Nasal passageway: Difference between revisions
No edit summary |
|||
| (69 intermediate revisions by 8 users not shown) | |||
| Line 1: | Line 1: | ||
{{ | {{Uncurated}} | ||
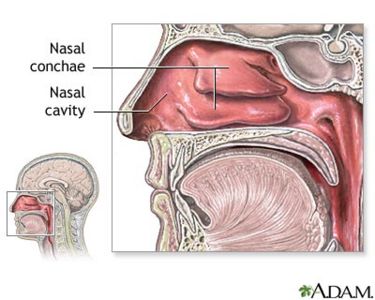
[[Image:Nasal anatomy.jpg|thumb|right|375px | From [http://www.nlm.nih.gov/ MedlinePlus]]] | [[Image:Nasal anatomy.jpg|thumb|right|375px | From [http://www.nlm.nih.gov/ MedlinePlus]]] | ||
| Line 5: | Line 5: | ||
==Introduction to the Nasal Passageway== | ==Introduction to the Nasal Passageway== | ||
The nose | The nose is one of the few openings that bacteria have direct access to get inside the body. The nasal passage is important for filtering the air that we breathe in and it also stops tiny foreign particles or microorganisms from entering the body. What many people do not know is that the nose and nasal passages are, or can be , the perfect environment for some bacteria, good and bad. This page will focus on describing what makes the nasal passages such a hospitable environment for the bacteria to grow and live inside the nose. | ||
==Description of Nasal Passageway== | ==Description of Nasal Passageway== | ||
| Line 13: | Line 13: | ||
The main entry to the nasal passageway is through the nostrils, inside the nose, which is located on the face. From there, the passageway extends to the throat. The nose is the organ of smell located in the middle of the face. The internal part of the nose lies above the roof of the mouth. It is supported by bone and cartilage. The bony part is formed mainly by the nasal bones on each side and the frontal process of the maxillary bone. The nasal cavity is the air passage starting at the nostril (opening of the nose) and ending at the back of the throat(4). Nasal Obstruction is a partial or complete blockage of one or both of these air passages. | The main entry to the nasal passageway is through the nostrils, inside the nose, which is located on the face. From there, the passageway extends to the throat. The nose is the organ of smell located in the middle of the face. The internal part of the nose lies above the roof of the mouth. It is supported by bone and cartilage. The bony part is formed mainly by the nasal bones on each side and the frontal process of the maxillary bone. The nasal cavity is the air passage starting at the nostril (opening of the nose) and ending at the back of the throat(4). Nasal Obstruction is a partial or complete blockage of one or both of these air passages. The nose is one of the few openings of the body for bacteria and microbes to go inside the body. | ||
===Physical Conditions of the Nasal Passageway=== | ===Physical Conditions of the Nasal Passageway=== | ||
| Line 35: | Line 35: | ||
===Influence by Adjacent Communities=== | ===Influence by Adjacent Communities=== | ||
[[Image:Staphylococci.jpg|thumb|right|250px | Staphylococci -picture from [http://phil.cdc.gov/phil/ Public Health Image Library ]]] | [[Image:Staphylococci.jpg|thumb|right|250px | Staphylococci -picture from [http://phil.cdc.gov/phil/ Public Health Image Library ]]] | ||
The nasal passageway is close to other niches like the lungs, mouth, and throat. The nasal passage is influenced by the bacteria colonies of [[Staphylococcus aureus]]. Other pathogens include such as Haemophilus influenzae, S. pneumonia, Nisseria meningitides, Moraxella catarrhalis and S. aureus . Successful colonization depends not only on the ability of S. aureus to survive host factors but also on coexistence with other bacteria. An airborne bacterium also causes allergies and irritation. | The nasal passageway is close to other niches like the lungs, mouth, and throat. The nasal passage is influenced by the bacteria colonies of ''[[Staphylococcus aureus]]''. Other pathogens include such as ''Haemophilus influenzae'', ''S. pneumonia'', ''Nisseria meningitides'', ''Moraxella catarrhalis'' and ''S. aureus''. Successful colonization depends not only on the ability of ''S. aureus'' to survive host factors but also on coexistence with other bacteria. An airborne bacterium also causes allergies and irritation. | ||
