Neisseria meningitidis -- Meningitis

Etiology/Bacteriology
Taxonomy
| Domain = Prokaryote | Phylum = Proteobacteria | Class = Betaproteobacteria | Order = Neisseriales | Family = Neisseriaceae | Genus = Neisseria | species = Neisseria meningitidis
Description
Neisseria meningitidis is an aerobic, Gram-negative diplococcus that causes meningococcal diseases such as meningococcemia and bacterial meningitis. Meningitis arises upon inflammation of the meninges, which consists of the membrane that envelops and protects the central nervous system. N. meningitidis is also commonly known as meningococcus and is carried by approximately 8-25% of the general population in the normal mucosa of the nasopharynx and upper respiratory tract. The varying compositions of the polysaccharide capsule on different strains of N. meningitidis allow the species to be divided into several serogroups, with serogroups A, B, and C as the prominent strains responsible for outbreaks of meningitis in both developed and undeveloped countries. The infection is transmitted to individuals through contact with respiratory secretions or saliva from sneezing, coughing, and talking. Symptoms of the disease are sudden onset and include fever, neck stiffness, and severe headache. Early diagnosis and immediate treatment are vital to the survival of patients assumed to be ill with meningococcal meningitis. Treatment for infected individuals involves the administration of antibiotics such as penicillin G to rid the pathogen and prevent its colonization.[1] [2]
Pathogenesis
Transmission
Meningococci have been categorized into 13 serogroups: A, B, C, D, 29E, H, I, K, L, W-135, X,Y, and Z. Of the 13 serogroups, A, B, C, W-135, and Y remain encapsulated, causing more than 90% of the invasive disease across the world. [3] N. meningitidis commonly colonizes in the nasopharynx. As a result, droplets or discharge from the nose or throat that contain N. meningitidis can be transferred to other individuals, resulting in successful transmission of the species. Direct contact with the respiratory droplets can occur through coughing, sneezing, and kissing. Transmission also occurs at higher frequencies in environments where crowding is common, such as prisons, dormitories, and military installations. [4]
Infectious dose, incubation, and colonization
The infectious dose of N. meningitidis is unknown, but the transmission of bacteria is highly contagious. On average, the incubation period is 2-4 days but can range from approximately 2-10 days, while invasive meningococcal infections occur within 14 days of acquiring the bacteria. [5] Individuals with N. meningitidis infections are most contagious during the period of 3 days preceding initial symptom presentation and continue to remain infectious while meningococci persists in nasalpharynx discharge. [6] Humans serve as the sole natural reservoir for N. meningitidis, and 10% to 35% of adults and adolescents are asymptomatic carriers, with the majority of bacteria carried as nonpathogenic strains. [7] [8] Carriers of meningococci have the bacteria as a commensal microorganism residing in the respiratory tract and nasopharynx mucosa. It is the penetration of these colonized bacteria into the mucosal membrane and subsequently into the bloodstream that results in various forms of illness. [3]
Epidemiology

While N. meningitidis is found worldwide, the region of highest incidence is located in sub-Saharan Africa. Referred to as the “meningitis belt”, the frequency of meningococcal disease in this area is several times higher than that of the United States. During the dry season (December-June), the outbreak of sporadic epidemics transpires with as many as 1,000 cases per 100,000 population. Nonepidemic periods have lower rates of occurrence, with approximately 5-10 cases for every 100,000 inhabitants in the region. The outbreaks in the African meningitis belt are usually a result of the serotype A group of N. meningitidis, although minor cases are at times due to serogroups C, X, and W-135. Individuals travelling to areas located within sub-Saharan Africa are at significant risk of contracting disease after extended contact with local inhabitants during the course of an epidemic. [9]
Outbreaks of meningococcal disease are predominately found in the meningitis belt, but they also appear in the Unitd States. 90% of meningococcal diseases in the United States are a result of serogroups B and C. The average annual rate of invasive diseases caused by N. meningitidis is estimated to be 1.1 cases per 100,000 people or 2,600 cases annually. [4] Those most at risk for meningococcal disease are toddlers, with rates of incidence estimated to be 46% in children younger than 2 years. Approximately 25% of infections occur in patients older than 30 years. [4]
Morbidity and Mortality
The mortality rates of illness caused by N. meningitidis differs depending on the region, country, and age group. [9] Typically, 5% to 10% of patients with meningococcal meningitis die, usually within a period of 24 to 48 hours of initial symptom presentation, despite prompt diagnosis and antibiotic therapy. Without treatment, individuals afflicted with meningitis have a 50% mortality rate. Among the patients that recover from invasive meningococcal diseases, approximately 10% to 20% have permanent sequelae including hearing loss, neurologic damage, or learning disabilities. [10] Other complications that occur infrequently include blindness, seizures, myocarditis, pericarditis, ataxia, pneumonia, conjunctivitis, and chronic meningococcemia. [4]
