Tuberculosis in India
Introduction
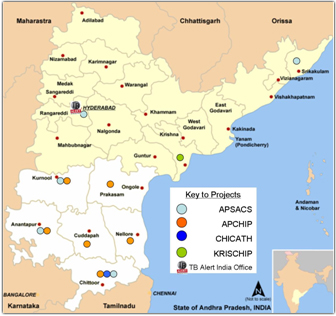
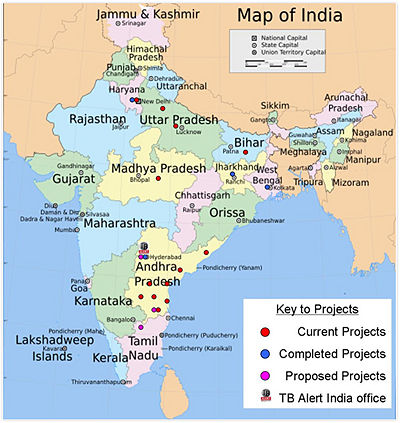
Tuberculosis, also known as TB, is an infectious disease that is prevalent in attacking the lungs but also has the capability to invade other parts of the body. It infects the host through particles known as bacilli that are transferred through air. Not only is this microbe highly contagious, but it affects one-third of the worlds population(1), though only 10% show symptoms of TB and can transmit the disease to others. From the one-third infected, the most cases are in India. In fact, today in India more than 250,000 people die from tuberculosis every year(9). Mycobacterium tuberculosis is an etiological agent of tuberculosis in humans, which are the only reservoirs for this bacterium(2). All parts of India are known to be affected by TB infections but the state of Andhra Pradesh has the highest rate of the disease amongst all of India(15).
Kingdom: Bacteria
Phylum: Actinobacteria
Order: Actinomycetales
Suborder: Corynebacterineae
Family: Mycobacteriaceae
Genus: Mycobacterium
Species: M. tuberculosis (2)
Description of Tuberculosis
Description of the Microbe
Many cases of tuberculosis are caused by the intracellular pathogen, Mycobacterium tuberculosis. Mycobacteria are non-motile, and have a slender, rod-shaped form (4). Mycobacteria tuberculosis are aerobic bacteria; hence they are able to successfully grow in host tissues of high oxygen concentration and infect mononuclear phagocytes, or white blood cells. Since M. tuberculosis is highly aerobic, it normally survives in the respiratory system of the host where there are high levels of oxygen (4). The complex lipid biosynthesis enables M. tuberculosis to form a thick lipid cell wall which plays a crucial role in its survival and virulence. Thus, the cell wall’s structure allows the bacteria to survive within macrophages and provides a resistant barrier against common drugs (4).
M. tuberculosis is difficult to study in the laboratory mainly due to its lengthy growth and tendency to form clumps, making it difficult to handle. Mycobacteria have very slow growth rate, with a doubling time of 12 to 18 hours, and takes more than 3 weeks to develop colonies (4).The cells clump together because of the high lipid content of the cell wall; consequently, this characteristic of M.tuberculosis also makes it immune to gram positive staining(3). Acid-fast techniques are used to stain Mycobacteria because of their thick waxy cell wall that primarily contains mycolic acid which resists ethanol-based and acidic organic decolorization solvents(4). In addition,
Studies have shown that M. tuberculosis attains an unusual immunopathology that causes either hypoinflammatory or hyperinflammatory response which reduces the survival of its host. Hypervirulent M. tuberculosis mutants are determined to have deletions in their cell wall, modifying the regulator which enables them to increase the expression of granuloma (3). Granulomas prevent the spread of the infection by confining bacteria into a compact collection of different immune cells and activated macrophages. As a result, toxins are released by the immune cells which kill the bacteria (3). Furthermore, granulomas become dormant and are sealed off by scar tissue. Dormancy regulon is a process by which M. tuberculosis is exposed to nitric oxide and carbon monoxide in the absence of aerobic respiration, which enables it to survive in anaerobic conditions(5). If any bacilli survive, they might be able to reactivate years later. This bacterium reactivates by stimulating or triggering immune cells to release substances that render the host tissue cells that are sensitive to killing it (5). Furthermore, immune cells might choose to release substances that liquefy the bacteria-containing center of the granuloma. When the granuloma erodes, the liquefied material is released into the airway and cavities form in the lung (5). Oxygen and carbon dioxide then enter the space creating a favorable environment causing bacilli to replicate in large numbers. M. tuberculosis has a flexible modular respiratory system enabling it to best utilize the energy production of its environments (3).
