Naloxone Hydrochloride
Pharmacology of Naloxone Hydrochloride
Author: Alexander Gant Van Vliet

Naloxone hydrochloride, known by the brand name Narcan, is an opiate antagonist medication used primarily to reverse or lessen the effects of an opiate overdose. [2][8] It was first synthesized in 1982 by Jack Fishman of Rockefeller University. Later that year, Harold Blumberg of New York Medical College, found that the newly synthesized drug was a “potent, rapid-acting, and relatively pure narcotic antagonist. ”.[7] When delivered into the blood stream it travels to the brain. Naloxone’s hydrophilic properties allows it to easily cross the blood brain barriers where it can make its way to the opiate receptors of the brain and, due to its high affinity for the opiate receptors it outcompetes opiates and binds to the receptors. The three opioid receptors are the mu, kappa and delta receptors. They all have analgesic (pain relieving) properties when activated however the mu receptor also causes respiratory depression. [3] This is important for naloxone because it has the highest affinity for the mu receptor. In a person with any levels of opiates, whether naturally or artificially there, naloxone will prevent those opiates from binding and affecting the opiate receptors. This in turn stops any symptoms of an opiate overdose, and thus the reason for its use in overdoses.
Naturally occurring opiates come in the form of endorphins in your body. They are vitally important to short term survival in critical situations. Endorphins will bind to the opioid receptors and create a temporary effect by blocking pain. They are released following injury and can give a person time to remove them selves from a dangerous situation.[4] The effect of endorphins is short lived and they eventually detach from the receptor and pain ensues. This is why you often don’t feel pain immediately after getting injury.
When there is no presence of opiates in the brain naloxone will continue to bind to the opiate receptors, however it won’t have any symptomatic effects either positively or negatively. This is due to the fact that it is a pure opioid receptor antagonist. This means that it has no agonist effect, which in this case would be a stimulation of the opiate response.[2][8] Earlier opioid receptor antagonists, like nalorphine, had antagonistic effect on one of the receptors but had an agonist effect on another making it inefficient at treating overdoses. Again for this reason naloxone is an ideal medication for opiate overdoses, because even if it is not an opiate overdose there is no adverse effects of giving the medication. This unique pharmacological effect has lead to the universal adaptation of the use of naloxone in any person with suspected opiate overdose.
Opiate Receptors and Signs of an Overdose
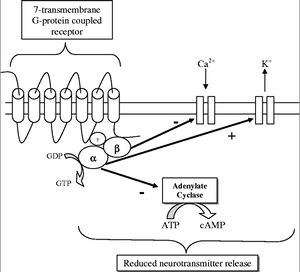
The opiate receptors are 7-Transmembrane G-Protein Coupled Receptors (GPCR), outlined in Figure 2. When the ligand (opiate) binds to the receptor on the transmembrane protein it causes an exchange of GDP for GTP on the alpha subunit of the protein, which causes both the alpha and beta subunit to disassociate from the receptor protein. This disassociation has three effects. The first is the closing of voltage sensitive Ca2+ channels. The second is the pumping out of K+. This hyperpolarizes the neuron. The third step is the inhibition of adenalyte cyclase, which prevents the conversion of ATP to cyclic adenosine monophosphate (cAMP). cAMP is an important secondary cell signaling molecule. All of this contributes to a reduction in function of the cells by not allowing the release of neurotransmitters, which are vital to cell signaling and transmission of a signal.[9]
When the GTP is hydrolyzed into GDP the alpha and beta subunits reassemble and rebind to the receptor protein and the ligand disassociates and the signal given by the opiate G-Protein Coupled Receptor is terminated. The inhibition of neurotransmitters in neurons is what gives opiates its analgesic or pain relieving effects. When an excess of opiates are taken there is an effect on breathing due to the lack of the ability of neurons to detect changes in CO2 levels due to dampening of signals passed on by carbon dioxide chemoreceptors.[9] What kills persons from an opiate overdose is respiratory depression leading to respiratory arrest and then cardiac arrest. The signs of current opiate overdose are known as the “opiate overdose triad”. Those three symptoms are pinpoint pupils, unconsciousness, and respiratory depression. Left untreated this will lead to death.
