Mycobacterium ulcerans in Africa
Classification
Higher Order Taxa:
Cellular organisms; Bacteria; Actinobacteria; Actinobacteria (class); Actinobacteridae; Actinomycetales; Corynebacterineae; Mycobacteriaceae; Mycobacterium
|
NCBI: Taxonomy Genome: - Mycobacterium ulcerans 1615 – Mycobacterium ulcerans Agy99 |
Summary
Mycobacterium ulcerans was first described in 1897. This bacteria causes severe ulcers on the skin in the late stages of buruli ulcer and can severely hinder a person's mobility. The disease's association with slow moving bodies of water has been established and there is an increasing awareness of insect vector transmission of the infection (Amofah, et al., 2002). Typically those that are affected by the BU are women and children; this could be due to their exposure to water more frequently (Senior, 2009). Yet another important trend is the recent global climate change impact has had on wetland habitats. The increased formation of wetland areas in Africa and enlarging rural populations engaged in basic agriculture in these wetlands can be an environmental factor (Senior, 2009).
History
The Buruli Ulcer is one of the most neglected but treatable disease of tropical areas. It is a disease caused by infection with Mycobacterium ulcerans. It has received less attention than various others under the same infectious agent. Other diseases such as tuberculosis and leprosy overshadow the extensive damage Buruli Ulcer can cause. The disease is known as the third most common mycobacterial disease after tuberculosis and leprosy in people who have normal immune systems (Van der Werf, et al). The Buruli Ulcer has been reported in over 30 countries and there is much speculation as to where else it may occur (Ortiz, et al, 2009).
The first description of skin ulcers in the region of Africa was in 1897 in Kampala, Uganda by Sir Albert Cook. The British physicians report from Mengo Hospital was the first most consistent recording with modern day Buruli ulcer. It was not until 1948, that a Professor in Australia, Peter MacCallum, again diagnosed the disease in 6 of his patients, giving it the name Bairnsdale ulcer. MacCallum and his colleagues were the first to isolate Mycobaterium ulcerans (World Health Organization, 2009).
In the 1960s there were multiple cases occurring in the present Nakasongola District of Uganda. At the time the region was known as Buruli county, which gave rise to the most prominently used name for the disease, Buruli ulcer. In 1989, Van der Werf described 96 cases in the Asante Akim North District of Ashanti Region (Amofah, et al, 2002). Emergence has rapidly escalated since the 1980s in various regions, and in particular that of West Africa. It was in 1998 that the World Health organization (WHO) realized the great public health important of the disease to many countries. In Ghana itself there were four regions reporting a total of 1,200 cases that year (Amofah, et al, 2002). WHO took action and established the Global Buruli Ulcer Initatiative. Recently in 2004 the World Health Assembly (WHA) has vouched to improve control of the Buruli ulcer and increase the amount of research being done on this disease. Currently in WHO monitored African regions at least 16 of the 41 countries report cases (Amofah, et al, 2002).
Buruli Ulcer In Africa
Cases of buruli ulcer have shown an increase in the number of patients admitted into CSNG (Centre Sanitaire et Nutritionnel Gbemoten) in southern Benin from 1992-1997, Oueme and Atlantique from 1992-2002, as well as other regions in Africa due to buruli ulcer (Debacker, 2004). Patients in the African area are most commonly affected by ulcers but may show nodules, plaques or odemas. Clinically, buruli ulcer in the skin is divided into three categoires: nonulcerative forms (papules, nodules, indurated plaques, or edemas), ulcerative forms, and the healing or scarring forms. Bone lesion forms also exist (Debacker, 2004). In addition, Buruli Ulcer also causes illness and long-lasting negative socioeconomic effects in rural areas (Benbow, 2008)
Risk factors for contraction of the disease in Africa are places nearby stagnant or slow running water. Buruli Ulcer occurrences may have also increased due to human-made modifications that include agricultural activities, deforestation, mining and construction of dams, which are sources of stagnant water. Such activities seem to have a direct correlation to the increased frequency of the disease as diamond mines along the Cuango River in Angola may have influenced the emergence of the disease in the region (Kibadi, 2008). In addition, many animal species have tested positive in the endemic areas of Africa. Most studies indicate that infection occurs through inoculation of M. ulcerans into skin lesions of aquatic insect bites, however, a specific vector for the disease to people has not been convincingly identified and insect bites seems an unlikely vector in more recent studies (Benbow, 2008).
