Ebola virus
Introduction
Ebola virus is a member of the Filoviridae viral family of RNA viruses, which are characterized by the long, thin filaments seen in micrograph images. It is named after the Ebola River where the virus was first discovered.
The virus causes Ebola hemorrhagic fever, which is a serious and usually fatal disease for those who contract it. It damages the endothelial cells that make up the lining of the blood vessels and creates difficulty in coagulation of the infected individual’s blood. As the vessel walls become more damaged, and the platelets cannot coagulate, the individual undergoes hypovolemic shock, or a dramatic decrease in blood pressure. Depending on the type of virus, Ebola can have up to a 90 percent mortality rate for those infected. For more details on the infection mechanism, see Infection Mechanism of Genus Ebolavirus.
Until the 2014 outbreak, Ebola hemorrhagic fever was reported in humans only in Africa. Figure 1 shows a man who has fallen ill with Ebola in the Democratic Republic of the Congo, formerly known as Zaire. He most likely died shortly after this photograph was taken due to a great loss of blood. The other person in the photo is dressed in protective clothing so as not to contract the virus from the patient.
There are several different types of Ebola virus that effect humans. Currently they are Zaire, Sudan, and Ivory Coast Ebola virus, named for the respective regions in Africa in which the strain was found. Reston Ebola virus is a type of Ebola that only infects non-human primates. It was first discovered in an outbreak in Reston, Virginia. Outbreaks of Ebola are sometimes caused by new strains of the virus; so more types can and are being discovered. For example, in 2007 there was an outbreak of Ebola hemorrhagic fever in the Bundibugyo District of Uganda where a new strain of the virus, as classified according to the Center for Disease Control, was found to be the cause.
Ebola virus is a large concern of public and global health because it has such a high mortality rate that it is a very dangerous virus and a potential bioterrorism agent.
History
Ebola virus was first discovered in 1976 when an outbreak of Ebola hemorrhagic fever occurred in Zaire and another later that year in Sudan. Each outbreak had about 300 victims, but did not spread much larger than that because of the remoteness of the areas in which they occurred.
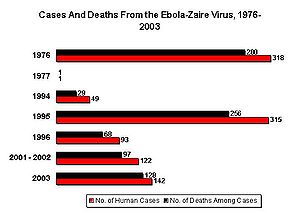
The Zaire Ebola virus has one of the highest fatality rates of any pathogenic virus affecting humans. In the 1976 outbreak, it killed 88 percent of patients, 81 percent in 1995, 73 percent in 1996, 80 percent in 2001-2002, and 90 percent in 2003, although none of these outbreaks were as large as the original. Figure 2 shows the number of cases in each outbreak from 1976 through 2003 along side of the number of deaths in each outbreak. This chart highlights the high fatality rate of Zaire Ebola virus.
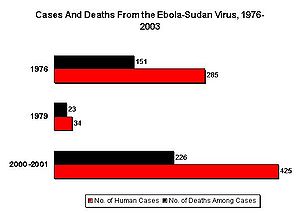
Sudan Ebola virus has a lower, yet still very dangerous, fatality rate of 53 percent in 1976, 65 percent in 1979, 53 percent in the over 400 patients infected in 2000, and 41 percent in 2004. Figure 3 charts the number of individuals infected in three outbreaks of Sudan Ebola virus between 1976 and 2003 as well as the number of these victims that died because of Ebola hemorrhagic fever. It is clear the Sudan Ebola virus, although not as fatal as the Zaire strain, is still very lethal.
Ivory Coast Ebola virus was first discovered in 1994 when a scientist conducting autopsies on chimpanzees contracted Ebola hemorrhagic fever. This strain found was different than the Zaire or Sudan strains. However, this has been the only case of Ivory Coast Ebola known to have occurred in humans.
Most Ebola virus outbreaks have originated in Africa and have traveled only to other countries through shipment of non-human primates or through accidental contamination in testing facilities. Crab-eating macque that were imported from the Philippines to Reston, Virginia in 1989 were found to have a virus similar to Ebola. Over 150 animal handlers were all tested for Ebola and only 6 were found to have developed antibodies to it, none of which actually developed Ebola hemorrhagic fever. The Center for Disease Control concluded that this strain had a low infection rate for humans and it was later classified as its own strain named Reston Ebola virus.
For a complete list of Ebola cases throughout history see: Known Cases and Outbreaks of Ebola Hemorrhagic Fever, in Chronological Order compiled by the CDC.
