Change in the Pharyngeal Microbial Environment after a Tonsillectomy: Difference between revisions
No edit summary |
No edit summary |
||
| Line 25: | Line 25: | ||
==What is a Tonsillectomy?== | ==What is a Tonsillectomy?== | ||
A tonsillectomy is the surgical removal of the tonsils which is performed as a last resort invasive effort to fight recurrent tonsillitis infection, cancer, and other issues that cannot be solved via antibiotics <ref name=aa/>. Tonsillectomies previously were the most popular procedure used to combat respiratory disease, however, now the prevalence of such procedures has decreased to less than one half of the number from 40 years ago <ref name=c/>. The 20-30 minute procedure includes the use of general anesthesia, and the severing of the mucous membrane by electrocautery, or cold-knife cutting, or snare pulling, and then more electrocautery or sutures to stop the bleeding <ref name=d/>. Due to the extremely high risk factors and complications that are associated with this procedure, it is only recommended if certain requirements are met. The Mayo clinic defined its criteria for surgery as the following, “Seven episodes of tonsillitis in a single year, or five episodes of tonsillitis in each of two consecutive years, or three episodes of tonsillitis in each of three consecutive years” <ref name=c/>. After the procedure, painful swallowing and a sore incision site is to be expected. As is dehydration if fluid intake is decreased and possibly nausea <ref name=c/>. The greatest concern comes from the risk of hemorrhage, which can arise at any moment after surgery when the scabs covering the incision site start to flake off <ref name=c/>. Post tonsillectomy hemorrhage, which varies in risk from 0.28%-20%, is always considered an emergency and requires immediate attention and likely surgical intervention <ref name=e/>. | A tonsillectomy is the surgical removal of the tonsils which is performed as a last resort invasive effort to fight recurrent tonsillitis infection, cancer, and other issues that cannot be solved via antibiotics <ref name=aa/>. Tonsillectomies previously were the most popular procedure used to combat respiratory disease, however, now the prevalence of such procedures has decreased to less than one half of the number from 40 years ago <ref name=c/>. The 20-30 minute procedure includes the use of general anesthesia, and the severing of the mucous membrane by electrocautery, or cold-knife cutting, or snare pulling, and then more electrocautery or sutures to stop the bleeding <ref name=d/>. Due to the extremely high risk factors and complications that are associated with this procedure, it is only recommended if certain requirements are met. The Mayo clinic defined its criteria for surgery as the following, “Seven episodes of tonsillitis in a single year, or five episodes of tonsillitis in each of two consecutive years, or three episodes of tonsillitis in each of three consecutive years” <ref name=c/>. After the procedure, painful swallowing and a sore incision site is to be expected. As is dehydration if fluid intake is decreased and possibly nausea <ref name=c/>. The greatest concern comes from the risk of hemorrhage, which can arise at any moment after surgery when the scabs covering the incision site start to flake off <ref name=c/>. Post tonsillectomy hemorrhage, which varies in risk from 0.28%-20%, is always considered an emergency and requires immediate attention and likely surgical intervention <ref name=e/>. Individuals over the age of twelve are at greater risk for complication and higher levels of pain, due to the buildup of scar tissue on the tonsils themselves and an overall larger surface area <ref name=e/>. Therefore, some doctors do not recommend this procedure for adults unless absolutely necessary. | ||
==Pre-Tonsillectomy Microbial Environment== | ==Pre-Tonsillectomy Microbial Environment== | ||
Revision as of 15:42, 9 April 2024
By Lindsey Abramson
Introduction
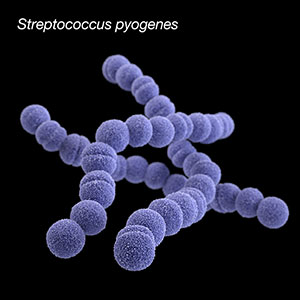
Tonsillectomies, the surgical removal of the tonsils, are performed on individuals with recurrent tonsillitis infections, recurrent strep throat, enlarged tonsils, and other issues such as cancerous cells [1]. The goal of this radical procedure is the eradication of bacteria assuming antibiotics have been frequently used and failed / resistance was developed [2]. Streptococcus pyogenes (also called group A streptococci, or GAS) is the causative agent bacterium of strep throat, one of the leading causes that push individuals towards an elective tonsillectomy [3]. Although viruses are also common, other problematic bacteria include: Staphylococcus aureus, Haemophilus influenzae, Streptococcus pneumoniae, Escherichia coli, and Pseudomonas aeruginosa [2].