Use in EMS and Prehospital Care
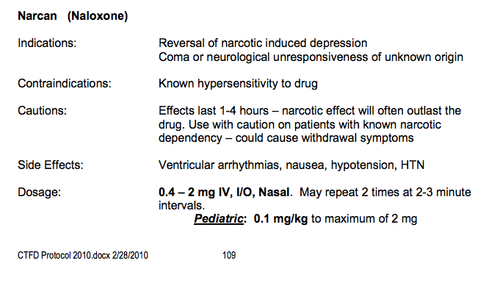
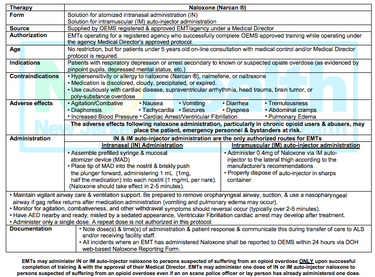
Due to the high prevalence of abuse of opiates, naloxone is especially popular among prehospital EMS responders. Over the counter opiate analgesics account for about 72 percent of the recorded prescription drug abuse cases in the United States.[10] The increasing abuse of illegal opiates such as heroin and opium has also lead to an increasing push for the use of naloxone in prehospital care. Many fire departments carry a similar protocol to the one pictured in Figure 4, taken from the state of New Jersey naloxone drug protocol. As shown the indication for the use of naloxone is “Patients with respiratory depression or arrest secondary to known or suspected opiate overdose (as evidenced by pinpoint pupils, depressed mental status, etc.)”. Due to its very minimal side effects many protocols suggest the use in any sort of “suspected opiate overdose” giving the power to the EMS provider to constitute what that suspicion is. It is for this reason that naloxone has been used almost as diagnostic tool because if the patient does not revert from their symptoms from aggressive treatment of nalxone it is most likely not an opiate overdose and thus the EMS or hospital provider can start trying to figure out another possibility for the current symptoms. This has been furthered by paramedic theory that any unconscious persons of unknown origin should get the administration of D50 (50% dextrose solution used for reversing of diabetic hypoglycemia emergencies) and naloxone since those are the two most likely reasons for a person’s unconsciousness.
There are some varying opinions on the ideal dosage and administration of the drug. The standard naloxone administration set, as shown in Figure 1, comes with a prefilled syringe with 2 milligrams of drug, dissolved in 2 milliliters of saline. This gives it a 1:1 ratio of drug in solution making it easy to administer specific quantities. The quantity given depends greatly on the route of administration. There are three routes used for administration. The first is via a previously established intravenous line (IV line). This is a direct way to administer the drug directly into the bloodstream. As one would expect there is a very quick time of onset associated with this route at around 2 minutes. The downside of this is it requires the establishment of an IV line. This can be difficult due to IV catheterization being a fairly technical skill and the possibility that the veins might not be useable due to previous IV drug abuse like heroin. The second route of is via an intra-muscular injection (IM shot). This is just like any normal shot you would get at a doctor. A small gauge hypodermic needle is used to inject the drug into the muscle of the leg or deltoid muscle in the shoulder. As long as perfusion of blood to those muscles is good there is a rapid absorption of it into the blood stream. The issue with IM injections is that during opiate overdoses, especially with respiratory compromise, blood is shunted away from the skin and muscles and to the vital organs in order to keep the person alive. Thus if perfusion of blood to the skin and muscle is poor, then the drug will not be transported to its effector proteins in the brain. Along with that it still requires the use of needles, which requires fairly extensive EMS training to be used. This issue was somewhat solved with the creation of naloxone auto-injectors that work much like an epi-pen. The final method is via intra nasal sprays (IN sprays). This is done by a mucosal atomizer device, also called a mad device. It is attached to the prefilled syringe (as it is included in most naloxone kits) and it creates a spray of the solution, which can be sprayed up the nose where it will absorb into the capillaries of the mucosal membrane. The use of the MAD device has gained popularity due to its easy set up and because it takes little training to be able to be used properly. The downside with this route of administration is that it is the least efficient at delivering the drug to the brain, and thus more of it has to be used.[4]
Dosages as mentioned above varies based on the route of administration. As exemplified by the New Jersey state naloxone protocol (Figure 4), the dosage of naloxone via IN administration is 1 milligram in each nostril resulting in a total dosage of 2 milligrams. The dosage for IM and IV administration is about .4 milligrams due to the more direct route into the blood stream.
