The Return of Listeria
Introduction
By Chris Chu
Picture this: It's a scorching summer day, and you're standing in line at your favorite ice cream shop, torn between flavors and toppings. However, what if the seemingly innocent act of choosing your treat was overshadowed by a silent threat?
Enter
Listeria monocytogenes, a bacterium lurking in that beloved cold dessert.
Listeria monocytogenes, infamous for causing listeriosis, is not limited to ice cream—it can be found in an array of foods, including raw vegetables, meat, and dairy products. While most healthy individuals may experience only mild flu-like symptoms from consuming contaminated food, certain demographics face grave risks.Groups such as the elderly, pregnant women, newborns, and individuals with compromised immune systems are particularly susceptible to severe illness from Listeria monocytogenes. For them, listeriosis can escalate into dangerous conditions like meningitis, posing significant health threats. Symptoms of listeriosis vary but can include fever, muscle aches, nausea, and diarrhea. In severe cases, the infection can progress to affect the nervous system, leading to symptoms such as headache, stiff neck, confusion, and convulsions. Swift diagnosis and treatment, often involving antibiotics, are crucial, especially for high-risk individuals.To combatListeria monocytogenes contamination, stringent food handling and hygiene practices are imperative. From thorough cooking of raw foods to meticulous washing of produce, proper precautions can significantly reduce the risk of infection.The prevalence of Listeria monocytogenes in the food supply chain can be influenced by environmental conditions and human activities. Understanding these factors is essential for implementing effective prevention strategies and mitigating risks to public health.Delving into the gene expression of Listeria monocytogenes provides valuable insights into its virulence and antibiotic resistance mechanisms. By deciphering its genetic makeup, researchers can better understand how this pathogen interacts with the human body and the environment, aiding in the development of targeted interventions.
Overview
History
The discovery of Listeria monocytogenes is dated in 1924 where three bacteriologists isolated L. monocytogenes as etiological agents (microorganisms that cause diseases in humans[1]) by injecting rodents in an experiment. One of the microbiologists, E.G.D Murray, isolated the gram-positive rods from the blood of a rodent; however, could not identify the pathogenic microorganism to any genus known resulting in calling it Bacterium monocytogenes[2]. The first recorded case of Listeria monocytogenes in humans dates all the way back to Denmark in 1929. However, the first ever culture of L. monocytogenes was isolated in France from a patient with meningitis[3]. After twenty years of listeriosis discovery, the bacteria was found mostly among livestock, and mostly in small rodents.[4]. Very few cases were found in humans making it very rare and uncommon. This resulted in little to no mention in famous textbooks on bacteriology. It wasn’t until the late 40s that Dr. Stanley extracted monocytosis producing agents from living rabbit cells and described them as lipids[5]. His discovery helped broaden the understanding of how monocytes are distributed throughout the body and contribute to their development in the immune system.
Structure
L. monocytogenes is a firmicute, which is part of a phylum of bacteria called Bacillota. It is a gram positive bacteria, however it could also be gram negative depending on the age of the culture[6].. The shape of these organisms are rod-like and do not form spores. There is no outer membrane, however, it has a S-layer which is a thick cell wall with layers of peptidoglycan. L. monocytogenes has a cell wall around 200 Å in thickness[7]. L. monocytogenes can thrive in refrigerator temperatures and have an enzyme called RNA helicase which improves activity and replication at low temperatures. This enzyme boosts their ability to survive in harsh climates. This bacteria also has a flagella, which is used to propel itself and attach it to enterocytes during infection[6]. Enterocytes, found in both the small and large intestines, are predominant epithelial cell lineage which has membranes with tight junctions that form between cells to create a physical barrier for mycobacteria[8]. L. monocytogenes have 4 primary virulence factors that help it infect host cells. It possesses internalins (Inl A and InlB) which are cell-surface galactose residues, lipoteichoic acids, and surface proteins that help L. monocytogenes attach to gastrointestinal epithelial cells using host protein cadherin[9]. This allows them to enter the cell and infect it. After the bacteria has invaded the host cells, it uses listeriolysin (LLO)[10]. Listeriolysin are proteins that form cytotoxic pores on the cell’s vacuole to allow L. monocytogenes to derange cellular processes by going through the cell membrane. Phosphatidylinositol-specific phospholipase C (PI-PLC) aids in the bacteria's evasion from the host cell vacuole and induces membrane disruption[6]. Lastly it also uses actin polymerization (ActA) to help in move between cells after infection[11].