Sinuses: The diseased maxillary and ethmoid sinuses are most commonly associated with affecting the nasal passages by causing inflammation and congestion. One of the diseases caused by the communities of bacteria is sinusitis. The ability of bacteria to infect the sinuses must first be set up by conditions that create a favorable environment in the sinus cavities. The inflammation in the sinuses is chronic do begin with.(5) The causes for such chronic sinusitis cases are sometimes unclear. The Bacteria that causes the sinusitis are Streptococcus pneumonia, H. influenzae, Moraxella catarrhalis. The symptoms of this disease are severe headache, pain or pressure in the areas of the face, cough, and fever. It could also be damaging to the mucous membrane if left untreated. Bipolaris specifera is a fungus that also causes sinus. This fungus is very fast growing and they grow at 25 degrees Celcius. In their growing process they change their shape and color too (23). | Sinuses: The diseased maxillary and ethmoid sinuses are most commonly associated with affecting the nasal passages by causing inflammation and congestion. One of the diseases caused by the communities of bacteria is sinusitis. The ability of bacteria to infect the sinuses must first be set up by conditions that create a favorable environment in the sinus cavities. The inflammation in the sinuses is chronic do begin with.(5) The causes for such chronic sinusitis cases are sometimes unclear. The Bacteria that causes the sinusitis are ''Streptococcus pneumonia'', ''H. influenzae'', ''Moraxella catarrhalis''. The symptoms of this disease are severe headache, pain or pressure in the areas of the face, cough, and fever. It could also be damaging to the mucous membrane if left untreated. ''Bipolaris specifera'' is a fungus that also causes sinus. This fungus is very fast growing and they grow at 25 degrees Celcius. In their growing process they change their shape and color too (23). | ||
Throat: The throat is connected to the nasal passageway and contains aerobic, gram-positive bacteria which are characterized by hemolysis. An example of a pathogenic bacteria in the throat is [[Streptococcus pyogenes]], which can infect when the immune system is down and cause diseases such as scarlet fever and pharyngitis (strep throat) among others. An example of nonpathogenic bacteria in the throat is [[Streptococcus salivarius]] which may enter the bloodstream and may cause diseases such as septicemia although not very often. These diseases mostly affect the throat, but may move upwards to cause nasal passageway infections. Sore throat also affects the conditions in the nose by causing post nasal drip. | Throat: The throat is connected to the nasal passageway and contains aerobic, gram-positive bacteria which are characterized by hemolysis. An example of a pathogenic bacteria in the throat is ''[[Streptococcus pyogenes]]'', which can infect when the immune system is down and cause diseases such as scarlet fever and pharyngitis (strep throat) among others. An example of nonpathogenic bacteria in the throat is ''[[Streptococcus salivarius]]'' which may enter the bloodstream and may cause diseases such as septicemia although not very often. These diseases mostly affect the throat, but may move upwards to cause nasal passageway infections. Sore throat also affects the conditions in the nose by causing post nasal drip. | ||
Bipolaris Specifera: Polyps and fungal diseases have made their way through dura and extended far intracranially, especially in the frontal recess region and the roof of the anterior ethmoid. They obstruct both the nostrils with glassy polyps. Hemotoxylin and eosin (H&E) and Gomoris methenamine silver (GMS) both affect the mucus lining of nasal sinuses. This is a very rare combination of two commonly different diseases found in the same location and caused by the same pathogen, Bipolaris Specifera (23)”. | |||
===Conditions under which the environment changes=== | ===Conditions under which the environment changes=== | ||
| Line 54: | Line 56: | ||
===Which microbes are present in the Nasal Passageway?=== | ===Which microbes are present in the Nasal Passageway?=== | ||
Even though we cannot see them with our naked eye, microscopic organisms are living inside our nasal passageways. Although most of these bacteria are non-pathogenic, some may induce illness if they successfully break through the bodies defense systems. Some examples of these non-pathogenic bacteria are Streptococcus, Neisseria, Haemophilus, and Micrococcus. Some of the pathogenic examples include Staphylococcus aureus, Corynebacterium diphtheriae, Streptococcus pneumoniae, and Haemophilus influenzae among others. (15) | Even though we cannot see them with our naked eye, microscopic organisms are living inside our nasal passageways. Although most of these bacteria are non-pathogenic, some may induce illness if they successfully break through the bodies defense systems. Some examples of these non-pathogenic bacteria are ''Streptococcus'', ''Neisseria'', ''Haemophilus'', and ''Micrococcus''. Some of the pathogenic examples include ''Staphylococcus aureus'', ''Corynebacterium diphtheriae'', ''Streptococcus pneumoniae'', and ''Haemophilus influenzae'' among others. (15) | ||
Normal: | Normal: | ||