There is much done to in response to the disease in endemic areas such as Benin, West Africa where the disease has become the second most important mycobacterial disease after tuberculosis. In Benin, five BU Detection and Treatment Centers (CDTUB) are dispersed throughout BU-endemic regions. Cases are detected and followed-up by community-based surveillance teams nearest the health facility. A trained nurse then registers each case on a BU02 form, which is sent to the national level, regional and local levels. These records show that 51% of the 2,598 cases were in children less than 15 years of age and cases were equally distributed between male (49.7%) and female (50.3%) patients (Sopoh, 2007).
Patient duration of hospitalization decreased in 1997-2001 to 1-2 months for all forms of the disease except those affected by nodules, which may be due to reduced patient delay (median of 20-46 days (nonulcerative), 61-91 days (ulcerative)) or better care (Debacker, 2004). It is unlikely that this period will be further reduced considerably for advanced buruli ulcer disease victims with current therapies (Debacker, 2004).
Reduction in the number of cases has dropped recently in severeal regions in response to many factors. Some past and present steps taken are: intensive publicity on buruli ulcer, promotion of treatment in local villages, and minimalized transportation costs by frequenting local practioners (Debacker, 2004). Currently, more work is being done to lower the amount of untreated cases and treatment costs, as well as prevention of disease from occurring because of fear of surgery and lack of access to practioneers for locals in buruli ulcer endemic regions.
Disease
Buruli Ulcer occurs in areas near bodies of water that are hot and humid, with West Africa being the most affected region. This ulcer is most commonly found in adolescents, ages 5 to 15 years old, and doesn’t discriminate based on gender (Van der Werf, et al., 2005). It is thought that the microbe is transmitted by contaminated water, soil, and vegetation through open sores or small lacerations on the skin. There was one unconfirmed case of transmission by insects. Small, raised, painless nodules on the skin, is a sign of the early stages of the disease. Typically, this nodule can be removed with minor surgery. Unfortunately, many people who are affected by the disease live in rural areas of West Africa. They are either afraid of surgery or don’t have the economic means to allow a family member to stop working in order to take care of the sick person. This leads to seeing more patients coming in with the late stages of the disease affecting them. They have large ulcerated regions on their limbs that are very hard to surgically remove and cure. In the advanced stage, it is hard to treat because the patient can relapse or be affected secondarily by other systemic problems. The large ulcerative region can leave extensive scarring which hinders the person from being able to work at their full potential. This can be a great economic burden to them and their family (Van der Wer, et al., 2005).
Microbe
Mycobacterium ulcerans is a slow growing mycobacterium with a doubling time of 80 days (Marsollier, 2004). It inhabits water where it can colonize aquatic plants, herbivorous animals and aquatic insects. This mycobacterium stains red in response to the neutral red cytochemical reaction and gives positive results to the catalase test. (Yaoi, 1957)
Comparative genomic analysis showed that M. ulcerans evolved from Mycobacterium marinum by horizontal transfer of a virulence plasmid encoding for mycolactone production. The plasmid as well as the insertions and deletions were crucial for its emergence as a pathogen (Demangel 50). For instance, the plasmid gained from Mycobacterium marinum lost its ability to express ESAT-6, CFP-12 and HspX proteins. The loss of these immunodominant proteins helps it evade its host’s immune response. In addition, the mycolactone produced by M. ulcerans is the cause of Buruli Ulcer and is essential for colonization of salivary glands of N. cimicoides, a host and vector for the mycobacteria (Huber, 2008).
M. ulcerans produces a biofilm on the surface of aquatic plants and, in addition, surrounds the biofilm by an extracellular matirix (ECM) on insect and mammilian hosts. Like some other biofilms, it provides increased protection under diverse environmental conditions, resistance against antibodies, and facilitates colonization. In contrast to other bacterial biofilms, however, the ECM M. ulcerans produces is a thick layer surrounding only the outermost layer of the mycobacteria where it accumulates mycolactone in vesicles for secretion. (Marsollier, 2007)
The loss of expression of ESAT-6, CFP-12 and HspX proteins and biofilm formation allows M. ulcerans to proliferate on the host extracellularly to release mycolactone.