Symptoms and Treatments
Treatments
Listeria monocytogenes is a worldwide foodborne illness that has a hospitalization and mortality rate. Luckily, the annual cases of Listeria have been declining. 7.7 million per one million cases to 3.1 during the period from 1990 to 2023 in the USA and in Europe the infection rate declined from 4.5 cases per million to 3.4 cases from 1999 to 2003[12]. Annually, there are about 1600 cases of Listeria infections that are reported in the USA[13]. The mortality rate is about 30% while the hospitalization rate is about 99.1%[14]. The Center for Disease Control and Prevention (CDD) estimates that Listeria is the third leading cause of death from food poisoning int the USA[15]. Anyone can have a Listeria infection, however, the ones with the greatest chance of an infection are: people who are pregnant, people who are 65 years and older, and people with a weakened immune system. Pregnant women are 10 times more likely to have listeriosis which can result in miscarriages, stillbirths, preterm labor, and serious illness to the newborn[16]. The new born could have symptoms of dever, vomiting, little to no interest in feeding, irritability and difficulty breathing[17]. More than half of all infections occurred to people 65 and older[18]. As people age, stomach acid becomes weaker and not able to kill the bacteria, as a result makes people older than 65 four more times to get a Listeria infection[19].
Symptoms
Symptoms of listeriosis include fever, muscle aches, nausea, vomiting, and diarrhea[20]. More severe symptoms are headaches, stiff neck, loss of balance, convulsions, and death[21]. Patients who are not pregnant most often are diagnosed with bacteremia, meningitis, and meningoencephalitis[22]. Listeriosis is most common during third trimester, however it can occur at any time during pregnancy[23]. Neonatal listeriosis may also occur. This occurs in the first 7 days of life, results from bacteremia or sepsis[24]. These symptoms can last from a few days to several weeks. Michigan State said that Listeriacan be even more dangerous and have long term effects. It can compromise the immune system and cause sepsis and meningitis[25]. Meningitis is the infection and inflammation of the fluid and membranes in the brain and spinal cord which results in headaches, fever, and stiff neck[26]. Sepsis is when the body doesn’t respond well to an infection. This leads to organs not working well. Sepsis will lead to septic shock where there are dramatic drops in blood pressure which results in damaging organs such as lungs, kidneys, liver and more[27].
Prevention
There are many ways to prevent the risk of having a Listeria infection. If there are foods that have been contaminated in the fridge, decreasing the temperature will slow down the rate of growth. Everything that has been contaminated should be washed. After they have been washed, they should be sanitized with one tablespoon of chlorine bleach to one gallon of hot water, and then properly dried[28].
Case Study
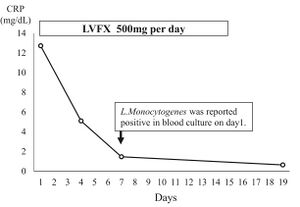
Beta-lactam antibiotics, like penicillin, ampicillin, amoxicillin, and gentamicin, exhibit bactericidal properties and are advised for listeriosis treatment[29]. However, in 2023, a study was conducted to treat L. monocytogenes with an oral levofloxacin in an immunocompromised patient[30]. Levofloxacin is part of the quinolone antibiotic class which treats a variety of bacterial infections by stopping the growth of bacteria[31]. In the case study, the patient was a 72 year old woman, her symptoms were a fever (39◦ C), watery diarrhea (since 5 days), and malaise[32]. They believe the cause of this was from sausage since that was the last thing she ate prior to the fever, however, it is unclear since there wasn't enough detailed information. She has a history of rheumatoid arthritis, controlled with prednisolone (5mg/day) and methotrexate (16mg/week)[33]. Blood tests showed elevated levels of C-reactive proteins ( proteins made by the liver which increase production during inflammation in the body[34]) and increased white blood cell count[35]. Liver enzymes, kidney function and coagulation factors were within normal limits, which led them to suspect it was a bacterial infection which initiated an antimicrobial treatment with oral levofloxacin[36]. The patient’s fever was resolved after the third day of the oral levofloxacin treatment[37]. The seventh day was when they diagnosed L. monocytogenes bacterium in a positive blood culture[38]. Combination therapy, adding gentamicin (part of the aminoglycoside antibiotic glass which kills bacteria and stops it from growing[39]) to ampicillin (part of penicillin class and works by killing bacteria[40]
) was believed to be most effective against the bacterium in vitro, however, it was against intracellular bacteria[41]. Levofloxacin and other fluoroquinolones have shown some promise to help treat L. monocytogenes by penetrating intracellularly and being concentrated in the cytoplasm of the host cell[42].