Many EMS protocols include the ability to use more of the drug until you reach the desired effect. This is usually written as “titrate to effect”. The “desired effect” is to restore proper respiratory function. As shown by the College Township Fire Department protocol (Figure 4) the dosage can be repeated twice with two to three minute intervals in between. What is often not understood is that a reestablishment of proper respiratory function does not always have to correspond with reestablishing consciousness in the person. Unconsciousness in and of itself is not an immediate danger to a person’s life. The danger comes when you have a threat to airway, breathing or circulation. Ideally naloxone administration would be sufficient to restore proper breathing but not to restore consciousness. This is due to the fact that sudden opiate withdrawal can lead to dangerous side effects for the person as well as the caregiver. Some of the more severe side effects of narcan administration due to sudden opiate withdrawal include nausea, vomiting, diarrhea, and agitation. As experienced by many EMS providers who have successfully used naloxone all four of these can happen to an extreme extent.
Onset and Duration of Naloxone’s Effect
One of the most important considerations is the time it takes naloxone to take effect (time of onset) and how long that antagonist effect will last for. The half-life of narcan is about 60-90 (almost the same as morphine, a common opiate analgesic) minutes however it is quickly redistributed away from the brain meaning it will not have a 60-90 minute effect of blocking the opiate receptors. Thus, even though naloxone might have similar half-life to opiates its effect will not last as long. Since this is true administration of naloxone does not insure a cure to the opiate overdose but rather a temporary antagonist. [11] The fear with this is that a person will be given naloxone, recover from their overdose and then suddenly relapse later when the narcan has been removed and the opiates rebind to the opiate receptors and the person can relapse into an opiate overdose.
Layperson Use of Naloxone

Due to naloxone’s immediate antagonist effect and few contraindications there has been a movement to see to it that it become more immediately available to persons other than EMS and doctors. It is often found that the first person on scene of an opiate overdose is a friend or a parent and their ability to use the drug could change the outcome of many overdose patients. In October of 2015 Pennsylvania passed the “Heroin Antidote Law” allowing police to administer naloxone and allows doctors to prescribe the drug to family and friends of drug addicts.
The pharmacy CVS in September of 2015 approved the selling of naloxone over the counter in states in which it was legally allowed to (Arkansas, California, Minnesota, Mississippi, Montana, New Jersey, North Dakota, Pennsylvania, South Carolina, Tennessee, Utah, and Wisconsin).[13] This took away the necessity of getting a prescription from a doctor and has allowed many more lay people to get their hands on the drug.
There are some limitations and concerns with layperson use of naloxone. The first being the possibility of an overdose patient relapsing into an overdose after the effect of the naloxone has worn off. Studies have shown that even though naloxone has a shorter effect and half-life than opiates like heroin relapse into an overdose is rare. In a study conducted in Chicago out of 319 peer administrated naloxone injections, not one of them resulted in a reoccurrence of overdose symptoms.[12] It is also argued that should this issue arise a second dose can easily be re-administered. The second concern is that prescription of naloxone will promote the use of dangerous opiate practices by either using more frequently or in higher doses. It was found that the acute withdrawal symptom side effects of using naloxone often discourages risky drug abuse habits and actually increases the desire to seek treatment. A third limitation is due to the lack of efficiency of distributing naloxone to at risk persons. Although distribution programs have been shown to be successful they select for a very specific group of opiate users. For example one Chicago distribution center, the Chicago Recovery Alliance, distributed 10,000 vials of naloxone and there was a reported 972 verified reports of naloxone reversing opiate overdoses.[12] Other studies have shown that it would take about 110 naloxone kits handed out to the general population to prevent one death. [1] However many distributing centers, such as that one, are associated with needle exchange centers whose target audiences are heroin abusers. With the increase of prescription opiate abuse, programs would have to be developed in order to provide naloxone to those all of those at risk.
