Herpesviridae and Their Role in Uveitis
Introduction
Herpesviridae, which is most commonly known as herpes, is a family in the order Herpesvirales, that is made up of DNA viruses known for causing diseases in humans and other animals. There are many viruses in this family, more than 130 [1], and there are 3 subfamilies: Alphaherpesvirinae, Betaherpesvirinae, and Gammaherpesvirinae. Out of all Herpesviridae, only eight use humans as their primary host [2]. In the Alphaherpesvirinae group, the viruses are the herpes simplex virus 1, herpes simplex virus 2, and varicella-zoster virus. In the Betaherpesvirinae group, the viruses are the cytomegalovirus, Human herpesvirus-6, and Human herpesvirus-7. In the Gammaherpesvirinae group, the viruses are the Epstein-Barr virus and Kaposi’s sarcoma herpes (or Human herpesvirus-8). The Alphaherpesvirinae virus, the most common Herpesviridae subfamily, have a short replication cycle, that takes about 18 hours. They have a wide range of hosts, and destroy cells efficiently. The Betaherpesvirinae virus replication cycle is long, and has a relatively small number of host cells that it can infect. When they infect cells it results in the cells becoming enlarged (called cytomegalo). The Gammaherpesvirinae virus also has a very narrow host range, and they are specific for only T or B lymphocytes [3, 8].
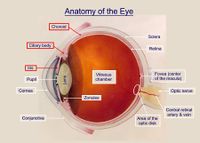
One consequence of becoming infected with a Herpesviridae virus is the possibility of uveitis. This disease causes a form of inflammation in the eye. Specifically, it is the inflammation of the uvea, which is a pigmented layer in the eye that is composed of the iris, ciliary body, and choroid. Uveitis can be in either one eye or both eyes, and it can also involve other parts of the eye such as the cornea, sclera, retina, vitreous body, and/or the optic nerve. It is considered an ophthalmic emergency and it needs to be examined by an optometrist or ophthalmologist, followed by treatment in order to control the inflammation. If left untreated, it will often lead to blindness [5]. Uveitis can be described more specifically based on where in the eye it occurs. There is anterior uveitis (the inflammation of iris, or of both the iris and ciliary body), intermediate uveitis (inflammation of the cilliary), posterior uveitis (inflammation of the choroid), and panuveitis uveitis (inflammation in all areas of the uvea).
Of the eight herpesviridae capable of infecting humans, five of them are incredibly common. Herpes simplex virus 1 and herpes simplex virus 2 are the cause of genital and orolabial herpes, cytomegalovirus causes mononucleosis and pneumonias, Epstein-Barr virus causes mononucleosis, and the varicella-zoster virus is responsible for both shingles and chicken pox. Of these common viruses, herpes simplex virus, varicella-zoster virus, and cytomegalovirus are each capable of causing acute, recurrent, and chronic uveitis [4]. All herpesviridae viruses can be latent or lytic. Many people who are infected are unaware because they don’t exhibit any symptoms.
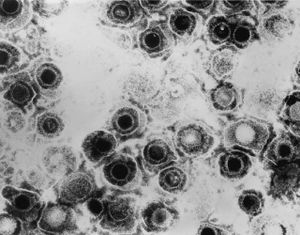
Herpesviridae Structure
All Herpesviridae virions have the same unique structure made up of four elements or layers, which is how viruses come to be classified as such [3]. These elements are the core, capsid, tegument, and envelope. The structure of the virus is responsible for keeping the its genome safe, as well as enabling the virus to infect the correct target cell. Within the core, there is a molecule of double-stranded DNA. Virus DNA in the Herpesviridae family generally have about 120 to 250 kb pairs. The virus core is inside of an icosahedral capsid, which usually has a diameter of about 100 nm that is made up of 162 capsomeres. Herpes simplex virus capsids are made up of five conserved proteins. These proteins are pUL19, that is responsible for forming all of the capsids, pUL18 and pUL38, that form triplexes so that adjacent capsomeres can be interacted with and stabilized, pUL35, that is responsible for covering hexons, and pUL6, that is responsible for forming a portal [7]. Depending on the type of Herpesviridae virion, there may be other cellular proteins there such as actin, tubulin, heat shock proteins, or annexin [7]. The tegument, which coats this capsid, is a layer of proteins that has viral mRNAs along with viral proteins in it. Surrounding the tegument is a lipid bilayer envelope that contains glycoproteins, lipids, and polyamines in it [3, 7].