Outbreaks
There have been many outbreaks of Listeriosis in the United States. Part of the Centers for Disease Control and Prevention is to identify which foods have a high chance of being infected. Their job was Identifying the potential food source behind the outbreak. CDC and the United States Food and Drug Administration teamed up and investigated, which included interviewing the patients on the kind of food they consumed before falling sick[43]. The CDC identified an ice cream production facility and its warehouse in Brooklyn, NY as the suspected origin of the outbreak. Subsequent analysis confirmed this suspicion by isolating the Listeria strain responsible for the outbreak from the "Soft Serve On The Go" vanilla chocolate cup ice cream, which was consumed by large number affected individuals. The NY State Department of Agriculture and Markets also detected the Listeria strain in samples taken from the ice cream cups at the manufacturing facility[44].
Another company that was linked to Listeria was Rizo-Lópex Foods on February 6, 2024[45]. The items were queso fresco and cotija cheese which made people sick in this outbreak. Many foods including cheeses, crema, and yogurts were recalled aswell.There were a total of 26 reports, and out of the 23, only 3 were not hospitalized and 2 died. In the past decade 524 total listeriosis cases were reported and resulted in 80 deaths[46]. Once again, since its ability to thrive at low temperatures helps it excel in global outbreaks.
Most common foods that are frozen[47]. However, Listeria outbreaks can be linked to leafy greens[48]. Since June 13, 2023, 19 were diagnosed with Listeria and 18 were hospitalized, however, there were no deaths. Out of the 14 individuals surveyed regarding their consumption of leafy greens, 13 (93%) reported having consumed them. Analysis revealed that those affected by the outbreak were eight times more likely to have consumed iceberg lettuce and five times more likely to have eaten romaine lettuce before falling ill compared to individuals who contracted Listeria but were not linked to any outbreak. Leafy greens and various brands of packaged salads were purchased by individuals from multiple stores[49].
On the CDC website, they present safer options to choose from and have a less likely chance of contracting Listeria. Instead of eating unpasteurized soft cheese (queso fresco or brie) and sliced cheeses that may be unheated at a deli, you should look for hard cheeses (cheddar or parmesan), cottage cheeses, cream cheese, string, mozzarella, and any cheese that has been pasteurized at 165 degrees fahrenheit[50]. Deli meats or any fermented or dry sausages that have not been heated to 165 degrees fahrenheit, are also a higher risk of getting listeriosis[51]. In 2022, there was a listeria outbreak related to deli meat and cheeses. Out of the 16 that were reported, 13 were hospitalized and 1 died[52]. The bacteria could have come deli slicers[53].Pre-made salads have a high risk as well;making homemade salads would be much safer. Smoked fish is another common carrier of listeria, as long as it is packaged and sealed correctly, the chances are much lower. Melons that have been cut and left out for more than 2 hours or been exposed to higher temperatures of 90 degrees fahrenheit are not safe[54]. In October 2011, there was an outbreak related to Jensen Farms Cantaloupes[55]. There were 147 reported cases which resulted in 33 deaths and 143 hospitalizations[56].
Variants
Listeria outbreaks extend beyond the United States, with documented occurrences of unclear origin in South Africa, Australia, and Europe. This article conducts a thorough examination of compiled literature on various reported Listeria outbreaks, exploring their connections to potential food sources. Researchers have been beginning to look at other variants of Listeria and recommendations aimed at preventing future outbreaks, thus contributing to improved public healthcare and human well-being.
The genus Listeria comprises 17 recognized species (including Listeria monocytogenes, Listeria seeligeri, Listeria ivanovii, Listeria welshimeri, Listeria marthii, Listeria innocua, Listeria grayi, Listeria fleischmannii, Listeria floridensis, Listeria aquatica, Listeria newyorkensis, Listeria cornellensis, Listeria rocourtiae, Listeria weihenstephanensis, Listeria grandensis, Listeria riparia, and Listeria booriae), all of which are all small rod-shaped gram-positive bacteria. Among these, only two species, L. monocytogenes and L. ivanovii, are recognized as pathogens[57]. There are two groups the species in genus are categorized into (1) Listeria sensu strictu, which includes L. monocytogenes, L. seeligeri, L. marthii, L. ivanovii, L. welshimeri, and L. innocua[58], and (2) Listeria sensu lato, which included the rest of the species[59]. Each different species of genus is separated based on relatedness to L. monocytogenes and economic and public health impact[60]. Species in Listeria sensu strictu share specific phenotypes characteristics which allow them to grow at temperatures as low as 4°C, motility, the ability to catalyze reactions, and the inability to reduce nitrate to nitrite. Also, these species will test positive in the Voges-Proskauer; the ability to produce acetoin from fermentation of glucose[61]. Some of the species within Listeria sensu strictu, show hemolytic activity, produces hemolysins that damage the membrane of red blood cells which is called hemolysis[62]. L. ivanovii is unique to Listeria monocytogenes since it is the only one that can ferment Dribose, Similar to Listeria sensu strictu, Listeria sensu lato also has a similar phenotype. Only two out of the sensu lato species, have the ability to produce acetoin from fermentation of glucose[63]. Unlike its counter part, all of the genus in Listeria sensu lato have the ability to reduce nitrate to nitrite[64]. There have been late studies that have said there is motility in Listeria sensu lato strains, however, more recent studies have shown no signs of motile[65]. All species were seen to acidify D-xylose and D-glucose[66].