[[Staphylococcus epidermidis]] with Corynebacteria predominantly colonizes the upper respiratory tract, especially the nostrils. S. epidermidis covers 90%-100% staphylococci from the nasal cavity when S. aureus is not present. When S. aureus is present, the amount of S. epidermidis dramatically decreases. It is also present on human skin and mucosa. It may form biofilms to attach securely to the epithelial cells in the nasal passageway. The S. epidermidis has lysostaphin in the peptidoglycan that can prevent it from lysis. The peptidoglycan is connected to the teichoic acids by covalent bonds. S. epidermidis has glycerol teichoic acid glucosyl residues which makes it differ from S. aureaus bacteria. S. epidermidis can use glucose anaerobically , but most strains make acetoin, phosphatase and reduce nitrate. All strains can produce acid when exposed to sugar, except a couple of sugars like mannitol, when oxygen is present.(25) The minimum water activity is .85 for growth. (19) | ''[[Staphylococcus epidermidis]]'' with Corynebacteria predominantly colonizes the upper respiratory tract, especially the nostrils. ''S. epidermidis'' covers 90%-100% staphylococci from the nasal cavity when ''S. aureus'' is not present. When ''S. aureus'' is present, the amount of ''S. epidermidis'' dramatically decreases. It is also present on human skin and mucosa. It may form biofilms to attach securely to the epithelial cells in the nasal passageway. The ''S. epidermidis'' has lysostaphin in the peptidoglycan that can prevent it from lysis. The peptidoglycan is connected to the teichoic acids by covalent bonds. ''S. epidermidis'' has glycerol teichoic acid glucosyl residues which makes it differ from ''S. aureaus'' bacteria. ''S. epidermidis'' can use glucose anaerobically , but most strains make acetoin, phosphatase and reduce nitrate. All strains can produce acid when exposed to sugar, except a couple of sugars like mannitol, when oxygen is present.(25) The minimum water activity is .85 for growth. (19) | ||
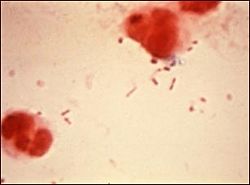
[[Image:Corynebacterium diptheriae.jpg|thumb|right|250px | Corynebacterium diptheriae -picture from [http://phil.cdc.gov/phil/ Public Health Image Library ]]] | [[Image:Corynebacterium diptheriae.jpg|thumb|right|250px | ''Corynebacterium diptheriae'' -picture from [http://phil.cdc.gov/phil/ Public Health Image Library ]]] | ||
[[Corynebacterium]] is a Gram-positive normal flora in the nose. The Corynebacterial envelop is made up of peptidoglycan, arabinogalactan, corynemycloic and corynemycolenic acids, trehalose dimycolates, and phosphatides of mannose and inositol. The lipoidal antigens on the cell surface makes it invasive to the host's immune system, but it doesn't allow the bacteria to attach firmly to the surface of the nares. The Corynebacterial are facultatively aerobic organisms. They ferment glucose for energy, but they are unable to use maltose or galactose. They have granules of long-chain polyphosphate that stores phosphate and will be used as energy in stressful times.(27) | [[Corynebacterium]] is a Gram-positive normal flora in the nose. The Corynebacterial envelop is made up of peptidoglycan, arabinogalactan, corynemycloic and corynemycolenic acids, trehalose dimycolates, and phosphatides of mannose and inositol. The lipoidal antigens on the cell surface makes it invasive to the host's immune system, but it doesn't allow the bacteria to attach firmly to the surface of the nares. The Corynebacterial are facultatively aerobic organisms. They ferment glucose for energy, but they are unable to use maltose or galactose. They have granules of long-chain polyphosphate that stores phosphate and will be used as energy in stressful times.(27) Most species of Corynebacterium will not cause diseases in humans; however, there is a specific species that is highly infectious. The ''[[Corynebacterium diphtheriae]]'' causes infection in the upper respiratory tract, and can be deadly if untreated. (2) | ||
Another Gram-positive bacterium that lives in the human nose is the [[Staphylococcus aureus]], often referred to as staph. It is carried either on the skin or in the nose of healthy people, but 25% - 30% of the population is populated in the nose. The optimum pH for the | Another Gram-positive bacterium that lives in the human nose is the ''[[Staphylococcus aureus]]'', often referred to as staph. It is carried either on the skin or in the nose of healthy people, but 25% - 30% of the population is populated in the nose. The optimum pH for the ''Staphylococcus'' to live in is 7.0-7.5, and the optimum temperature is 30-37 degree Celsius. (19) The minimum water activity Staph needs to survive is .85. While Staph is growing, it will not cause any infection, until the bacteria can enter a wound. It cause an infection once it enters a wound because it has the ability to bind to fibrinogen, which is needed to form blood clots, just like ''Staphylococcus epidermidis''.(28) Stap contains a high concentration of salt that inhibits other bacteria and it has the ability to ferment mannitol, a sugar, as a source of energy. (19)''S. aureus'' did not attach to mucus-producing airway epithelium but to basolateral plasma membrane of columnar cells, to basal cells, and to the basement membrane. (1) | ||
