Practice Template - Eva Illuzzi
Classification
Taxa Kingdom: Bacteria, Phylum: Bacteroidetes, Class: Bacteroidia, Order: Bacteroidales, Family: Bacteroidaceae, Genus: Bacteroides
Species Bacteroides fragilis (B. fragilis)

Introduction
Bacteroides fragilis is a gram-negative, non-spore forming, rod-like anaerobic microbe.[1] The bacteria reside in the gut flora of the human microbiota. Bacteroides fragilis remain commensal with the host when in the gut. There, they play an essential role in processing complex molecules into simpler ones in the host intestines. However, if the microbe enters the bloodstream or surrounding tissue it can lead to severe anaerobic infections, most commonly the formation of abscesses.
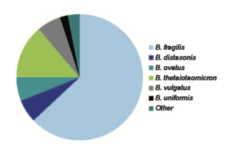
Anaerobes are the most common bacteria in the human colon. Within the group of anaerobes, Bacteroides make up approximately 25% of the anaerobic bacteria within the gut.[2] The Bacteroides genus consists of: B. fragilis, B. distasonis, B. ovatus, B. thetaiotaomicron, B. v ulgatus, B. uniformis, B. eggerthii, B. merdae, B. stercoris,and B. caccae (shown in Figure 2). Of these Bacteroides, B. fragilis is the most frequent isolate and responsible for the majority of the anaerobic infections.[1] B. fragilis is most commonly associated with intra-abdominal infections. A number of these species demonstrate resistance to a wide variety of the current antibiotics.
Pathogenesis and Epidemiology
B. fragilis is often considered the single most important pathogen among the anaerobes that exist in the normal flora. Infections from B. fragilis commonly arise from a break in the mucosal membrane of the intestine.[3] The travel of B. fragilis outside of the gut can lead to a variety of infections such as local abscesses at the site of the break, metastatic abscesses by spread through the bloodstream to distant organs, or lung abscesses by inhalation of the bacteria.
Bacteroides species can be passed from a mother to offspring during childbirth, integrating itself into the human flora.[4] Species of Bacteroides, including B. fragilis, appear in the newborn microbiota about 10 days after birth.[5] Predisposition to B. fragilis infection can arise from surgery, disease, or trauma which can cause a rupture of the gastrointestinal tract leading to pathogenesis.
E. coli, a facultative anaerobe, uses the oxygen at the site which brings the oxygen to a level where anaerobes, such as B. fragilis, can thrive and grow. Due to this phenomenon, many severe anaerobic infections contain a mix of anaerobic and aerobic flora.

Virulence
Adherence to Tissues: The fimbriae of B. fragilis allows for easy adhesion to epithelial cells and extracellular molecules. B. fragilis can also adhere to peritoneal surfaces due to its unique polysaccharide capsules, a structural function that not many other anaerobes possess. These adhesive properties permit B. fragilis to establish itself within the host tissue and avoid immune targeting and attack.[1]
Protection from Host: The ability of a bacterium to protect itself from the immune response of its host is a large contributing factor to the species' virulence. Due to its polysaccharide capsule, a key promoter in the formation of intraabdominal abscesses, its LPS (Lipopolysaccharide), the main component of the outer membrane of gram-negative bacteria, and a variety of protective enzymes B. fragilis is able to defend itself from the immune response of the host.[1][6]
Destruction of Tissues: Histolytic enzymes of B. fragilis control and induce tissue destruction. This destruction of the host is one of the main reasons why B. fragilis is considered so virulent and dangerous. As the abscesses form, the B. fragilis also can eliminate surrounding tissue often leading to permanent damage. Abscesses that remain untreated for prolonged periods of time can expand to severe levels and even lead to intestinal obstruction or damage of the surrounding blood vessels.[1]
Treatment and Prevention
B. fragilis has inherent resistance to penicillin due to its production of β-lactamase.[1] Bacteroides are also exposed to many antibiotics over the course of their lifetime as antibiotics first pass through the digestive tract. This constant exposure combined with its inherent resistance to penicillin leads to Bacteroides being one of the most antibiotic resistant microbes among anaerobic bacteria.
Antibiotics such as clinimycin, metronidazole, carbapenem, beta-lactam/beta-lactamase inhibitor combinations (e.g. ampicillin/sulbactam, piperacillin/tazobactam), and cephamycins (cefoxitin, cefotetan, cefmetazole), are some of the only treatments found to eliminate a Bacteroides fragilis infection.[7][8] However, resistance rates to cefoxitin and clindamycin are on the rise.[9] After severe infections, the abcesses commonly need to be drained and the patient should continue treatment with antibiotics. Abcesses in the lungs can usually heal without intravenous treatment.