More Uveitis and Herpesviridae Information
There are some false preconceptions about the herpes simplex virus. While it is commonly assumed that main way someone receives the virus is as a sexually transmitted disease, this is only true in a small percentage of ocular cases. A patient’s history often plays the largest role in their chances of infection. Also, Herpesviridae are known for their ability to stay latent for many years in the ganglia. In fact, more than 90% of people have the latent virus in their body, but exhibit no symptoms [15]. Most people that carry the latent virus don’t even know that they have it. However, when the body’s immune system is compromised, that is when the virus may become active. A person’s genetic makeup along with the strength of the virus also affect the virus’s latency.
Each year, there are more than 500,000 cases of active herpes simplex ocular infection in just the United States. Additionally, in developed countries, ocular herpes simplex virus is one of the biggest reasons for blindness [12]. Based on where the ocular infection takes place in the eye, the disorders that herpes simplex virus causes will vary. They include: conjunctivitis, blepharitis, episcleritis, scleritis, keratitis, anterior uveitis, retinitis, and vitritis. While herpes simplex virus is not the only cause of uveitis, it is a very common infectious cause of it, and it is responsible for about 9% of anterior uveitis infections. Herpes simplex virus can cause an inflammatory reaction that can be acute, chronic or recurrent. When it is acute herpes simplex virus uveitis is often linked to corneal involvement that causes keratitis. Although uveitis caused by herpes simplex virus can occur both with or without corneal inflammation [12].
In the past, Herpesviridae viruses in uveitis have often been misdiagnosed. In subjects infected by herpes simplex virus uveitis, correct diagnosis was established at its onset in merely 4% to 9% of cases. After a long period of follow ups, that percentage raises to 44% [12]. The average length of time in between the beginning of ocular disease and its correct diagnosis was 3.4 years [12]. Furthermore, in one study, herpes simplex virus uveitis had a missed or ignored diagnostic rate of 70% [12].
By knowing what clinical symptoms to look for, optometrists should be able to spot Herpesviridae viruses in uvieits more often with a higher success rate. For instance, herpes simplex virus infection in the uveal tract usually looks like anterior uveitis or iridocyclitis. Although posterior uveitis, panuveitis, or retinitis can also occur sometimes [12]. There are many symptoms to look out for. For example, some other Herpesviridae uveitis symptoms include lowered corneal sensation, iris transillumination defects, posterior iris synechiae, unexplained corneal scarring, anterior and/or vitreous cells, granulomatous or non-granulomatous KPs, focal or diffuse patchy iris atrophy, and elevated intraocular pressure. Inflammation in the posterior can cause retinal vasculitis, cystoid macular edema, papillitis, spontaneous hyphema, and acute retinal necrosis. Also, herpes simplex virus uveitis in most cases is unilateral recurrent inflammation. A study found that about 85% of those infected with herpes simplex virus uveitis have unilateral involvement of ocular inflammation, and about 8% of infected have bilateral uveitis. Furthermore, herpes simplex virus uveitis can be linked with corneal involvement and with herpes simplex virus keratitis [12].
Etiology
Herpes simplex virus I and herpes simplex virus II each have different virus specific antigens. While they can both result in an infection in multiple areas on the body, herpes simplex virus I tends to occur in the middle of the pharynx, and herpes simplex virus II tends to occur in the genital region. When it comes to herpes in the eye, the cause is usually due to herpes simplex virus I. In most cases, the virus gets to the cornea of the eye through direct contact, or through the trigeminal nerve after the person has already been infected orally [16]. However, when first infected, in most cases, the person will show no symptoms of it. It is most likely to be reactivated when the infected person’s immune system is weakened. This reactivation can occur on any branch of the trigeminal nerve [16]. The only sure-fire way to prevent infection is to completely avoid any direct contact with it.
Diagnosis & Treatment
Uveitis has the potential to cause severe eyesight loss or blindness. In the United States, it is the cause of 10 to 20% of blindness [14]. Therefore, it is very important that it gets diagnosed correctly, including the cause behind the uveitis. If something is diagnosed incorrectly, the treatments will be wrong, which can possibly lead to other potential problems. Diagnosis can sometimes be a problem, especially with inexperienced ophthalmologists, because some of the disease’s signs can be very hard to identify. Even if the disease is seen to be as a result of a herpesviridae virus, it is vital to know which specific virus it was. Therefore, it must be determined if it was a herpes simplex virus, a varicella-zoster virus, or a cytomegalovirus virus.