Transmission
Ebola is transmitted through bodily fluids and/or direct contact with infected individuals. It is believed to spread to human populations through contact with infected primates, as opposed to directly from natural reservoirs. The suspected natural sources of the virus are certain species of fruit bats. They have been found to carry the virus, but they themselves are asymptomatic, making them good candidates for natural reservoirs.
Outbreaks of Ebola virus are often traced to an individual that has handled a gorilla or chimpanzee carcass. It is common for the virus to then spread to family members or hospital workers because of their close proximity to the victim. The virus spreads to people that come into contact with these patients’ blood or contaminated medical equipment. Because Ebola kills its victims so quickly and the outbreaks usually occur in isolated areas, the disease does not typically spread very far. Also, Ebola has an incubation period of up to 21 days, but is normally closer to 10 days, so infected persons do not have time to carry the disease very far. It is highly unlikely that Ebola could turn into a large epidemic.
Oftentimes Ebola outbreaks are mistakenly classified initially as outbreaks of malaria, dysentery, influenza, typhoid fever or other bacterial infections because the early symptoms are similar and these infections are common in the same areas of Africa. This misinterpretation of symptoms can lead to the spread of Ebola within medical centers because necessary precautions are not taken.
Transmission of Ebola virus among non-human animals is a little different. It is proposed that fruit bats drop partially eaten fruits that carry viruses in the bat saliva. Gorillas or other monkeys then eat the fruit, and therefore the virus as well. Gorilla carcasses have been found to contain multiple strains of Ebola virus. Decomposing bodies only remain infectious for three to four days after death, and gorillas do not typically interact among different groups, which means the victims were probably infected by several animal host reservoirs.
Symptoms
Ebola virus begins to effect infected individuals with flu-like symptoms. There is a quickly oncoming fever, achy muscles, and headache, which are soon followed by bloody vomit and diarrhea. Some days later, victims can begin to bleed through the eyes, nose, or mouth. A hemorrhagic rash can develop on the entire body, which also bleeds. Muscle pain and swelling of the pharynx also occur in most victims.
Patients are diagnosed by testing of urine or saliva with an ELISA test, however the results are not always accurate.
Due to the extensive amount of bleeding, most patients will die of hypovolemic shock and/or systematic organ failure within 2 to 21 days of contracting Ebola virus. However, some patients do defervesce after about 14 days and are able to survive the virus.
Prevention and Treatment
There is currently no treatment for Ebola hemorrhagic fever. Infected individuals are treated for the symptoms they have, but the body must fight off the virus on its own. To help patients deal with symptoms better, supportive care is usually given. This includes:
• Administering intravenous fluids in order to keep normal levels of electrolytes.
• Using breathing devices to maintain oxygen levels and drugs to control fever.
• Maintaining blood pressure and trying to aid in blood clotting through medications.
• Preventing infections from bacteria through use of antibiotics.
• Relieving pain and keeping as clean of an environment as possible through good nursing care
A vaccine for Ebola virus is currently being extensively researched. Ebola is on the United States’ list of possible bioterror agents. Due to the high risk, the US government is putting funds into vaccine research.
There is a vaccine that has been proven effective in non-human primates to prevent the contraction of Ebola virus, however there are no vaccines approved for humans yet. A prototype vaccine was administered in March of 2009 to a researcher who was accidentally pricked with a syringe containing Ebola virus particles. The vaccine was given to her as an emergency treatment. There seemed to be no harmful side effects of the injection and she did not develop Ebola hemorrhagic fever. However, it is uncertain if she was actually ever infected with the virus so researchers cannot be sure if the virus was effective or not. Subsequent research is being conducted and will hopefully lead to an Ebola vaccine in the near future.
Current Research
The National Institute of Allergies and Infectious Diseases collects records of all new and emerging research on Ebola virus.
In 2005, a study was performed in collaboration with the United States Army Medical Research Institute for Infectious Diseases to test the efficiency and effects of a new, longer-lasting immunization for non-human primates against Ebola virus that required only the boost dose in lieu of the previous vaccination followed by the boost. The results showed that the boost was just as effective on its own.
Due to these results, a fast-acting, single dose vaccination was developed and tested in humans. The purpose of such a vaccine is to allow health workers the ability to contain Ebola virus outbreaks through ring vaccinations. In a ring vaccination, vaccines are given to all people not yet infected in the region of Ebola cases. A fast acting vaccine is the best for this strategy and protects the entire community from a devastating outbreak. This study was completed in 2008 and is still being followed to see if the immunity is long lasting.