Preventative measures of B. fragilis infections includes administration of antibiotics prior to abdominal or pelvic surgery.[1]
Bacteroides infection can also be prevented by initial treatment with gentamicin, an antibiotic which targets facultative anaerobes such as E. coli but not Bacteroides.6 Because Bacteroides fragilis infection depends also on the existence of a facultative anaerobe, this antibiotic can be another preventative measure taken to prevent severe anaerobic infections involving B. fragilis. This method, however, does not stop the later development of Bacteroides abscesses. Therefore a more effective treatment combines both gentamicin with clindamycin, an antibiotic that is effective against Bacteroides, prevents the initial infection and later development of abdominal abscesses.[1]
Research
Research into B. fragilis is especially relevant today as it continues to increasingly become resistant to more and more antibiotics. A large majority of the B. fragilis research is currently being conducted on the the polysaccharide capsule and how this structure contributes to the virulence and abcess formation within the host.[10]
Bacteroides are common alternatives in fecal indicator organism as they make up a large amount of the normal fecal bacterial flora. Bacteroides have a high degree of host specificity and typically have a low growth potential making them optimal indicators. Due to their sheer numbers, there is a greater likelihood of isolating Bacteroides over other traditional fecal indicators, such as E. coli. As fecal indicator organisms, B. fragilis, especially, can be useful for identifying situations of poor sanitation and risk of potential infections from pathogenic microorganisms.[11] The use of Bacteroides as a fecal indicator can determine the potential presence of dangerous bacteria following a flood or sewage contamination in a building as well as identifying fecal contamination in recreational waters. Testing for Bacteroides is often done using PCR analysis.
Conclusion
B. fragilis is one of the most significant human anaerobic pathogens. It is the most commonly isolated bacteria from anaerobic infections but also exists commensally within the human intestines. The anaerobe only presents danger when it escapes the gastrointestinal tract due to a rupture. After escaping, the anaerobic infection can be very severe due to the high virulence and pathogenicity of B. fragilis. The pathogen can produce large abscesses outside the intestinal tract or even travel through the blood to infect a distant organ such as the abdomen, brain, liver, pelvis, or lungs. This specific species of Bacteroides is still being studied today due to its prominence within the body, its increasing antibiotic resistance, its important use in fecal tracing, and its unique structural and physical functions that other species of the Bacteroides genus do not contain. Continued understanding of the B. fragilis species can lead to a deeper understanding of the human microbiota and anaerobic infections.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Wexler HM. Bacteroides: the good, the bad, and the nitty-gritty. Clin Microbiol Rev. 2007 Oct;20(4):593-621.
- ↑ Salyers, A. A. 1984. Bacteroides of the human lower intestinal tract. Annu. Rev. Microbial. 38:293-313.
- ↑ Elsaghir H, Reddivari AKR. Bacteroides Fragilis. [Updated 2020 Jun 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-.
- ↑ Reid G. 2004. When microbe meets human. Clin. Infect. Dis.39:827-830.
- ↑ Simon, G. L., and S. L. Gorbach. 1984. Intestinal flora in health and disease. Gastroenterology 86:174-193.
- ↑ Mancuso, Giuseppe et al. Bacteroides fragilis-derived lipopolysaccharide produces cell activation and lethal toxicity via toll-like receptor 4. Infection and immunity vol. 73,9 (2005): 5620-7.
- ↑ Mandell GL, Bennett JE, Dolin R (2004). Principles and Practice of Infectious Diseases (6th ed.). Churchill Livingstone.
- ↑ Brook I (December 2007). Treatment of anaerobic infection. Expert Rev Anti Infect Ther. 5 (6): 991–1006.
- ↑ Bartlett JG, Fabre V. Bacteroides Fragilis. In: Johns Hopkins ABX Guide. Johns Hopkins University; 2019.
- ↑ Tzianabos AO, Kasper DL, Onderdonk AB. Structure and function of Bacteroides fragilis capsular polysaccharides: relationship to induction and prevention of abscesses. Clin Infect Dis. 1995 Jun;20 Suppl 2:S132-40.
- ↑ Fiksdal L, Maki JS, LaCroix SJ, Staley JT. Survival and detection of Bacteroides spp., prospective indicator bacteria. Appl Environ Microbiol. 1985 Jan;49(1):148-50.
Edited by Eva Illuzzi, student of Joan Slonczewski for BIOL 116 Information in Living Systems, 2020, Kenyon College.
