so fast that forensic pathologists have previously classified deaths resulting from Clostridium botulinum producing the deadly neurotoxin in the gut of infants, thereby killing the infants, as sudden infant death syndrome (SIDS) (Arnon et al. 1978). Other symptoms throughout the course of this disease include constipation, lightheadedness, dry mouth and throat, vomiting, and loss of voluntary muscle control. While the prognosis has improved drastically over the past several decades, people who are inflicted with cases of botulism poisoning sometimes experience respiratory depression symptoms for up to years after their original episode. These people must often seek long-term treatment and respiratory rehabilitation for such symptoms, which can also lead to mental and financial burden. The following scientifically examined cases adequately outline these symptoms.
Specific Cases
Before ethical standards existed as they do today, researchers studied the effects of Botulism on rhesus monkeys and squirrel monkeys. In all, 101 monkeys were affected with the neurotoxins intravenously to study how closely the affected monkeys reflected the symptoms of humans that had been intestinally affected with Botulism. The progression of this disease in adults is particularly grotesque and painful, and is characterized by early symptoms such as headache, nausea, diarrhea, and constipation. Late symptoms include pharyngeal paralysis that restricts swallowing, inability to talk, choking, strangulation, and ultimately death. Since the monkeys were injected with the toxins intravenously, they did not exhibit the gastro-intestinal symptoms that humans exhibit after being infected through the intestine. However, the rest of the disease exhibited the exact same course of symptoms in the monkeys as it does in humans. The observers noted that, during the early stages of the disease, the monkeys would frequently bump into large objects on the laboratory floor. From there, symptoms progressed to muscular weakness, inability to swallow, vomiting, respiratory failure, and ultimately death. The authors also noted that, in their study, the monkeys were most susceptible to the Type A botulinum neurotoxin. Furthermore, the lethal dose at which 50% of the rhesus monkeys died was 40 MU/kg (Herrero et al. 1967).
Another study proposed that neurotoxin production by Clostridium botulinum might be one cause of sudden infant death syndrome. They examined 280 dead infants for the presence of the neurotoxin and Clostridium botulinum. They outlined four particular cases that they say were typical of all of the case-reports in which the neurotoxin was found in the dead infants body. One case describes an infant that appeared perfectly healthy when placed in bed. However, the baby was found dead 8 hours later in the same position that the mother left it. Microscopy later showed that the baby had suffered congestion in its lungs, brain, kidneys, and liver. The other three were very similar, and consisted of a parent putting the infant to bed, and returning to see that the infant had died in a similar position. Each death occurred seemingly quick, over a period of hours or days, hence the name “sudden infant death syndrome”. This syndrome has also been called “crib death” because of the sheer number of infants that die overnight while in their cribs (Arnon 1978).
Cases of botulism have also been observed in elderly patients. In the early 1970’s there was an outbreak of botulism in Birmingham, Alabama that was traced back to Clostridium botulinum samples found in a suspicious leftover can of salmon. This case was similar to many other cases and was characterized by a loss of facial muscle use, loss of eye movement, and respiratory failure. The patients also experienced hypotension, dysphonia, dysphagia, and ptosis. They were all administered antitoxin therapy, yet respiratory muscle use was never fully restored (Ball et al. 1979).
The first ever cases of infant botulism cause by the neurotoxin serotype E produced by Clostridium botulinum were reported in two 16-week-old infant girls in Italy. In the case of the first girl, the doctors originally misdiagnosed the disease as being an intestinal blockage that required surgery. After surgery, her conditioned worsened, she began to display some of the stronger symptoms typical of infant botulism, and the diagnosis was made. The second case was presented at the same hospital, and because of her conditions and having dealt with the first case just 7 months earlier, the doctors immediately suspected that it was infant botulism. Their suspicions were confirmed for both cases by fecal cultures. However, the organism that the scientists isolated was Clostridium butyricum, which closely resembles Clostridium botulinum, and produces a type E serotype neurotoxin that is indistinguishable from the one that Clostridium botulinum produces (Aureli et al. 1986). In 2000, scientists analyzed and characterized the binding sites of the Clostridium botulinum neurotoxin serotype B. They felt as though the insight that they were able to provide about the catalytic and binding sites of the neurotoxin type B would allow for someday manufacturing specific inhibitors that would block the reception of the neurotoxins by the binding sites (Swaminathan & Eswaramoorthy 2000). This was huge progress at the time, since just 20 years earlier the first two cases of type E infant botulism had surfaced in Italy. With this type of information, hopefully scientists will be able to create specific inhibitors to the binding sites of all of the different neurotoxin serotypes that are produced by Clostridium botulinum.