Mycobacterium ulcerans is found mostly in wetlands of tropical and subtropical regions in following regions:
Africa: Benin, Burkina Faso, Côte d'Ivoire, Ghana, Liberia, Nigeria, Togo, Guinea, Sierra Leone, Angola, Cameroon, Congo, Democratic Republic of Congo, Equatorial Guinea, Gabon, Sudan, Uganda Asia: China, Malaysia, Japan. Western Pacific: Australia, Papua New Guinea, Kiribati Americas: French Guyana, Mexico, Peru, Surinam.
Strains from Africa produce the highest degree of inflammation, necrosis and bacillary loads. (Ortiz, 2009)
The similar ecology that the regions share suggests that environmental factors play a role in the proper development of M. ulcerans. Ideal growing temperature of M. ulcerans is 30°C- 33°C, typical of tropical regions. Further evidence supporting that M. ulcerans is dependent on environmental factors is shown as the normal doubling time of 80 days in cultured M. ulcerans is doubled in a medium consisting of freshwater green algae Rhizoclonium and Hydrodictyon or their extracts (Marsollier, 2004).
Pathology
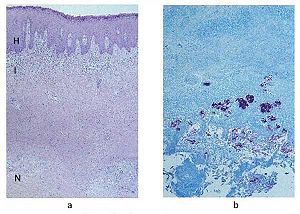
Once inside the host, the incubation period of Mycobacterium ulcerans, on an average, is said to be between 2-3 months. Early stages of infection of M. ulcerans are governed by two factors: a) toxin produced called mycolactone and b) its optimum growth temperature between 30-33oC. The toxin, mycolactone, produced by the bacteria is extremely damaging to the living tissue (especially skin and bones) (World Health Organization).
Upon invasion on to the dermis cells (lower skin layer), M. ulcerans goes through a latency period where it takes a while to grow enough to be able to make the mycotoxin, which then eats away the skin around it. It has been found that necrosis of the fatty tissue speeds up the process of growth of M. ulcerans. During extensive erosive phase of this disease, there is no immune response from the host side and even tests done for the disease remain negative. It is thought that the lack of immune response towards the toxin might be because the toxin might have already been neutralized or that it was no longer produced. Once the toxin ceases to be produced the body goes into recovery, in which case there are antibodies seen in the blood and healing is seen (Asiedu K et al). It is postulated that bacteria start to die because of the lack of nutrient in the infected area, and once that happens the immune response is initiated.
According to the Armed forces Institute of pathology, the disease can manifest itself via different pathways. After the initial infection, the disease can be either localized or delocalized. If the disease is more localized, then formation of nodes is seen at the bottom of the skin which gradually eats its way thorough the surface. The disease can also pass the localized ulcerative phase and progress straight to the delocalized phase causing plaques filled with liquid, if left untreated. The infection generally spreads through the lymphatic system to different locations of the skin and bones.
There are several different form of lesions seen in this disease, which are listed as follows:
- 1. The Nodular lesion: they are formed at the initial stages of the disease and about 2cm wide. These lesions are painless.
- 2. Minor ulcerative lesion: the ulcer is small and the bacteria is colonized and limited to the center of the lesion.
- 3. Major ulcerative lesion: small to large ulcers. The ulcers are surrounded by edematous tissue. The bacteria is present around the base of the ulcers and closer to the boarder of the lesions.
Current Methods
The first and foremost method of addressing Buruli ulcer is prevention of the initial infection. Unfortunately, after inoculation by the bacteria there is little that can be done from preventing the bacterial spread. Early detection of the bacterial infection, before any visible skin formation has surfaced, is one solution. This can be done via a diagnostic test. Upon inoculation of the virus into the host, a toxin called mycolactone diffuses from the infected tissues and travels into the blood stream and spleen. This toxin displays significant immunosuppressive effects, which ultimately leads to the formation of the ulcers. Early diagnostic testing’s can detect the presence of the mycolactone toxin well before the ulcer develops, allowing sufficient time to kill the bacteria before severe damage has been done (Hong et al, 2008). There are currently several effective treatments for killing the bacteria, each with their own pros and cons.