Transmission of disease
Tuberculosis is caused by a rod-shaped bacterium called Mycobacterium tuberculosis (Mtb) which primarily enters the body by inhaling Mtb-contaminated air. Symptoms of Tuberculosis vary depending on the treatment that a person is under and how much the disease has progressed. Once a person is exposed to the bacteria, the infection is categorized into three forms: latent Tuberculosis infection, active Tuberculosis, and multi-drug resistant tuberculosis. A person with latent Tuberculosis has an immune system that is competent to prevent the spread and keep Mtb to remain in its dormant form. A person with active tuberculosis is capable of spreading the bacteria to others and begins to display common symptoms. Mtb begins to grow and infect mainly lungs and possibly spreads to other extrapulmonary parts of the body(6). Active tuberculosis can be treated by taking antibiotics for several months even though it is more preferable to get treatment during latent TB infection. Once a person fails to take medications or get treatments consistently until Tuberculosis is completely cured, it can develop into a more severe form, known as multi-drug resistant tuberculosis (MDR-TB). MDR-TB develops as the bacteria becomes resistant to the antibiotics that it has already encountered, which could ultimately lead to death unless taken alternate medications or treatments(8).
A person with active pulmonary Tuberculosis can simply release the bacteria into the air and infect others by exhaling, coughing, spitting, laughing, etc. When Mycobacterium tuberculosis enters a healthy person, symptoms may not readily appear since the immune system is strong enough to prevent the bacteria from spreading throughout the body (bacteria is still alive but not spreading). On the other hand, others are more prone to active tuberculosis if they:
•are living in contact with someone that has active Tuberculosis
•are nurses or doctors whom are taking care of patients with active Tuberculosis
•have weak immune system from having illness (such as HIV)
•do not have healthcare/treatment available to cure or prevent the bacteria from spreading
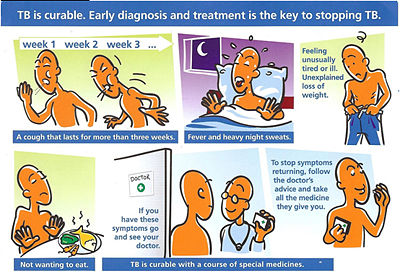
Once a person has active Tuberculosis, they will display common symptoms such as sweating, fever, fatigue, consistent coughing for a significant period of time, and difficulty in breathing(8, 10).
Prevention
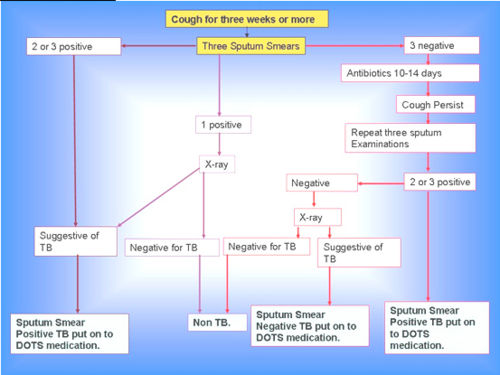
Due to the fact that India carries the highest number of TB cases in the world,there are many projects and preventative procedures that are and have been taking place due to this major endemic since the early nineties. Programs such as DOTS, or Directly Observed Treatment-Short-course, a global initiative with the goal to help prevent the spread of tuberculosis by providing direct treatment of the infection. Providing proper treatment, not only prevents the infection but also eliminates the chances of the development of Multi-Drug Resistant Tuberculosis (MDR-TB) which cannot be treated with conventional medications. In India RNTCP, also known as the Revised National Tuberculosis Control Programme, applies the principles and implementations of the preventative procedures of the DOTS program to all parts of India. The following are some of the accomplishments of the program:
1. The accuracy of TB diagnosis has more than doubled.
2. The success rate of actual treatment and recovery from the infection is up to 85%.
3. Poverty is alleviated by saving lives, or reducing the duration of illness and preventing new infectious cases.
4. The emergence of MDR-TB is prevented by ensuring patient adherence to treatment and uninterrupted supply of anti -TB drugs.