Future
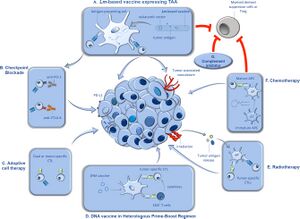
Researchers have begun to use Listeria-based vaccines in tumor immunotherapy to help patients[67].Various strategies have been employed to enhance the immune system's ability to combat tumors, ranging from the delivery of isolated immune system elements to the utilization of microorganisms[68]. These approaches have surfaced as valuable assets in the battle against cancer. The development of a listeria-based vaccine is helpful since Listeria monocytogenes have the ability to active and deliver tumor antigens selectively to antigen-presenting cells[69]. The Lm vaccines infect the antigen presenting cells in the lymph nodes and release tumor antigens, which are called cytotoxic T lymphocytes (CTL)[70]. Sometimes the CTL will then clock certain molecules on the cells[71]. Cells that target both tumors and Lm-derived antigens alongside Lm vaccines, given directly into the tumor, can broaden the response of the immune system against the cancer[72]. Using Lm vaccines along with other types of vaccines in a specific order can boost the immune response even more[73]. Radiation therapy can help Lm vaccines by killing tumor cells and releasing more tumor antigens, which then help activate the immune system[74]. Some chemotherapy drugs, like cyclophosphamide, can also make Lm vaccines more effective by improving the function of certain immune cells and reducing the number of cells that suppress the immune system in the tumor[75]. Blocking a certain signaling pathway can also improve the effectiveness of Lm vaccines by stopping certain cells from entering the tumor and suppressing the immune system there[76].
Conclusion
In a world filled with seemingly innocent pleasures, the threat of Listeria monocytogenes lurks, casting a shadow over the enjoyment of everyday foods. Listeria monocytogenes, notorious for causing listeriosis, extends its reach far beyond the realm of ice cream, infiltrating various foods such as raw vegetables, meat, and dairy products. While many may only experience mild flu-like symptoms upon consumption of contaminated food, vulnerable demographics face graver risks. The elderly, pregnant women, newborns, and those with weakened immune systems stand particularly susceptible, with listeriosis potentially escalating into life-threatening conditions like meningitis. Symptoms of listeriosis vary, ranging from fever and muscle aches to more severe manifestations such as headaches and convulsions. Swift diagnosis and treatment, often involving antibiotics, are imperative, especially for those at higher risk. To combat Listeria monocytogenes contamination, stringent food handling and hygiene practices are paramount. From thorough cooking of raw foods to meticulous washing of produce, these precautions significantly mitigate the risk of infection.Understanding the environmental factors and human activities that influence the prevalence of Listeria monocytogenes in the food supply chain is crucial for implementing effective prevention strategies. Delving into the bacterium's gene expression offers valuable insights into its virulence and antibiotic resistance mechanisms, aiding in the development of targeted interventions.On a global scale, Listeria monocytogenes remains a significant concern for public health. While annual cases may be declining, the mortality and hospitalization rates underscore the severity of this foodborne illness. Case studies offer valuable insights into the treatment of listeriosis, highlighting the efficacy of antibiotics such as levofloxacin in combating the bacterium. However, challenges remain, particularly in addressing antibiotic resistance and intracellular infections.The genus Listeria comprises various species, with only Listeria monocytogenes and Listeria ivanovii recognized as pathogens. Understanding the phenotypic characteristics and genetic makeup of these species aids in their identification and management.Outbreak investigations, such as those conducted by the Centers for Disease Control and Prevention, play a crucial role in identifying potential food sources and implementing necessary recalls.The CDC has helped by also classifying leafy greens, deli meats, and pre-made salads have all been implicated in outbreaks, underscoring the importance of informed food choices.The threat of Listeria monocytogenes serves as a reminder of the complex interplay between food safety, public health, and microbial pathogens. Vigilance, education, and research are essential in mitigating the risks posed by this bacterium, ensuring a safer and healthier future for all.