Additionally it is feared that bystander of layperson use of naloxone will discourage the additional step of getting the person definitive care at a hospital. This is due to the fear that EMS or hospital involvement will bring along police and criminal prosecution for the possession of illegal narcotics. In fact many states have Good Samaritan laws that prevent criminal prosecution if 911 is called to report an overdose. For example Washington state law was revised to include this statement protecting good Samaritans. “ A person acting in good faith who seeks medical assistance for someone experiencing a drug-related overdose shall not be charged or prosecuted for possession of a controlled substance pursuant to RCW 69.50.4013, or penalized under RCW 69.50.4014, if the evidence for the charge of possession of a controlled substance was obtained as a result of the person seeking medical assistance.” This was in response to the number of overdose deaths in the state of Washington, increasing from 403 to 761 from 1999 to 2007 and surpassing the number of motor vehicle accident (MVA) deaths (610 deaths in 2007).[6] Other states have adapted similar laws to help save lives and get help to those who need it, however it has to be universally adapted if it wants to have the impact it is going for because in the moment of panic people are not going to want to look up if their state has a Good Samaritan policy protecting them or their friend from criminal prosecution in a overdose situation.
The final issue with layperson use of naloxone comes from the issue that it shouldn’t be truly given by a “layperson” who is not an expert in a given subject. Studies in which analysis was done in cases in which a bystander giving naloxone was trained, to some extent, in the use of the drug versus the bystander having no training the outcome showed that trained persons had significantly higher effectiveness in reversing overdoses. This is to be expected. The most universally used method is via a MAD device spraying the drug. In order for it to be effective the syringe and MAD device have to be put together properly and 1ml of drug has to be sprayed in each nostril because that is the maximum amount of liquid that can be effectively sprayed into a nostril and deliver the maximum amount of drug and not just be passed on into the digestive system. Also in the two to five minutes before the drug takes effect persons may have to monitor the persons airway and maybe even give rescue breaths to give the drug time to take effect.
Layperson sue of naloxone has been made easier by the creation of naloxone auto-injectors (Figure 5), which give the person an IM injection into the quadriceps muscle of the leg. They come in a prefilled auto injector that actually has audible voiced commands. The dose is .4 milligrams and all of it is given in the one use auto-injector. The prescription set comes with two auto-injectors and a trainer. Having the second dose available would allow the person administering it to be able to give a repeat dose if the first one is not enough or if the person goes back into an overdose. The downside of this unit is that it is fairly costly at about 580 dollars per unit.[5] The alternative is the nasal spray version which, although maybe slightly less effective, cost only about 20 dollars and can be obtained for free at many clinics.
There have been recorded cases of hepatotoxicity with use of nalxone in persons with past history of hepatitis c infection. Hepatotoxicity is damage of the liver due to chemicals, which in this case would be the naloxone itself. Studies done have found that the chances of this happening increases with multiple uses of naloxone and that current infection of hepatitis c increases the risk of liver damage. That being said the prevalence of hepatotoxicity in narcan users is "rare at most". [14]
Conclusion
Naloxone hydrochloride is a very important, life saving opiate antagonist. The massive increase of the malicious and accidental overuse of over the counter and illegal opiate narcotics has pushed naloxone into the forefront on the fight against drug related deaths. Its use in prehospital EMS and bystanders has been proven to save the lives of many accidental overdose patients. Its pure antagonist effects, easy administration via IN sprays, and very few side effects make it the ideal drug of choice for reversing life threatening opiate overdoses. Issues still remain however. It is not a definitive treatment for drug abuse but merely a temporary solution to a deadly issue. Its use does not always provide the definitive care needed to prevent further overdose attempts. Revisions to current laws have lessoned the criminal repercussions of reporting opiate overdoses and have allowed a bigger outreach of the drug. Issues still remain however in the widespread distribution and training in the use of naloxone. In order to have the impact it is capable of, cheap and easy distribution of the drug will have to be perfected.