(10)
Why is TB a problem in India?
Tuberculosis became prevalent, starting in the 1950s and continued to threaten the population in India affecting two out of five people. It is also known as the “disease of the poor” because it is commonly spread amongst people living in underprivileged areas. People who live in underprivilaged areas are most targeted because of their overcrowded living situation in addition to their malnourishment. A person who is malnourished has a weak immune system which is incapable of fighting off the bacteria (Mycobacterium tuberculosis) that causes Tuberculosis. Once a person in such overcrowded community obtains the disease, there is a much higher chance that Tuberculosis will spread more rapidly within the community. Moreover, muti-drug resistant tuberculosis develops more frequently in India because of their insufficient healthcare. Most patients take antibiotics irregularly or stop taking medications before they are completely "cured." In addition, women ignore the symptoms and neglect to get the treatment. Since women take care of the household, they spread the MtB more readily to their children and husbands. Although Tuberculosis is problematic world-wide, it is considered more deadly in India because of an increase in emerging cases of muti-drug resistant Tuberculosis which results in a high percentage of death from the disease. (7). In the last two decades, the spread of HIV in India has increased the vulnerability to Tuberculosis within the population. Comparing people who were HIV+ and HIV-, HIV+ appeared to have 50~60% lifetime risk whereas HIV- had 10% lifetime risk to develop Tuberculosis. Regardless of the government’s effort to prevent the spread of Tuberculosis, India has become one of the “highest Tuberculosis burdened countries” by presenting one-fifth of the entire global Tuberculosis cases(7).
What is being done to address this problem
The most common treatment for Tuberculosis involves the prescription of one or more of the six antibiotics (pyrazinamide which inhibits fatty acid synthesis, isoniazid which inhibits mycolic acid synthesis, cycloserine or ethambutol which inhibit cell wall biosynthesis, capreomycin which inhibits the bacterium’s peptide synthesis, or rifampicin which acts on RNA polymerase) for the long term, usually between six months to three years. Even though these anti-tuberculosis medications have been available for decades now, death rates and incidents of the infectious disease have not been declining significantly in India. For this reason, a government supported program called DOTS has been implemented in the regions of the country since 1993, and since 2006 has been extended to provide coverage to all of India’s population of more than one billion people. The strategy of the DOTS program (or Revised National Tuberculosis Control Programme as it is known in India) is to provide plentiful medication and supervised care to all those infected with the disease(7). All affected individuals are guaranteed the necessary amount of the top anti-tuberculosis drugs for the whole course of treatment. Furthermore, the affected individuals are supervised to ensure the proper intake of the medicine. Under the program, any individual can be screened for the disease free of charge (10). Today, the success rate of the program is 85%, meaning that 85% of all those who receive or have received treatment are no longer infected with Tuberculosis(11). Though the program has shown significant success in treating and diagnosing emerging cases of the disease, Tuberculosis is still a major problem in India as is evident by the appearance of drug resistant tuberculosis due to patients that do not complete the medication treatment for the prescribed term that has been a result of economic hardships(11). It would be fair to say that with improved quality of life more affected individuals would be able to complete the advised anti-tuberculosis treatment, since most of those affected live in poverty.
What else could be done
Currently, a number of studies and advancements are being done to resolve the situation in India. Researchers have determined that the most common Mycobacterium tuberculosis strains are the Central-Asian Clade in Northern India and the East-African-Indian Clade in Southern India (12). Understanding the genetic similarities and differences between these two strains in comparison to other tuberculosis strains helps build vaccinations more specific to the cause in India. Targeting regions unique to certain Indian strains, such as the TbD1 region which is only found in the East-African-Indian Clade, may help in creating a vaccine with greater specificity. One of the more common vaccines against tuberculosis is bacillus Calmette-Guérin, a live but weakened strain of bovine tuberculosis bacillus. Though widely used throughout the world, this vaccine only shows an efficacy rate of about 50% (13). New and more effective treatments are being researched to identify more common extracellular proteins displayed by infected host cells. Identifying these key proteins further assists in targeting key markers for vaccines. Additionally, researchers are using other means to conduct research on tuberculosis resistance and vaccination. The use of animal models, such as mice and rabbits, helps test new vaccines and treatments as these and other species share many physiological commonalities with humans (14). Though testing with these species does not give exact results as testing within a human population, the methods are generally more cost efficient and safer for humans while still producing useful results. Further research in the specific strains in India as well as the use of animal models will progress science forward into creating a more tuberculosis preventive India.