- ↑ Biological Materials Shipping Manual - campus services. (n.d.). https://campus.und.edu/safety/_files/docs/biological-materials-shipping-manual.pdf
- ↑ H. Hof, History and epidemiology of listeriosis, FEMS Immunology & Medical Microbiology, Volume 35, Issue 3, April 2003, Pages 199–202, https://doi.org/10.1016/S0928-8244(02)00471-6
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC88991/#:~:text=The%20first%20cases%20of%20human,meningitis%20(159%2C%20604).
- ↑ Seeliger HP. Listeriosis--history and actual developments. Infection. 1988;16 Suppl 2:S80-4. doi: 10.1007/BF01639726. PMID: 3138193.
- ↑ Seeliger HP. Listeriosis--history and actual developments. Infection. 1988;16 Suppl 2:S80-4. doi: 10.1007/BF01639726. PMID: 3138193.
- ↑ North, R. J. (1963). Some structural aspects of Listeria monocytogenes. Journal of Ultrastructure Research, 9(3–4), 187–197. https://doi.org/10.1016/s0022-5320(63)80001-5
- ↑ North, R. J. (1963). Some structural aspects of Listeria monocytogenes. Journal of Ultrastructure Research, 9(3–4), 187–197. https://doi.org/10.1016/s0022-5320(63)80001-5
- ↑ Hooper, L. V. (2015). Epithelial cell contributions to intestinal immunity. Advances in Immunology, 129–172. https://doi.org/10.1016/bs.ai.2014.11.003
- ↑ Rogalla D, Bomar PA. Listeria Monocytogenes. [Updated 2023 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534838/
- ↑ Rogalla D, Bomar PA. Listeria Monocytogenes. [Updated 2023 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534838/
- ↑ Rogalla D, Bomar PA. Listeria Monocytogenes. [Updated 2023 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534838/
- ↑ Shamloo E, Hosseini H, Abdi Moghadam Z, Halberg Larsen M, Haslberger A, Alebouyeh M. Importance of Listeria monocytogenes in food safety: a review of its prevalence, detection, and antibiotic resistance. Iran J Vet Res. 2019 Fall;20(4):241-254. PMID: 32042288; PMCID: PMC6983307.
- ↑ Shamloo E, Hosseini H, Abdi Moghadam Z, Halberg Larsen M, Haslberger A, Alebouyeh M. Importance of Listeria monocytogenes in food safety: a review of its prevalence, detection, and antibiotic resistance. Iran J Vet Res. 2019 Fall;20(4):241-254. PMID: 32042288; PMCID: PMC6983307.
- ↑ Shamloo E, Hosseini H, Abdi Moghadam Z, Halberg Larsen M, Haslberger A, Alebouyeh M. Importance of Listeria monocytogenes in food safety: a review of its prevalence, detection, and antibiotic resistance. Iran J Vet Res. 2019 Fall;20(4):241-254. PMID: 32042288; PMCID: PMC6983307.
- ↑ Centers for Disease Control and Prevention. (2022, October 25). People at risk - pregnant women and newborns. Centers for Disease Control and Prevention. https://www.cdc.gov/listeria/risk-groups/pregnant-women.html
- ↑ Centers for Disease Control and Prevention. (2022, October 25). People at risk - pregnant women and newborns. Centers for Disease Control and Prevention. https://www.cdc.gov/listeria/risk-groups/pregnant-women.html
- ↑ Mayo Foundation for Medical Education and Research. (n.d.). Listeria infection. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/listeria-infection/symptoms-causes/syc-20355269
- ↑ enters for Disease Control and Prevention. (2022b, November 8). People at risk - older adults. Centers for Disease Control and Prevention. https://www.cdc.gov/listeria/risk-groups/elderly.html
- ↑ enters for Disease Control and Prevention. (2022b, November 8). People at risk - older adults. Centers for Disease Control and Prevention. https://www.cdc.gov/listeria/risk-groups/elderly.html
- ↑ Center for Food Safety and Applied Nutrition. (n.d.). Listeria (listeriosis). U.S. Food and Drug Administration. https://www.fda.gov/food/foodborne-pathogens/listeria-listeriosis#:~:text=Mild%20symptoms%20may%20include%20a,loss%20of%20balance%2C%20and%20convulsions.
- ↑ Center for Food Safety and Applied Nutrition. (n.d.). Listeria (listeriosis). U.S. Food and Drug Administration. https://www.fda.gov/food/foodborne-pathogens/listeria-listeriosis#:~:text=Mild%20symptoms%20may%20include%20a,loss%20of%20balance%2C%20and%20convulsions.