Currently the World Health Organizations recommends management of the bacteria with a combination of rifampicin and streptomycin/amikacin for eight weeks as a first-line treatment for all forms of the active disease, along with surgical removal of the infected tissue (WHO 2004). The bacterium responds very well to this treatment, and the prognosis of patients whom have undergone the treatment is very good. Unfortunately, many third world countries do not have access to the costly antibiotics, nor do they have the proper medical staff and resources to perform sterile surgical removal of the infected tissue. The drugs necessary for the treatment are rarely available, and often times many people with the condition do not even have the means to be seen by a physician. This has caused a great need for cheaper and easier treatments of the bacterial infection. For this reason several other low cost, holistic approaches have been developed, and tested by scientists, in hopes of finding an easier and more cost efficient method of treating Buruli ulcer.
One such low cost, holistic approach is the use of green clay on the infected tissue. The absorptive and microbial properties of clay minerals have been used for many generations as healing ailments (Williams et al, 2009). Researches have recently assessed the use of this green clay as an inexpensive treatment for the ulcer. Line Brunet de Courssou, a French humanitarian working in the Ivory Coast with many people having Buruli ulcer, developed the treatment. A hydrated form of the clay is applied on the entire surface of the patients skin. One day after the initial clay application, rapid and non-surgical deterioration of the damaged tissue can be seen. After continuous treatment wound healing and healthy tissue regeneration has been shown to occur (Williams et al, 2009). The actual mechanism of the clay is still being debated, but it is thought that the clay may promote bacterial growth, which in turn vamps up the immune response to the site, and therefore rendering the immune system more efficient to attack and destroy the bacteria.
A heat application therapy is also another low cost yet effective method of treating the bacteria. Mycobacterium ulcerans, grows best at 30°C–33°C and not above 37°C. Sodium acetate trihydrate, which is found in most over the counter heating pads, can be applied to the infected skin regions. These heating pads are easy to apply, rechargeable in hot water, non-toxic, and non-hazardous to the environments (Junghanss et al 2009). This method of treatment has shown to completely heal wounds caused by the bacteria, as well as kill the bacteria itself, preventing a relapse. The bacteria are unable to withstand the constant application of heat, and are eventually totally destroyed rendering the patient healthy.
Improving The Situation
Studies have shown a close association between buruli ulcer and wetlands, slow flowing and stagnant water (Kibadi, 2008). Diamond mining occurs in the wetlands next to the Kwango/Cuango River. Miners often work long hours digging for diamonds with basic equipment and often with unprotected hands and feet. (Kibadi, 2008) Water sources along the river are unprotected and hygienic procedures are lacking (Kibadi, 2008). This is the current situation that contributes to the spread of buruli ulcer in West Africa. Improvements can be as simple as increasing hygienic practices to improving work environments. The world health organization has created a control strategy to help minimize the spread of the disease (WHO, 2009). The strategy calls for strengthening of existing health systems, activities for early detection, standardized case management, supervision, monitoring and evaluation of control activities, social mobilization and partnerships, and research. (WHO, 2009). All of these have been set to minimize the morbidity and disability associated with buruli ulcer.
Other preventative measures include the development of a vaccine against Mycobacterium ulcerans or the toxins that it may produce (Van de Werf, et al., 1999). Although it is stressed that the first line of defense be small things such as putting on trousers as a mechanical defense against contaminated material (Van de Werf, et al., 1999). Other mycobacterium in the environment trigger a cell mediated immune response (Van de Werf, et al., 1999). Although an effective vaccine has not been developed it is by no means unattainable. Currently the BCG vaccine has proven effective at protecting against the buruli ulcer but is not a complete protection (Van de Werf, et al., 1999). More work and research needs to be done on creating an affordable vaccine to protect against formation of buruli ulcers. Work should also be focused on preventative measures. Providing good working conditions for diamond miners and providing citizens with basic knowledge of sanitary practices will likely improve the situation. The buruli ulcer is a testament to how when basic needs are not met endemics develop.
References
Amofah, George, et al. “Buruli Ulcer in Ghana: results of a National Case Search.” Emerging Infectious Diseases. 8 (2002): 167-170.