Micrococcus luteus is another Gram positive, spherical, bacterium that also resides in the nose as well as the mouth, skin and upper resipratory tract as an obligate aerobe. M. luteus is normally harmless except for those that have compromised immunities. M. luteus is resistant to reduced water potential that is found in mucus and can tolerate drying and high salt concentrations were the nasal cavity to dry up. | ''[[Micrococcus luteus]]'' is another Gram positive, spherical, bacterium that also resides in the nose as well as the mouth, skin and upper resipratory tract as an obligate aerobe. ''M. luteus'' is normally harmless except for those that have compromised immunities. ''M. luteus'' is resistant to reduced water potential that is found in mucus and can tolerate drying and high salt concentrations were the nasal cavity to dry up. | ||
Diseased: | Diseased: | ||
The nasal passages, being as large as it is (from a microbe's standpoint), can harbor many types of bacteria, viruses, and fungi which can often lead to infection. It is in fact the main site for different organisms to lodge and multiply. One very commonly found gram-positive bacteria is the [[Staphylococcus epidermidis]] which colonizes in the anterior naris. (11)It lives naturally on the skin and mucous membranes. Their grape-like appearance when viewed under the microscope only measures approximately 1-micrometer in diameter. This bacteria, if environmental conditions are optimal, will form biofilms to aggregate more securely. A three stage process of the exopolysaccharide casing of the biofilm provides excellent protection against the environment and phagocytosis by their host's immune system as they seek to mature and eventually dissolute from the colony. The slime (biofilm), mainly composed of teichoic acid and typically found on the cell wall of these microbes can also protect them against antibiotics making them very difficult to treat. This unique ability of the Staphylococcus epidermidis to form a biofilm in the nasal passages may be the reason for their strong virulence. A patient's inability to rid of S. epidermis due to its protective biofilm usually leads to infection.(13) | The nasal passages, being as large as it is (from a microbe's standpoint), can harbor many types of bacteria, viruses, and fungi which can often lead to infection. It is in fact the main site for different organisms to lodge and multiply. One very commonly found gram-positive bacteria is the ''[[Staphylococcus epidermidis]]'' which colonizes in the anterior naris. (11)It lives naturally on the skin and mucous membranes. Their grape-like appearance when viewed under the microscope only measures approximately 1-micrometer in diameter. This bacteria, if environmental conditions are optimal, will form biofilms to aggregate more securely. A three stage process of the exopolysaccharide casing of the biofilm provides excellent protection against the environment and phagocytosis by their host's immune system as they seek to mature and eventually dissolute from the colony. The slime (biofilm), mainly composed of teichoic acid and typically found on the cell wall of these microbes can also protect them against antibiotics making them very difficult to treat. This unique ability of the ''Staphylococcus epidermidis'' to form a biofilm in the nasal passages may be the reason for their strong virulence. A patient's inability to rid of ''S. epidermis'' due to its protective biofilm usually leads to infection.(13) | ||
The [[Streptococcus pneumoniae]] bacteria is another Gram-positive bacteria that is commonly found in the nasal passages, primarily in a patient with acute sinusitis. This lancet-shaped bacteria, approximately 0.5 - 1.25 micrometers in diameter, is one of the primary causes of pneumonia. Although they are also found in the upper respiratory tract of healthy individuals, they are usually the cause of sinus infection when a small amount of this bacteria is lodged in the sinus cavities such as the ethmoid or maxillary sinuses, typically by the force of a sneeze or the blowing of the nose. They are mostly found in pairs (diplococci), but can sometimes be seen alone or in short chains. (12) | The ''[[Streptococcus pneumoniae]]'' bacteria is another Gram-positive bacteria that is commonly found in the nasal passages, primarily in a patient with acute sinusitis. This lancet-shaped bacteria, approximately 0.5 - 1.25 micrometers in diameter, is one of the primary causes of pneumonia. Although they are also found in the upper respiratory tract of healthy individuals, they are usually the cause of sinus infection when a small amount of this bacteria is lodged in the sinus cavities such as the ethmoid or maxillary sinuses, typically by the force of a sneeze or the blowing of the nose. They are mostly found in pairs (diplococci), but can sometimes be seen alone or in short chains. (12) | ||