- ↑ Listeriosis - symptoms, causes, treatment: Nord. National Organization for Rare Disorders. (2023, November 20). https://rarediseases.org/rare-diseases/listeriosis/
- ↑ Listeriosis - symptoms, causes, treatment: Nord. National Organization for Rare Disorders. (2023, November 20). https://rarediseases.org/rare-diseases/listeriosis/
- ↑ Listeriosis - symptoms, causes, treatment: Nord. National Organization for Rare Disorders. (2023, November 20). https://rarediseases.org/rare-diseases/listeriosis/
- ↑ Mary Donaldson, M. S. U. E. (2023, May 16). The serious and long-term effects of foodborne illness. Safe Food & Water. https://www.canr.msu.edu/news/the_serious_and_long-term_effects_of_foodborne_illness
- ↑ Mayo Foundation for Medical Education and Research. (2023, October 4). Meningitis. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/meningitis/symptoms-causes/syc-20350508
- ↑ Mayo Foundation for Medical Education and Research. (n.d.-b). Sepsis. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/sepsis/symptoms-causes/syc-20351214#
- ↑ Mayo Foundation for Medical Education and Research. (n.d.). Listeria infection. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/listeria-infection/symptoms-causes/syc-20355269
- ↑ Ishihara Y, Akazawa K. Treatment of Listeria monocytogenes bacteremia with oral levofloxacin in an immunocompromised patient. IDCases. 2023 Jan 7;31:e01680. doi: 10.1016/j.idcr.2023.e01680. PMID: 36660737; PMCID: PMC9843167.
- ↑ Ishihara Y, Akazawa K. Treatment of Listeria monocytogenes bacteremia with oral levofloxacin in an immunocompromised patient. IDCases. 2023 Jan 7;31:e01680. doi: 10.1016/j.idcr.2023.e01680. PMID: 36660737; PMCID: PMC9843167.
- ↑ WebMD. (n.d.). Levofloxacin Oral: Uses, side effects, interactions, pictures, warnings & dosing. WebMD. https://www.webmd.com/drugs/2/drug-14495-499/levofloxacin-oral/levofloxacin-solution-oral/details
- ↑ Ishihara Y, Akazawa K. Treatment of Listeria monocytogenes bacteremia with oral levofloxacin in an immunocompromised patient. IDCases. 2023 Jan 7;31:e01680. doi: 10.1016/j.idcr.2023.e01680. PMID: 36660737; PMCID: PMC9843167.
- ↑ Ishihara Y, Akazawa K. Treatment of Listeria monocytogenes bacteremia with oral levofloxacin in an immunocompromised patient. IDCases. 2023 Jan 7;31:e01680. doi: 10.1016/j.idcr.2023.e01680. PMID: 36660737; PMCID: PMC9843167.
- ↑ Mayo Foundation for Medical Education and Research. (2022, December 22). C-Reactive Protein Test. Mayo Clinic. https://www.mayoclinic.org/tests-procedures/c-reactive-protein-test/about/pac-20385228
- ↑ Ishihara Y, Akazawa K. Treatment of Listeria monocytogenes bacteremia with oral levofloxacin in an immunocompromised patient. IDCases. 2023 Jan 7;31:e01680. doi: 10.1016/j.idcr.2023.e01680. PMID: 36660737; PMCID: PMC9843167.
- ↑ Ishihara Y, Akazawa K. Treatment of Listeria monocytogenes bacteremia with oral levofloxacin in an immunocompromised patient. IDCases. 2023 Jan 7;31:e01680. doi: 10.1016/j.idcr.2023.e01680. PMID: 36660737; PMCID: PMC9843167.
- ↑ Ishihara Y, Akazawa K. Treatment of Listeria monocytogenes bacteremia with oral levofloxacin in an immunocompromised patient. IDCases. 2023 Jan 7;31:e01680. doi: 10.1016/j.idcr.2023.e01680. PMID: 36660737; PMCID: PMC9843167.
- ↑ Ishihara Y, Akazawa K. Treatment of Listeria monocytogenes bacteremia with oral levofloxacin in an immunocompromised patient. IDCases. 2023 Jan 7;31:e01680. doi: 10.1016/j.idcr.2023.e01680. PMID: 36660737; PMCID: PMC9843167.
- ↑ Mayo Foundation for Medical Education and Research. (2024, April 1). Gentamicin (injection route) description and brand names. Mayo Clinic. https://www.mayoclinic.org/drugs-supplements/gentamicin-injection-route/description/drg-20074471#:~:text=Gentamicin%20belongs%20to%20the%20class,flu%2C%20or%20other%20virus%20infections.
- ↑ U.S. National Library of Medicine. (n.d.). Ampicillin: Medlineplus Drug Information. MedlinePlus. https://medlineplus.gov/druginfo/meds/a685002.html
- ↑ Ishihara Y, Akazawa K. Treatment of Listeria monocytogenes bacteremia with oral levofloxacin in an immunocompromised patient. IDCases. 2023 Jan 7;31:e01680. doi: 10.1016/j.idcr.2023.e01680. PMID: 36660737; PMCID: PMC9843167.