Uveitis associated with herpes simplex virus is most common in people younger than 60 years old, however, it is possible to at any age. In most cases, this occurs one eye only, although it is possible in both eyes. Also, this condition is usually linked to acute ocular hypertension, or raised intraocular pressure in the eye, but not always. Sometimes, there will be iris atrophy, which is an out of place pupil, that will strongly suggest the cause of the uveitis to be herpes simplex virus. Also, a history of herpes simplex virus on the subject’s lips or genitals will help point to an answer, but that is not absolutely necessary. Some other symptoms to look for in a subject include large and central keratic precipitates (this is an inflammatory cellular deposit that would not be a worry if they were more evenly distributed on the corneal endothelium), dilated pupils, and a defect in iris transillumination [4]. Individually, none of the symptoms will result in a conclusion of herpes simplex virus, but when put together, a result can be found. Effective treatments for uveitis associated with herpes simplex virus have been found. It is recommended to take systemic antivirals as the primary treatment, as they will help to protect the cornea in the eye along with treating the uveitis. It has also been observed that if a topical antiviral is used for an extended period of time, the infected person is at risk for the development of keratopathy, which is a corneal disease that is caused by calcium appearing on the central cornea, which can lead to calcification. In addition, using topical corticosteroids also has a potential to cause some problems, mainly because of they are extremely hard for those infected with herpes to stop taking, resulting in a long and slow process in order to taper off of them [4].
Uveitis associated with varicella-zoster virus is most common in people older than 60 years old, but it possible at any age. One identifying characteristic of this virus causing uveitis is what looks like a little bit of string in the cornea of the infected person. This is caused by a special form of pseudodendrite that has cells amassed together in the center with no ulcerations. Varicella-zoster viruses in uveitis are also linked to greatly lessened corneal feelings, which essentially the reason for the blink reflex. Additionally, the symptoms seen in herpes simplex virus associated with uveitis can also be seen in varicella-zoster virus associated uveitis. However, the two can be easily differentiated because those infected with the varicella-zoster virus almost always has a history of dermatitis/shingles, or inflammation of the skin, caused by the virus, and it always occurs on the same side of the body. Treatment for this virus is similar to the herpes simplex virus treatment, so systemic antivirals are taken, except that the dose is doubled. To prevent the varicella-zoster virus, physicians use Varivax for chickenpox and Zostavax for shingles [4].

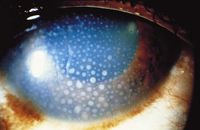
Uveitis has just relatively recently started to be associated with the cytomegalovirus virus. This virus causes uveitis much less frequently than the herpes simplex virus or the varicella-zoster virus. Although rare in both people over and under 60 years old, it is more prevalent in those under 60. The most identifying characteristic of this virus being associated with uveitis is a nummular keratic precipitate. This means that there are lesions that appear in a coin shape in the stroma. They appear as an immune reaction to viral antigens [6]. Since the cytomegalovirus is so rare, it is usually only considered after a patient with symptoms of uveitis from other Herpesveridae viruses has been treated with corticosteroids as well as systemic antivirals. The cytomegalovirus virus in association with uveitis can usually be treated with oral antiviral medication called ganciclovir, but there is possibility for relapse after the treatments are ended [4]. Because the cytomegalovirus in uveitis is a relatively new finding, more work on this virus’s association with uveitis needs to be done. This is especially because its treatment, ganciclovir, has toxicity problems, and it remains unknown what effects may occur after extended use of it [4].
It is important to note during the treatment of these viruses, that the Herpesviridae family is made up of all DNA viruses. As DNA viruses, their genome is in the form of double stranded DNA. Because of this, any topical or oral agents used in their treatment will be effective through their anti DNA transcription properties [15]. These agents will help to stop the DNA of the viruses from getting read, which will stop their protein synthesis along with their replication [15].