The S. pneumoniae has an extremely thick cell wall, approximately six layers compose of peptidoglycan with teichoic acid. This teichoic acid has two choline residues that bind specifically to choline-binding receptors on human cells. Its capsule, composed of polysaccharides prevents phagocytosis of the bacteria. The pili structures on some strains of S. pneumoniae have been identified in the involvement of colonization in the nasal passages. (12) This allows them to gain a strong attachment to epithelial cells and sometimes leads to a challenging problem if left untreated. | The ''S. pneumoniae'' has an extremely thick cell wall, approximately six layers compose of peptidoglycan with teichoic acid. This teichoic acid has two choline residues that bind specifically to choline-binding receptors on human cells. Its capsule, composed of polysaccharides prevents phagocytosis of the bacteria. The pili structures on some strains of ''S. pneumoniae'' have been identified in the involvement of colonization in the nasal passages. (12) This allows them to gain a strong attachment to epithelial cells and sometimes leads to a challenging problem if left untreated. | ||
[[Image:H. influenza.jpg|thumb|right|250px | Haemophilus influenzae -picture from [http://www.nlm.nih.gov/ MedlinePlus]]] | [[Image:H. influenza.jpg|thumb|right|250px | ''Haemophilus influenzae'' -picture from [http://www.nlm.nih.gov/ MedlinePlus]]] | ||
[http://microbewiki.kenyon.edu/index.php/Haemophilus_influenzae | [http://microbewiki.kenyon.edu/index.php/''Haemophilus_influenzae''] is a Gram-negative, rod-shaped bacterium that resides in the nasopharnyx region of the human nasal passage. They lack motility due to the absence of a flagella or pili. Its length is about 1.0 x 0.3 um. There are 6 strains of encapsulated ''H. influenzae'', which are categorized based on the type of polysaccharide capsule. The differences are denoted a through f, with ''H. influenzae'' serotype b (Hib), as the most commonly vaccinated strain. This vaccination helps in the prevention of invasive ''H. influenzae'' disease in young children. However, there also exists a non-encapsulated strain referred to as non-typeable ''H. influenzae'' (NTHi) which is unaffected by the vaccine due to lacking an antigenic capsule. (14) Virulance of this bacterial strain is based in large part to the lipopolysaccharide (LPS) component of its outer membrane. (29) The LPS is an endotoxin and is composed of varying elements of monosaccharides, such as L-glycero-D-manno heptose, D-Glc, D-Gal, and sialic acid (Neu5Ac), which provide added protection against chemical attack and an increase the ability to cause disease. NThi usually infects the upper and lower respiratory tracts leading to pneumonia, sinusitis, and otitis media, which is an infection of the middle ear. Its encapsulated counterpart, specifically Hib and Hif, can cause meningitis and bacteremia, usually occurring in 3rd world countries where children are unvaccinated. (14) | ||
== == | == == | ||
There are many different microbes that either reside or just pass through the nasal passages, most of which impact the health of their host. Those microbes that have such an impact are listed and briefly described below. | There are many different microbes that either reside or just pass through the nasal passages, most of which impact the health of their host. Those microbes that have such an impact are listed and briefly described below. | ||
{| | {| | ||
| align="center" style="background:#f0f0f0;"|'''Microbial Species''' | | align="center" style="background:#f0f0f0;"|'''Microbial Species''' | ||
| align="center" style="background:#f0f0f0;"|'''Description of Microbe''' | | align="center" style="background:#f0f0f0;"|'''Description of Microbe''' | ||
|- | |- | ||
| Moraxella catarrhalis || (formerly Branhammella catarrhalis) Gram-negative bacteria which are found in mucous membranes, can be opportunistic. Cells are non-motile, short rods/cocci found individually or in pairs. Optimum at 33-36 degrees celsius | | ''Moraxella catarrhalis'' || (formerly Branhammella catarrhalis) Gram-negative bacteria which are found in mucous membranes, can be opportunistic. Cells are non-motile, short rods/cocci found individually or in pairs. Optimum at 33-36 degrees celsius | ||
|- | |- | ||