- ↑ Ishihara Y, Akazawa K. Treatment of Listeria monocytogenes bacteremia with oral levofloxacin in an immunocompromised patient. IDCases. 2023 Jan 7;31:e01680. doi: 10.1016/j.idcr.2023.e01680. PMID: 36660737; PMCID: PMC9843167.
- ↑ Mohapatra RK, Mishra S, Tuglo LS, et al. Recurring food source-based Listeria outbreaks in the United States: An unsolved puzzle of concern? Health Sci Rep. 2024; 7:e1863. doi:10.1002/hsr2.1863
- ↑ Mohapatra RK, Mishra S, Tuglo LS, et al. Recurring food source-based Listeria outbreaks in the United States: An unsolved puzzle of concern? Health Sci Rep. 2024; 7:e1863. doi:10.1002/hsr2.1863
- ↑ Centers for Disease Control and Prevention. (2024, April 10). Listeria outbreak linked to queso fresco and Cotija cheese. Centers for Disease Control and Prevention. https://www.cdc.gov/listeria/outbreaks/cheese-02-24/index.html
- ↑ Mohapatra RK, Mishra S, Tuglo LS, et al. Recurring food source-based Listeria outbreaks in the United States: An unsolved puzzle of concern? Health Sci Rep. 2024; 7:e1863. doi:10.1002/hsr2.1863
- ↑ Mohapatra RK, Mishra S, Tuglo LS, et al. Recurring food source-based Listeria outbreaks in the United States: An unsolved puzzle of concern? Health Sci Rep. 2024; 7:e1863. doi:10.1002/hsr2.1863
- ↑ Centers for Disease Control and Prevention. (2023, June 13). Listeria outbreak linked to leafy greens. Centers for Disease Control and Prevention. https://www.cdc.gov/listeria/outbreaks/monocytogenes-02-23/index.html
- ↑ Centers for Disease Control and Prevention. (2023, June 13). Listeria outbreak linked to leafy greens. Centers for Disease Control and Prevention. https://www.cdc.gov/listeria/outbreaks/monocytogenes-02-23/index.html
- ↑ Centers for Disease Control and Prevention. (2023b, November 28). Prevent listeria. Centers for Disease Control and Prevention. https://www.cdc.gov/listeria/prevention.html
- ↑ Centers for Disease Control and Prevention. (2023b, November 28). Prevent Listeria. Centers for Disease Control and Prevention. https://www.cdc.gov/listeria/prevention.html
- ↑ Centers for Disease Control and Prevention. (2023a, March 29). Listeria outbreak linked to deli meat and cheese. Centers for Disease Control and Prevention. https://www.cdc.gov/listeria/outbreaks/deli-11-22/index.html
- ↑ Centers for Disease Control and Prevention. (2023a, March 29). Listeria outbreak linked to deli meat and cheese. Centers for Disease Control and Prevention. https://www.cdc.gov/listeria/outbreaks/deli-11-22/index.html
- ↑ Centers for Disease Control and Prevention. (2023b, November 28). Prevent listeria. Centers for Disease Control and Prevention. https://www.cdc.gov/listeria/prevention.html
- ↑ Centers for Disease Control and Prevention. (2023a, March 29). Listeria outbreak linked to deli meat and cheese. Centers for Disease Control and Prevention. https://www.cdc.gov/listeria/outbreaks/deli-11-22/index.html
- ↑ Centers for Disease Control and Prevention. (2023a, March 29). Listeria outbreak linked to deli meat and cheese. Centers for Disease Control and Prevention. https://www.cdc.gov/listeria/outbreaks/deli-11-22/index.html
- ↑ Orsi RH, Wiedmann M. Characteristics and distribution of Listeria spp., including Listeria species newly described since 2009. Appl Microbiol Biotechnol. 2016 Jun;100(12):5273-87. doi: 10.1007/s00253-016-7552-2. Epub 2016 Apr 29. PMID: 27129530; PMCID: PMC4875933.
- ↑ Orsi RH, Wiedmann M. Characteristics and distribution of Listeria spp., including Listeria species newly described since 2009. Appl Microbiol Biotechnol. 2016 Jun;100(12):5273-87. doi: 10.1007/s00253-016-7552-2. Epub 2016 Apr 29. PMID: 27129530; PMCID: PMC4875933.
- ↑ Orsi RH, Wiedmann M. Characteristics and distribution of Listeria spp., including Listeria species newly described since 2009. Appl Microbiol Biotechnol. 2016 Jun;100(12):5273-87. doi: 10.1007/s00253-016-7552-2. Epub 2016 Apr 29. PMID: 27129530; PMCID: PMC4875933.