Benbow, M. Eric. “Aquatic Invertebrates as Unlikely Vectors of Buruli Ulcer Disease.” Emerging Infectious Diseases. 14.8 (2008): 1248-1253.
“Buruli ulcer (Mycobacterium ulcerans infection)” World Health Organization 2009. The World Health Organization 25 August 2009 [1]
“Buruli ulcer: Pathogenesis” Armed Forces Institute of Pathology 4 February 2004. The Armed Institute of Pathology 25 August 2009. [2]
Debacker, Martin, et al. “Mycobacterium ulcerans Disease (Buruli Ulcer) in Rural Hospital, Southern Benin, 1997–2001.” Emerging Infectious Diseases. 10.8 (2004): 1391-1398.
Demangel, Caroline, et al. "Buruli ulcer: reductive evolution enhances pathogenicity of Mycobacterium ulcerans." Nature Reviews Microbiology 7 (2009): 50-60.
Hong, Hui, Emmanuelle Coutanceau, and Marion Leclerc. "Mycolactone Diffuses from Mycobacterium ulcerans-Infected Tissues and Targets Mononuclear Cells in Peripheral Lymphoid Organs." PLOS Neglected Tropical Diseases 2.10 (2008)
Huber, Charlotte A., et al. "Independent Loss of Immunogenic Proteins in Mycobacterium ulcerans." Clinical And Vaccine Immunology 15.4 (2008): 598-606.
Junghanss T, Um Boock A, Vogel M, Schuette D, Weinlaeder H, Pluschke G. Phase Change Material for Thermotherapy of Buruli Ulcer: A Prospective Observational Single Centre Proof-of-Principle Trial. PLoS Neglected Tropical Diseases. 2009;3(2):e380.
Kibadi K, et al. "New foci of Buruli ulcer, Angola and Democratic Republic of Congo." Emerging Infectious Diseases. 2008 Nov.
Marsollier, Laurent, et al. "Aquatic Plants Stimulate the Growth of and Biofilm Formation by Mycobacterium ulcerans in Axenic Culture and Harbor These Bacteria in the Environment." Applied And Environmental Microbiology 70 (2004): 1097-1103.
Marsollier Laurent, Brodin P, Jackson M, Korduláková J, Tafelmeyer P, et al. "Impact of Mycobacterium ulcerans Biofilm on Transmissibility to Ecological Niches and Buruli Ulcer Pathogenesis." PLoS Pathog 3.5 (2007): 582-594.
"Objective and strategy for control and research" World Health Organization. 2009. The World Health Organization 25 August 2009 [3].
Ortiz, Hurtado, et al. "Differences in virulence and immune response induced in a murine model by isolates of Mycobacterium ulcerans from different geographic areas." Clinical and Experimental Immunology 157.2 (2009): 271-281.
Senior, Kathryn, “Buruli Ulcer: Dare we ignore it?” The Lancet. 9 (2009) 273. The Lancet 28 August 2009. [4]
Sopoh, Ghislain Emmanuel, et al. “Buruli Ulcer Surveillance, Benin.” Emerging Infectious Diseases. 13.9 (2007): 1374-1376.
Van der Werf, Tjip S., et al. “Mycobacterium ulcerans infection.” The Lancet. 354 (1999): 1013-1018
Van der Werf, Tjip S., et al. “Mycobacterium ulcerans disease.” Bulletin of the World Health Organization. 83 (2005): 785-791.
Williams, Lynda B., Shelley E. Haydel, Rossman F. Giese, and Jr. Eberl. "Chemical and Mineralogical Characteristics of French Green Clays Used for Healing." Clays and Clay Minerals 56.4 (2009): 437-52.
World Health Organization. Provisional guidance on the role of specific antibiotics in the management of Mycobacterium ulcerans disease (Buruli ulcer). World Health Organization; Geneva, Switzerland: 2004.
Yaoi, H, et al. "Biological studies on Mycobacterium ulcerans (MacCallum). I. Outline of the characteristics." Clinical And Vaccine Immunology 1.1 (1957): 29-35.
Pictures courtesy of CDC
Edited by: Arshi Jaha, Brian Lim, Bridget Flannery, Christina Mcquaid, Emmanuel Guerrero, and Paulina Lopez, students of Rachel Larsen.