Herpesviridae Cycle
The Herpesviridae virus needs multiple steps in order replicate. Because the Herpesviridae family is made up of viruses that all share the same structure, the cycle they all go through are similar. By explaining the cycle that the herpes simplex virus goes through, an understanding of all Herpesviridae virus cycles can be gained. First, the virion must attach to the host cell. The virion has multiple envelope proteins that are capable of binding to one of several receptors on the target cell surface. After attachment, the virion uses the glycoproteins in its envelope to fuse its membrane with the membrane of the host. After fusion is complete, the virus’s entire capsid is released into the host cytoplasm. This full herpes capsid will then travel down what can be considered a ‘scaffold’ of microtubules, where it will eventually reach the nuclear membrane where a pore is located. As this happens, there is a virion host shutoff factor, called Vhs, that will degrade the mRNA of the host, causing the host to cease its protein synthesis [8]. Then, the herpes capsid will inject its DNA through the nuclear pore into the nucleus of the host cell. This is possible through the high pressure in the capsid, caused by the double stranded DNA being in the relatively small capsid. Once inside the nucleus, the viral DNA forms a circle similar to a plasmid. The viral DNA in the nucleus is transcribed to mRNA by the RNA polymerase ll of the host. Then, the viral genome can either start the infection cycle or go for latent infection. For latent infection, mRNA is used to encode LAT proteins, which are responsible for maintaining the virus’s latency, which last for decades until it switches to being lytic. On the other hand, to start the infection cycle, lytic mRNA leaves the nucleus in order to be translated by ribosomes. After translation, the proteins, ready to be put into capsids, re-enter the nucleus. In order to create progeny genomes, the viral DNA still in the nucleus is replicated by viral enzymes along with some enzymes provided by the host cell, and the rolling-circle method of DNA replication is used to create concatemeric DNA. This new DNA will result in some late-stage mRNA, and it will leave the nucleus to be translated, which will result in some envelope proteins. Once they have been translated, the envelope proteins move back through the endoplasmic reticulum and back into the nuclear membrane. Then, the additional late proteins come back to the nucleus, where they get put inside capsids that have DNA in them that has been cleaved into linear chromosomes. After that, an envelope, which was created by the outer nuclear membrane, is formed around the capsid. Then, the virion is sent through the endoplasmic reticulum (where they get a second envelope) as they continue on their way to the Golgi. Finally, as they reach the cell membrane of the host cell, the second envelope fuses with the cell membrane, causing the host cell to release the virions through exocytosis. If many virions are released quickly, the host cells are killed, leading to the sores that are seen when someone has herpes.
Herpesviridae in Uveitis
Herpes Simplex Virus: During infections, herpes simplex viruses go through an inflammatory phase which causes problems in the eye. The herpes simplex virus induces certain proteins to be coded that are similar but slightly different than proteins in normal tissue. For instance, the herpes simplex virus has a protein in its coat called UL6, which is very alike to proteins that are in our cornea. Because of this, if our immune system learns to attack that virus, it also likely attack the natural protein as well. As a result, CD4+ T cells will activate, leading to a release of Th1 cytokines and chemokines, causing a harmful cascade of inflammation [15]. Also, there is a protein called glyco-protein K, that can be a reason for inflammation during viral infection. It prompts CD8+ T cells to gather near an inflammation site where they can cause scarring in the cornea [15].
The exact pathogenesis of the herpes simplex virus in uveitis remains unknown, and needs to be studied more. However, it is thought to utilize certain mechanisms such as ischemic vasculitis, lymphocytic infiltration of the iris stroma or intraocular nerves, or viral replication [12]. Also, repeated viral infection is thought to be able to cause an inflammatory reaction exhibited as uveitis, or it can cause the immune system itself to act against viral antigens, which will result in tissue and organ inflammation and damage [12].
Vericella-Zoster Virus: This virus cannot be removed by our immune system, and it stays in our sensory ganglia while latent. When our immune system is compromised, the virus can activate, which will result in hyperesthesia causing a rash on our skin. If the hyperesthesia occurs in the right sensory nerve (likely the first division of the fifth cranial nerve), then the infection can occur in a person’s ocular structures, causing uveitis, as well as other problems such as corneal scarring, glaucoma, and cataracts [15].
Complications and Prognosis of Herpesviridae Uveitis
When faced with herpes simplex virus uveitis, there are many possible complications the infected area may have to deal with. Chronic uveitis can lead to problems such as the cornea becoming clouded, increased eye pressure, cataracts, glaucoma, retinal swelling, and retinal detachment [13]. Each of these problems can lead to permanent blindness when they are severe enough. Herpes simplex virus and vericella-zoster virus can also cause karatitis.
Current Research
Since diagnosing uveitis caused by Herpesviridae is so important, yet so difficult, research is being performed to determine how to best discover the virus causing this disease. A study by Errera et al. (2012) [17] looked at the detection of Herpesviridae in anterior uveitis using real-time PCR and intraocular specific antibody secretion. Since time is a factor, especially with severe Herpesviridae uveitis, diagnosing it quickly is undoubtedly crucial, but the clinician must also ensure that the diagnosis is correct. The results from Errera et al.’s study (2012) [17] show that while both tests had some success diagnosing the disease (with real-time PCR doing so more quickly) because of their high specificity, and that they both had benefits, there are still other parameters that exist independent of the tests’ sensitivities that can cause a misdiagnosis. This shows that we have yet to find the best way to diagnose this disease, and that more research should continue to be done.