Virulence Factors
N. meningitidis utilize a variety of virulence factors to facilitate survival and proliferation in the host reservoir.
Capsules
The absence or presence of encapsulated N. meningitidis is highly dependent on the origin of sample. When isolated from carriers, the bacteria may be either capsulate or acapsulate, while samples isolated from cerebrospinal fluid or the bloodstream are consistently capsulate. The presence of capsules in pathogenic N. meningitidis serve to provide resistance against antibody, complement-mediated, or phagocytic destruction by the host immune response. Serogroups B, C, W-135, and Y incorporate sialic acids into the capsule, allowing for evasion by the immune response as sialic acids are also commonly found on several host cell surfaces. A phenomenon identified as capsule switching occurs between the aforementioned serogroups, a process which allows for horizontal exchange of the capsule operon, thereby resulting in anti-capsular antibodies to prove ineffective in eliminating the pathogen. [8]
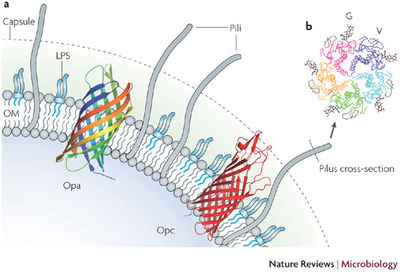
LPS
Endotoxin is a cardinal virulence factor in N. meningitidis, inducing septic shock in patients by triggering pro-inflammatory mediator production. However, the LPS in this species are referred to as lipooligosaccharides (LOS) due to the lack of repeating O-antigens in the polysaccharide structure. Is it the oligosaccharides that contribute to the 12 differing immunotypes of N. meningitidis which are also subject to phase variation via frameshift mutations, allowing the pathogen to circumvent the host immune response. [3]
Adhesion
Several structural and molecular features allow bacteria to adhere to the mucosal surfaces for colonization. N. meningitidis use filaments known as type IV pili located on its surface to adhere to the CD46 membrane coreceptors of host cells. [3] Pili of the Neisseria genus are approximately 6 nm in diameter. In addition to pili, N. meningitidis also express Opa and Opc, two types of proteins found on the outer membrane of the bacteria. Through genetic discrepancy, Opa proteins frequently undergo antigenic variation. Host cells such as epithelial and endothelial cells express a family of receptors known as CEACAM (carcinioembryonic antigen-related cell-adhesion molecule) that bind to Opa proteins during adhesion, while Opc proteins bind to other specific receptors on host endothelial cells. Both types of proteins mediate adhesion and invasion of host cells to facilitate the spread of the pathogen. [8] In addition to Opa and Opc proteins, N. meningitidis strains also express and secrete many other proteins that bind to human cells. Amongst these proteins are lactoferrin- and transferrin-binding proteins that also assist the bacteria in binding iron, a fundamental growth factor for colonization and the spread of disease. [8]
Clinical features
Symptoms of meningitis can develop very quickly and require prompt medical attention to increase the probability of recovery. [11] Characteristics of meningitis include acute onset of fever, severe headache, weakness, hypotension, and rash. In addition, these symptoms are often accompanied by stiff neck, photophobia, and altered mental status. For infants and toddlers, often the only characteristics of illness that present are fever and vomiting. [6] Up to 75% of patients with meningitis present with N. meningitidis in the bloodstream.
In cases where infection by N. meningitidis does not result in meningitis, other symptoms of illness can occur. Meningococcal sepsis, or meningococcemia, is an infection of the bloodstream and occurs with 5% to 20% of invasive meningococcal infections. In this case, symptoms are more severe than those of meningitis and include shock, acute adrenal hemorrhage, and organ failure occur. Additionally, progression of the disease is indicated as a purple petechial or purpuric rash that is characteristic of meningococcemia.[7]
Diagnosis
Diagnosis of meningitis cases can be allocated into three separate categories: confirmed, presumptive, and probable. Laboratory diagnosis of confirmed invasive meningococcal diseases is completed by isolation of the bacteria from normally sterile sites of the body, including the bloodstream and cerebrospinal fluid. Lumbar punctures are typically performed in order to extract the sample required for testing. [4] Gram-stains of samples drawn from cerebrospinal fluid that demonstrate the presence of gram-negative diplococci are thus classified as presumptive cases. The identification of probable cases includes the absence of a positive culture of N. meningitidis from sterile sites of the body but the presence of antigen and symptoms consistent with the disease. Additional modes of serologic testing can be used to evaluate the possibility of meningococcal disease but are not administered to confirm a definitive diagnosis. Serological tests involve determining the presence of antibodies to the polysaccharide capsule of N. meningitidis. Urine or serum tests for antigen are not used to diagnosis meningitis, as they are unreliable. [7]
Treatment
Due to the severity of illness, any individual suspected of infection by N. meningitidis should be admitted to a hospital immediately. Prompt treatment of infected patients is crucial for the survival of the individual. Antibiotic therapy is the treatment of choice for invasive disease. The primary line of antibiotics is penicillin G, typically administered intravenously at 250,000 IU per dose for every 4 to 6 hours. [4] Other effective antibiotic alternatives can be administered, including ampicillin, ceftriaxone, and cefotaxime. Antibiotic therapy is continued for a period of five to seven days to effectively eliminate the infection. To ensure eradication of N. meningitidis and to prevent its colonization in the nasopharynx, additional antibiotics are administered for chemoprophylaxis prior to hospital discharge. [6]