Treatments
Stomach pumping is common practice if the disease is food-related, otherwise antitoxin serums can be administered to the patient. In infants, the prognosis is not good, though human-derived antitoxins are currently being tested (World Health Organization, 2000). The prognosis is often not good because of the reasons outlined in the aforementioned cases of sudden infant death syndrome, where infants appear to be completely healthy just hours before they succumb to botulism. For this reason, it is sometimes very difficult to diagnose an infant with botulism, as many of the symptoms go overlooked, and are sometimes just written off to be symptomatic of the common cold. One case actually documented that doctors actually thought that the baby only had a common cold. Symptoms even looked like they were improving. However, as in many of the other cases, the baby was put to bed and the parents later found the infant dead in the same position as they had left it.
In 1985, despite measures taken to eliminate botulism as a cause of sudden infant death syndrome, the botulinum toxin was still found in 15% of 70 sudden and unexpected infant deaths (Sonnabend et al. 1985). Since then, the instances of botulism in infants and adults alike have become increasingly rare, less frequent, and more treatable. Regardless, scientists still allocate time to this subject because of the nature of the disease.
Vaccination has previously been used to confer resistance to humans to the poisoning of the neurotoxin produced by Clostridium botulinum. However, to date, those vaccinations have been difficult to produce because they are very expensive to produce and also relatively unsafe. Efforts have been made by researchers to construct a synthetic gene fragment of botulinum neurotoxins to confer protection against the botulinum toxin in humans by using nontoxic fragments of the original neurotoxin. This would alleviate both the cost-related and safety related issues of the production of the vaccine using the toxic form of the neurotoxin (Clayton et al. 1995).
More recently, scientists have developed a good candidate for a vaccine to protect against botulism from the neurotoxin serotype A. These researchers showed that their vaccine protected against botulism challenges in mice, yet are unproven in humans (Yu et al. 2009). More work is necessary to create a viable option for a vaccine in this area. Furthermore, their vaccine only addresses one serotype (A) of the Clostridium botulinum neurotoxin, which leaves several other serotypes to be studied. In fact, previous work has shown differential effects of different neurotoxin serotypes in cultures of embryonic rat dorsal root ganglia neurons (Welch et al. 1999). In fact, in embryonic rat dorsal root ganglia neurons, the most potent serotype (A) was 1000-fold more toxic to the cells than the least potent serotype (B) (Figures 3 & 4). Overall, more work is needed in the area of vaccination if botulism is to truly be combatted preventatively on a large scale.
Positive Uses of the Neurotoxin
Interestingly, the botulism neurotoxin, one of the most deadly poisons known to man, has been isolated from Clostridium botulinum and used for therapeutic purposes. When used in a controlled setting, the neurotoxin can be used in a variety of situations to treat conditions characterized by muscle spasms or a lack or muscular control. Some conditions that the neurotoxin can be used to treat include glabellar lines, limb spasticity, tremors, and many other conditions that might be associated with underlying neurological conditions. However, a relatively new form of botulism, known as inadvertent botulism, is characterized by cases of botulism that arises from the chronic use of the toxin in therapeutic situations, or accidental exposure in a laboratory setting (Caya 2004).
Biological Warfare Ramifications
Cases of botulism have become extremely rare in the United States, meaning very few doctors in the U.S. have actually seen a case firsthand. In light of the September 11th terrorist attacks in 2001, some scientists have suggested that the study of Clostridium botulinum, the neurotoxin it produces, and botulism are all of national interest, and pose a significant threat when considered for possible use through bioterrorism. When anthrax was used in bioterrorism, the inhalation delivery method was used, which is the same method that scientists believe would be used, should somebody want to introduce the toxin to a community. While this scenario is unlikely, it is certainly possible. The threat has certainly died down somewhat since we are now 13 years removed from the last foreign terrorist attack on American soil. However, last year’s Boston bombings illustrate that terrorism is still very much a threat to the lives of individuals everywhere. Therefore, it is very much still in the interest of the general public that doctors remain vigilant to these types of attacks. Scientists point to the front-line clinicians as being the main group through which an emergency like this would be recognized and neutralized swiftly and efficiently (Caya 2004).
References
Sugiyama H. 1980. Clostridium botulinum neurotoxin. Microbiological Reviews 44(3): 419 – 448