Conclusion
It is of utmost importance to be aware of and understand Herpesviridae viruses, as well as recognizing problems they can cause, such as uveitis. This is especially true for optometrists, as they must be able to identify and diagnose infected patients correctly. In some cases, an optometrist may not be enough and a specialist might be necessary. Without sufficient knowledge, it might result in misdiagnosed patients leading to serious complications. This is why more research is so essential in this area, so that the correct diagnosis can be made quickly, and then the best treatments can be given.
References
1.Brown, J.C., William W. Newcomb (2011). Herpesvirus Capsid Assembly: Insights from Structural Analysis. Current Opinion in Virology 1 (2): 142–149. doi:10.1016/j.coviro.2011.06.003. PMC 3171831. PMID 21927635.
2.Virus Pathogen Resource. About the Herpesviridae family. 2016. Web. http://www.viprbrc.org/brc/aboutPathogen.spg?decorator=herpes
3.Whitley RJ. Herpesviruses. In: Baron S, editor. Medical Microbiology. 4th edition. Galveston (TX): University of Texas Medical Branch at Galveston; 1996. Chapter 68. Available from: http://www.ncbi.nlm.nih.gov/books/NBK8157/
4.Doran, Marianne. 2009. Understanding and Treating Viral Anterior Uveitis. American Academy of Ophthalmology. http://www.aao.org/eyenet/article/viral-anterior-uveitis?september-2009
5.National Eye Institute. Facts about uveitis. 2011. Web. https://nei.nih.gov/health/uveitis/uveitis
6.American Academy of Ophthalmology. Herpes Zoster Ophthalmicus. http://www.aao.org/focalpointssnippetdetail.aspx?id=8367b620-245c-4ebf-89e7-eca0c8d35aa3
7.Mettenleiter, T. C. 2002. Herpesvirus Assembly and Egress. Journal of Virology, 76(4), 1537–1547. http://doi.org/10.1128/JVI.76.4.1537-1547.2002
8.Taddeo, B., & Roizman, B. 2006. The Virion Host Shutoff Protein (UL41) of Herpes Simplex Virus 1 Is an Endoribonuclease with a Substrate Specificity Similar to That of RNase A. Journal of Virology, 80(18), 9341–9345. http://doi.org/10.1128/JVI.01008-06
9.Los Alamos National Laboratory. Herpesvirus Family: Herpesviridae. 2001. Web. http://stdgen.northwestern.edu/stdgen/bacteria/hhv2/herpes.html#sub
10.iKnowledge. 2015. Uveitis. Web. http://clinicalgate.com/uveitis/
11.The ocular immunology and uveitis foundation. 2008. Pars Planitis. Web. http://www.uveitis.org/patients/support/parsplantis-org
12.Yao, Lijing, Agha Hassan Feroze. Herpes Simplex Uveitis. Web. http://www.uveitis.org/docs/dm/herpes_simplex_uveitis_scleritis.pdf
13.Haddrill, Marilyn, Gary Heiting, Michael DePaolis. 2014. All About Vision. Uveitis, iritis, and eye inflammation. Web. http://www.allaboutvision.com/conditions/uveitis.htm
14.Gritz, D; Wong, IG. 2004. Incidence and prevalence of uveitis in Northern California The Northern California Epidemiology of Uveitis Study.Ophthalmology 111(3): 491-500. doi:10.1016/j.ophtha.2003.06.014. PMID 15019324.
15.Potter, William B. 2010. An Overview of Ocular Herpetic Disease. Review of optometry. Web. https://www.reviewofoptometry.com/ce/an-overview-of-ocular-herpetic-disease
16.Nilm, LM, A Kozak, BH Feldman, M Doss, and V Bunya. 2015. Herpes Simplex Virus Keratitis. American Academy of Ophthalmology. Web. http://eyewiki.aao.org/Herpes_Simplex_Virus_Keratitis
17.Errera MH; P Goldschmidt; L Batellier; S Degorge; E Héron; L Laroche; JA Sahel; M Westcott; C Chaumeil. 2012. Findings In Detection Of Herpesviridae By Real-time Polymerase Chain Reaction And Intraocular Antibody Production In A Case-series Of Anterior Uveitis. Investigative Ophthalmology & Visual Science. Vol.53, 6166. http://iovs.arvojournals.org/article.aspx?articleid=2359865.
Authored for BIOL 238 Microbiology, taught by Joan Slonczewski, 2016, Kenyon College.