Prevention
Vaccination
There are two available meningococcal vaccines available in the United States: Meningococcal Polysaccharide Vaccine (MPSV4) and Meningococcal Conjugate Vaccine (MCV4). First licensed in 1974, MPSV4 consists of 50 mcg of purified capsular polysaccharides from the four serogroups A, C, Y, and W-135. In addition, the vaccine also contains lactose for stabilization properties. MPSV4 is utilized with single-dose and 10-dose vials which are administered through subcutaneous injection. This type of vaccine is typically ineffective for children under 18 months of age but for children older than this age, the amount of antibody necessary for protection is usually produced within 7 to 10 days of vaccination. Licensed in 2005, MCV4 is a more recent vaccine that conjugates the same capsular polysaccharide antigens from MPSV4 to the diphtheria toxoid protein, allowing the body to respond to the presented antigens more quickly and efficiently. [12] A combination of 4 mcg of capsular polysaccharide antigen with 48 mcg of diphtheria toxoid protein carrier constitutes every 0.5-mL dose of MCV4. Types of MCV4 are administered via intramuscular injection for persons 9 months to 55 years of age. In the United States, there are no vaccines available for serogroup B. [7]
Prophylaxis
In cases where exposure to N. meningitidis may have occurred, chemoprophylaxis is recommended to prevent those individuals from contracting the illness. This type of preventative treatment is administered circumstantially only to individuals who have had direct contact with the infected patient, such as household members, and not to individuals with only brief contact with the index case. Chemoprophylaxis should begin immediately upon exposure, as the effects of this treatment become significantly diminished as the duration of time lengthens since initial contact. The primary drug of choice for chemoprophylaxis is rifampin, with dosages tailored to individuals based on age. Its effectivity in eradication of N. meningitidis is approximately 90%. Other alternatives for prophylaxis are ceftriaxone, ciprofloxacin, and the least preferable option, azithromycin. [6]
Host Immune Response
The mechanism of action of the host immune response to N. meningitidis is not fully understood, but further research is being continued to study this interaction. What is known is that the bacteria subvert the immune response by producing outer membrane vesicles (OMV). In addition, the pathogen is able to escape complement system of the innate immune response with its capsular structure and molecular mimicry of outer host cell structures. During cytokine production by phagocytes in the body, proinflammatory responses are activated which allows N. meningitidis easier access through the endothelial barrier. [13]
One area of research currently being conducted analyzes the relationship between N. meningitidis and host neutrophils. Pathogenic N. meningitidis induce a host innate immune response, prompting a high, lethal influx of neutrophils to the site of infection. The overwhelming amount of neutrophil activity damages infected tissues, allowing the bacteria to subvert the tissue barrier and gain access to secondary anatomical areas. The recruitment of neutrophils becomes potent as the areas that N. meningitidis infects typically have an absence of neutrophil activity. It is the abundance of neutrophil activity that marks the major clinical demonstration of illness. Upon infiltration past the tissue, N. meningitidis can travel to the meninges, skin, and bloodstream, causing septic shock and disseminated intravascular coagulation. [14]
References
1 Center for Disease Control (CDC) General Information on Neisseria meningitidis
2 Bioquell General Information on Neisseria meningitidis
3 Yazdankhah SP, Caugant DA. “Neisseria meningitidis: an overview of the carriage state.” Journal of Medical Microbiology, doi: 10.1099/jmm.0.45529-0
4 Ferguson LE, Hormann MD, Parks DK, Yetman RJ. Neisseria meningitidis: Presentation, Treatment, and Prevention. Journal of Pediatric Health Care 16 (3). 2003.
5 Pathogen safety data sheet of Neisseria meningitidis
6 Oregon Public Health report on Meningococcal Disease
7 Center for Disease Control (CDC) Vaccine Information for Meningococcal Disease
8 Hill DJ, Griffiths NJ, Borodina E, Virji M. “Cellular and molecular biology of Neisseria meningitidis colonization and invasive disease.” US National Library of Medicine. 2010 Feb 9;118(9):547-64. doi: 10.1042/CS20090513.
9 Center for Disease Control (CDC): Bacterial Meningitis Manual
10 World Health Organization (WHO): Global Health Observatory
11 Mayo Clinic General Information on Meningococcal Diseases
12 WebMD: Children’s Vaccines
13 Gasparini R, Amicizia D, Lai PL, Panatto D. “Neisseria meningitidis: pathogenic mechanisms to overcome the human immune defences”. Journal of Preventive Medicine and Hygiene 2012; 53:50-55.
14 Criss AK, Seifert HS. “A bacterial siren song: intimate interactions between Neisseria and neutrophils.” 2012 Jan 31;10(3):178-90. doi: 10.1038/nrmicro2713.
Created by Christina Cheng, student of Tyrrell Conway at the University of Oklahoma.