References
(1) "Naloxone for Heroin Overdose Reversal." Naloxone Info 158.1 (2013): n. pag. Web. <http://naloxoneinfo.org/sites/default/files/Cost%20Effectiveness%20Summary_EN.pdf>.
(2) "Naloxone (Naloxone Hydrochloride) - Description and Clinical Pharmacology." Naloxone. DrugLib, n.d. Web. <http://www.druglib.com/druginfo/naloxone/description_pharmacology/>.
(3)"Opioid Receptor." Wikipedia. Wikimedia Foundation, n.d. Web. 16 Nov. 2015. <https://en.wikipedia.org/wiki/Opioid_receptor>.
(4) Barker, Karen. "Meet Narcan: The Amazing Drug That Helps save Overdose Patients." - Journal of Emergency Medical Services. JEMS, n.d. Web. <http://www.jems.com/articles/print/volume-33/issue-8/patient-care/meet-narcan-amazing-drug-helps.html>.
(5) Bebinger, Martha. "I Bought Narcan, And Here’s What I Learned." CommonHealth RSS. N.p., 6 June 2015. Web. <http://commonhealth.wbur.org/2015/06/narcan-naloxone-evzio>.
(6) "RCW 69.50.315: Medical Assistance-Drug-related Overdose-Naloxone-Prosecution for Possession." Washington State Legislator. N.p., 2015. Web. <http://apps.leg.wa.gov/rcw/default.aspx?cite=69.50.315#footerAnchor>.
(7) The 1982 John Scott Award Goes to Jack Fisbman and Harold Bhunberg for Synthesfs and Investfgatfon of Naloxone (n.d.): n. pag. Web. <http://garfield.library.upenn.edu/essays/v6p121y1983.pdf>.
(8) "Narcan (Naloxone) Drug Information: Clinical Pharmacology - Prescribing Information at RxList." RxList. N.p., n.d. Web. <http://www.rxlist.com/narcan-drug/clinical-pharmacology.htm>.
(9) McDonald, John. "Opioid Receptors." Medicine and Health. N.p., n.d. Web. <http://ceaccp.oxfordjournals.org/content/5/1/22.full>.
(10) Sciuto, Laura. "Which Prescription Drugs Do Americans Abuse Most?" PBS. PBS, 30 Apr. 2013. Web. <http://www.pbs.org/newshour/rundown/which-prescription-drugs-do-americans-abuse-most/>.
(11) Clarke, S., P. Dargan, and A. Jones. "Naloxone in Opioid Poisoning: Walking the Tightrope." Emergency Medical Journal. N.p., 1 Apr. 2014. Web. <http://emj.bmj.com/content/22/9/612.long#ref-32>.
(12) Kim, Daniel, Kevin S. Irwin, and Karen Khoshnood. "Expanded Access to Naloxone: Options for Critical Response to the Epidemic of Opioid Overdose Mortality." American Journal of Public Health. American Public Health Association, Mar. 2009. Web. <http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2661437/#bib6>.
(13) Grush, Lauren. "CVS Pharmacies in 12 More States Will Carry Drug to Treat Heroin Overdose." The Verge. N.p., 25 Sept. 2015. Web. <http://www.theverge.com/2015/9/25/9398823/naloxone-heroin-overdose-cvs-stores-over-the-counter>.
(14) Saxon, Andrew. "Topic: Treatment of Acute Pain in Patients Receiving Buprenorphine/naloxone." Providers Clinical Support System (n.d.): n. pag. Web. <http://pcssmat.org/wp-content/uploads/2014/03/PCSS-MATGuidanceMonitoringLiverFunctionTests-and-HepatitisInBupPatients.Saxon_.pdf>.
Authored by Alexander Gant Van Vliet for BIOL 291.00 Health Service and Biomedical Analysis, taught by Joan Slonczewski, 2016, Kenyon College.