- ↑ Orsi RH, Wiedmann M. Characteristics and distribution of Listeria spp., including Listeria species newly described since 2009. Appl Microbiol Biotechnol. 2016 Jun;100(12):5273-87. doi: 10.1007/s00253-016-7552-2. Epub 2016 Apr 29. PMID: 27129530; PMCID: PMC4875933.
- ↑ Orsi RH, Wiedmann M. Characteristics and distribution of Listeria spp., including Listeria species newly described since 2009. Appl Microbiol Biotechnol. 2016 Jun;100(12):5273-87. doi: 10.1007/s00253-016-7552-2. Epub 2016 Apr 29. PMID: 27129530; PMCID: PMC4875933.
- ↑ Ph.D., J. R., Graham Boorse, Ph. D., & M.S., A. M. (2022, January 18). Alpha and beta hemolytic streptococcus. Red Mountain Microbiology. https://open.maricopa.edu/redmountainmicro/chapter/alpha-and-beta-hemolytic-streptococcus/#:~:text=identification%20even%20further.-,HEMOLYSIS,as%20beta%2C%20alpha%20and%20gamma.
- ↑ Orsi RH, Wiedmann M. Characteristics and distribution of Listeria spp., including Listeria species newly described since 2009. Appl Microbiol Biotechnol. 2016 Jun;100(12):5273-87. doi: 10.1007/s00253-016-7552-2. Epub 2016 Apr 29. PMID: 27129530; PMCID: PMC4875933.
- ↑ Orsi RH, Wiedmann M. Characteristics and distribution of Listeria spp., including Listeria species newly described since 2009. Appl Microbiol Biotechnol. 2016 Jun;100(12):5273-87. doi: 10.1007/s00253-016-7552-2. Epub 2016 Apr 29. PMID: 27129530; PMCID: PMC4875933.
- ↑ Orsi RH, Wiedmann M. Characteristics and distribution of Listeria spp., including Listeria species newly described since 2009. Appl Microbiol Biotechnol. 2016 Jun;100(12):5273-87. doi: 10.1007/s00253-016-7552-2. Epub 2016 Apr 29. PMID: 27129530; PMCID: PMC4875933.
- ↑ Orsi RH, Wiedmann M. Characteristics and distribution of Listeria spp., including Listeria species newly described since 2009. Appl Microbiol Biotechnol. 2016 Jun;100(12):5273-87. doi: 10.1007/s00253-016-7552-2. Epub 2016 Apr 29. PMID: 27129530; PMCID: PMC4875933.
- ↑ Oladejo, M., Paterson, Y., & Wood, L. M. (2021, February 26). Clinical experience and recent advances in the development of listeria-based tumor immunotherapies. Frontiers. https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.642316/full
- ↑ Oladejo, M., Paterson, Y., & Wood, L. M. (2021, February 26). Clinical experience and recent advances in the development of listeria-based tumor immunotherapies. Frontiers. https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.642316/full
- ↑ Oladejo, M., Paterson, Y., & Wood, L. M. (2021, February 26). Clinical experience and recent advances in the development of listeria-based tumor immunotherapies. Frontiers. https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.642316/full
- ↑ Oladejo, M., Paterson, Y., & Wood, L. M. (2021, February 26). Clinical experience and recent advances in the development of listeria-based tumor immunotherapies. Frontiers. https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.642316/full
- ↑ Oladejo, M., Paterson, Y., & Wood, L. M. (2021, February 26). Clinical experience and recent advances in the development of listeria-based tumor immunotherapies. Frontiers. https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.642316/full
- ↑ Oladejo, M., Paterson, Y., & Wood, L. M. (2021, February 26). Clinical experience and recent advances in the development of listeria-based tumor immunotherapies. Frontiers. https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.642316/full
- ↑ Oladejo, M., Paterson, Y., & Wood, L. M. (2021, February 26). Clinical experience and recent advances in the development of listeria-based tumor immunotherapies. Frontiers. https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.642316/full
- ↑ Oladejo, M., Paterson, Y., & Wood, L. M. (2021, February 26). Clinical experience and recent advances in the development of listeria-based tumor immunotherapies. Frontiers. https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.642316/full
- ↑ Oladejo, M., Paterson, Y., & Wood, L. M. (2021, February 26). Clinical experience and recent advances in the development of listeria-based tumor immunotherapies. Frontiers. https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.642316/full
- ↑ Oladejo, M., Paterson, Y., & Wood, L. M. (2021, February 26). Clinical experience and recent advances in the development of listeria-based tumor immunotherapies. Frontiers. https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.642316/full