References
1. American Lung Association, May 2007, Tuberculosis (TB) http://www.lungusa.org/site/apps/nlnet/content3.aspx?c=dvLUK9O0E&b=2060731&content_id={50031760-2D7C-4FFF-AD75-4C49BDD1CD7D}¬oc=1&gclid=CPamgJK9v5wCFRxNagodKkC_ng (August 24,2009)
2. Todar,Kenneth PhD., Todar's Online Textbook of Bacteriology, http://www.textbookofbacteriology.net/tuberculosis.html (August 22,2009)
3. Shimono, Nobuyuki; Morici, Lisa; Casali, Nicola; Cantrell, Sally; Sidders, Ben; Ehrt, Sabine; and Riley, Lee W. “ Hypervirulent mutant of Mycobacterium tuberculosis resulting from disruption of the mcel operon.” Proc Natl Acad Sci U S A. 2003. 100(26): 15918-15923, http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=14663145.
4. Tan, Yi-Wei; Meng, Shufang; Li, Haijing; and Stratton, Charles W. “PCR enhances Acid-Fast Bacillus Stain-Based Rapid Detection of Mycobacterium tuberculosis.” J Clin Microbiol. 2004. 42(4): 1849-1850, http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=387609&tool=pmcentrez.
5. Kaufmann, Stefan H.E.; Cole, Stewart T.; Mizrahi, Valerie; Rubin, Eric; and Nathan, Carl. “Mycobacterium tuberculosis and the host response.” J Exp Med. 2005. 201(11): 1693-1697, http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=15939785.
6. Griffith D, Kerr C (1996). "Tuberculosis: disease of the past, disease of the present". Journal of Perianesthesia Nursing, Volume 11 issue 4: P 240–5.
7. Ministry of Health and Family Welfare, TB India 2007, RNTCP status report, http://www.tbcindia.org/pdfs/TB%20India%202007.pdf (August 18, 2009)
8. World Health Organization (WHO). "Global and regional incidence", Tuberculosis Fact sheet N°104, WHO, March 2006,http://www.who.int/mediacentre/factsheets/fs104/en/index.html(accessed August 20,2009).
9. World Health Organization: Epidemiology of TB in the Region (South-East Asia), http://www.searo.who.int/en/Section10/Section2097/Section2100_10639.htm.
10. TBC India: Directorate General of Health Services, Ministry of Health and Family Welfare: About RNTCP, http://www.tbcindia.org/RNTCP.asp.
11. Khatri, G. R., and Thomas R. Frieden. "Controlling Tuberculosis in India." The New England Journal of Medicine 347.18 (2002): 14211427.Web, http://content.nejm.org/cgi/content/full/347/18/1420.
12. Arora J, Singh UB, Suresh N, Rana T, Porwal C, Kaushik A, Pande JN. "Characterization of predominant Mycobacterium tuberculosis strains from different subpopulations of India." Infection, Genetics and Evolution (2009): 832-839. http://www.ncbi.nlm.nih.gov/pubmed/19463970?log$=activity
13. Horwitz MA, Harth G, Dillon BJ, Maslesa-Galic' S. "Recombinant bacillus calmette-guerin (BCG) vaccines expressing the Mycobacterium tuberculosis 30-kDa major secretory protein induce greater protective immunity against tuberculosis than conventional BCG vaccines in a highly susceptible animal model." Proceedings of the National Academy of Sciences of the U.S.A. (2000): 13853-8. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=11095745
14. U.D. Gupta, V.M. Katoch, "Animal models of tuberculosis for vaccine development." Indian Journal of Medical Research (2009): 11-18. http://icmr.nic.in/ijmr/2009/0103.pdf
15. Chauhan, Tilak, TB Alert India, http://www.tbalertindia.org, (August 22, 2009).
16. Getty Images, www.gettyimages.com, (August 24,2009).
Edited by Alexander Abejar, Yekaterina Tarasova, Kimya Panah, Jeung Lee, Huyen Htdao, students of Rachel Larsen
*** Special Thanks to Tilak Chauhan from TB Alert India for permission to use their illustrations @ www.tbalertindia.org ***