Before this single dose vaccine was created, there was another vaccine developed for humans that was tested in 2005. This vaccine entailed three doses of vaccine but proved to be safe, without serious side effects and appeared to create good immune responses in trial participants. However, with the discovery of the new, fast-acting vaccine this three-dose vaccine may no longer be relevant.
In 2009, a study is currently underway that includes collaborations from the United States Military as well as international groups that tests new DNA vaccines for Ebola and Marburg viruses. This new type of vaccine is still being experimented with and the results are unknown.
A major concern in formulating an Ebola vaccine is that in the regions where the virus is most commonly observed, many of the patients are immunocompromised due to HIV. A vaccine could therefore be more harmful than helpful in preventing Ebola hemorrhagic fever because it could actually cause the disease. A study done in 2008 on rhesus macaque monkeys who were infected with simian immunodeficiency virus (SIV) showed that the monkeys did not contract Ebola from the vaccine. The vaccine is therefore thought to be safe for immunocompromsied human patients.
A study was published in the Journal of Infectious Diseases in 2004 that brought to light interesting new information on the natural reservoirs of Ebola virus. It was recorded that approximately 13 percent of wild-born chimpanzees had Ebola antibodies in their blood. This finding showed researchers that Ebola virus is and was in circulation in the forests of countries where no human cases have been reported or before it infected humans. It also showed that chimps can be in contact with Ebola and survive, telling also that they have probably been exposed multiple times. An aspect of this research that is very relevant to global health is the possibly that is now known that Ebola can exist in places where it has not been before and could cause human outbreaks in unexpected countries.
Relation to Global Health Today
Ebola is such a great concern of global health today because of its high fatality rate. Outbreaks up to this point have been relatively small, although they have been very deadly. Recently, it has been discovered that there is evidence of Reston Ebola virus in swine populations in the Philippines. This could mean that the virus had been around since before 1989, when it was first detected in monkeys. If the disease has the ability to mutate and infect other animals it needs to be closely monitored so that it does not surprisingly surface in other animals.
The main goals currently being addressed with Ebola virus are finding ways of treatment for Ebola hemorrhagic fever and finding safe and effective vaccines for the virus that can be applied to humans. If an approved vaccine could be developed for Ebola virus, it would save many people from the painful effects of Ebola hemorrhagic fever.
Although it is not a problem right now for most populations outside of Africa, Ebola virus has the potential to be dangerous from the point of view of global health in the future. With more research and a greater understanding of the virus, Ebola will hopefully become a less pressing matter in global health.
This page was created by Andie Asimes.
References
Roger W. Barrette, Samia A. Metwally, Jessica M. Rowland, Lizhe Xu, Sherif R. Zaki, Stuart T. Nichol, Pierre E. Rollin, Jonathan S. Towner, Wun-Ju Shieh, Brigid Batten, Tara K. Sealy, Consuelo Carrillo, Karen E. Moran, Alexa J. Bracht, Gregory A. Mayr, Magdalena Sirios-Cruz, Davinio P. Catbagan, Elizabeth A. Lautner, Thomas G. Ksiazek, William R. White, Michael T. McIntosh "Discovery of Swine as a Host for the Reston ebolavirus. Science. 2009. Volume 325. p. 204-206.
Thomas W. Geisbert, Kathleen M. Daddario-DiCaprio, Mark G. Lewis, Joan B. Geisbert, Allen Grolla, Anders Leung, Jason Paragas, Lennox Matthias, Mark A. Smith, Steven M. Jones, Lisa E. Hensley, Heinz Feldmann, Peter B. Jahrling "Vesicular Stomatitis Virus-Based Ebola Vaccine Is Well-Tolerated and Protects Immunocompromised Nonhuman Primates". 28 November 2008. PLoS Pathogens.
E. M. Leroy, P. Telfer, B. Kumulungui, P. Yaba, P. Rouquet, P. Roques, J.-P. Gonzalez, T. G. Ksiazek, P. E. Rollin, and E. Nerrienet. "A Serological Survey of Ebola Virus Infection in Central African Nonhuman Primates". 1 December 2004. Journal of Infectious Diseases.
"Ebola and Marbug Vaccine" Crucell Biopharmaceuticals
"Ebola/Marbug Vaccine Development" National Institute of Allergies and Infectious Diseases
Associated Press "Experimental Ebola Vaccine Used on Human" 27 March 2009.
"Ebola" Wikipedia
"List of Ebola Outbreaks" Wikipedia
Edited by student of Joan Slonczewski for BIOL 191 Microbiology, 2009, Kenyon College.