At right is a sample image insertion. It works for any image uploaded anywhere to MicrobeWiki.
The insertion code consists of:
Double brackets: [[
Filename: PHIL_1181_lores.jpg
Thumbnail status: |thumb|
Pixel size: |300px|
Placement on page: |right|
Legend/credit: Magnified 20,000X, this colorized scanning electron micrograph (SEM) depicts a grouping of methicillin resistant Staphylococcus aureus (MRSA) bacteria. Photo credit: CDC. Every image requires a link to the source.
Closed double brackets: ]]
Other examples:
Bold
Italic
Subscript: H2O
Superscript: Fe3+
What is a Tonsillectomy?
A tonsillectomy is the surgical removal of the tonsils which is performed as a last resort invasive effort to fight recurrent tonsillitis infection, cancer, and other issues that cannot be solved via antibiotics [1]. Tonsillectomies previously were the most popular procedure used to combat respiratory disease, however, now the prevalence of such procedures has decreased to less than one half of the number from 40 years ago [4]. The 20-30 minute procedure includes the use of general anesthesia, and the severing of the mucous membrane by electrocautery, or cold-knife cutting, or snare pulling, and then more electrocautery or sutures to stop the bleeding [5]. Due to the extremely high risk factors and complications that are associated with this procedure, it is only recommended if certain requirements are met. The Mayo clinic defined its criteria for surgery as the following, “Seven episodes of tonsillitis in a single year, or five episodes of tonsillitis in each of two consecutive years, or three episodes of tonsillitis in each of three consecutive years” [4]. After the procedure, painful swallowing and a sore incision site is to be expected. As is dehydration if fluid intake is decreased and possibly nausea [4]. The greatest concern comes from the risk of hemorrhage, which can arise at any moment after surgery when the scabs covering the incision site start to flake off [4]. Post tonsillectomy hemorrhage, which varies in risk from 0.28%-20%, is always considered an emergency and requires immediate attention and likely surgical intervention [6]. Individuals over the age of twelve are at greater risk for complication and higher levels of pain, due to the buildup of scar tissue on the tonsils themselves and an overall larger surface area [6]. Therefore, some doctors do not recommend this procedure for adults unless absolutely necessary.
Pre-Tonsillectomy Microbial Environment
Include some current research, with at least one figure showing data.
Post-Tonsillectomy Microbial Environment
Include some current research, with at least one figure showing data.
Success Rates
Conclusion
References
- ↑ 1.0 1.1 1.2 Brietzke, S.E. and Andreoli, S.M., 2021. Systematic review and meta-analysis of the change in pharyngeal bacterial cultures after pediatric tonsillectomy. Otolaryngology–Head and Neck Surgery, 164(2), pp.264-270.
- ↑ 2.0 2.1 2.2 Yildizoglu, U., Polat, B., Gumral, R., Kilic, A., Tosun, F. and Gerek, M., 2015. Effect of antibiotic use on bacterial flora of tonsil core in patients with recurrent tonsillitis. European Archives of Oto-Rhino-Laryngology, 272, pp.1525-1528.
- ↑ 3.0 3.1 Slonczewski, S.L, Foster, J.W, and Zinser, E, 2024. Microbiology an evolving science, sixth edition. W.W. Norton and Company.
- ↑ 4.0 4.1 4.2 4.3 4.4 Stuck, B.A., Windfuhr, J.P., Genzwürker, H., Schroten, H., Tenenbaum, T. and Götte, K., 2008. Tonsillectomy in children. Deutsches Ärzteblatt International, 105(49), p.852.
- ↑ 5.0 5.1 Younis, R.T. and Lazar, R.H., 2002. History and current practice of tonsillectomy. The Laryngoscope, 112(S100), pp.3-5.
- ↑ 6.0 6.1 6.2 Liu, J.H., Anderson, K.E., Willging, J.P., Myer III, C.M., Shott, S.R., Bratcher, G.O. and Cotton, R.T., 2001. Posttonsillectomy hemorrhage: what is it and what should be recorded?. Archives of Otolaryngology–Head & Neck Surgery, 127(10), pp.1271-1275.
Authored for BIOL 238 Microbiology, taught by Joan Slonczewski,at Kenyon College,2024