| Eikenella corrodens || Gram-negative bacteria, anaerobic, faculatively aerobic, can be an opportunistic pathogen. Cells are non-motile, round-ended rods which may exhibit twitching motility. Reduces nitrate to nitrite. | | ''Eikenella corrodens'' || Gram-negative bacteria, anaerobic, faculatively aerobic, can be an opportunistic pathogen. Cells are non-motile, round-ended rods which may exhibit twitching motility. Reduces nitrate to nitrite. | ||
|- | |- | ||
| | | ''Streptococcus pyogenes'' || Gram-positive bacteria, asporogenous, facultatively anaerobic. Cells are non-motile, typically 1-micrometer, generally found in pairs or chain. Fermentative with carbohydrates metabolized anaerogenically and homofermentatively. Optimum at 30-37 degrees Celsius. | ||
|- | |- | ||
| | | Arcanobacterium || Genus of asporogenous bacteria, with wall type VI. They initially grow as irregular rod shapes and may eventually become granular and segmented. Growth primarily occurs through anaerobic or aerobic processes which can be enhanced by serum or blood and even increased pressures in CO2 | ||
|- | |- | ||
| | | ''Chlamydia pneumoniae'' || Cause of acute respiratory infection, associated with subacute respiratory disease. Chronic infection and re-infection can lead to severe disease involving immunologically-based pathogenesis. | ||
|- | |- | ||
| | | Rhinovirus || Genus of viruses from the family Picornaviridae, which infect the upper respiratory tract. They are the primary cause of the common cold as they can propagate in many types of human cells. Has the ability to withstand freezing temperatures, but is optimal at 33 degrees Celsius. | ||
|- | |||
| | |||
|} | |||
(28) | |||
===Are there any other non-microbes present?=== | ===Are there any other non-microbes present?=== | ||
| Line 105: | Line 109: | ||
Diseased: | Diseased: | ||
Fungal infection are not very common in the nasal passages, however, there have been cases in which patients that are immune-suppressed have experienced mycosis. Patients with uncontrolled diabetes or those with acquired immunodeficiency syndrome (AIDS) are typically a target for either Phycomycetes or [[Aspergillus]]. Other types of mycotic pathogens also infect humans, but are more uncommon. The fungal pathogens that usually invade the nasal passages are saprophytes which are found in soils and on plants, thriving in high glucose and acidic environments. As aspergillosis originates in the nose and paranasal sinuses it can invade the brain and vascular structures via arterial wall invasion causing tissue necrosis and arterial thrombosis. The aspergillus and bipolaris species can illicit an allergic response in the sinuses leading to chronic progressive inflammatory response which causes bone expansion and even bone destruction. Aeration and irrigation of the sinuses with a topical antifungal agent are treatments that may speed up the recovery process. (11) | Fungal infection are not very common in the nasal passages, however, there have been cases in which patients that are immune-suppressed have experienced mycosis. Patients with uncontrolled diabetes or those with acquired immunodeficiency syndrome (AIDS) are typically a target for either ''Phycomycetes'' or ''[[Aspergillus]]''. Other types of mycotic pathogens also infect humans, but are more uncommon. The fungal pathogens that usually invade the nasal passages are saprophytes which are found in soils and on plants, thriving in high glucose and acidic environments. As aspergillosis originates in the nose and paranasal sinuses it can invade the brain and vascular structures via arterial wall invasion causing tissue necrosis and arterial thrombosis. The ''aspergillus'' and ''bipolaris'' species can illicit an allergic response in the sinuses leading to chronic progressive inflammatory response which causes bone expansion and even bone destruction. Aeration and irrigation of the sinuses with a topical antifungal agent are treatments that may speed up the recovery process. (11) | ||
===Do the microbes that are present interact with each other?=== | ===Do the microbes that are present interact with each other?=== | ||
The reason only 25% - 30% of the nasal passageway is populated by the | The reason only 25% - 30% of the nasal passageway is populated by the ''S. aureus'' is beacuse ''S. epidermidis'' and Corynebacterium have a negative symbiosis behavior with the ''S. aureus''. Some possible ways that the bacteria compete with one another is through the synthesis of bacteriocins, bacteriolytic enzymes, etc. or the competition of specific attachment to epithelial cells. There are ''S. aureus'' that produces some bactericiocin agains some Corynebacterium speices and ''S. epidermidis'' bacteriocin against ''S. aureus'', but there is no bactericiocin produced by corynebacteria against the other two bacteria. Binding to the epithelial cells involves the carbohydrate portion of the human nasal mucin support. The Corynebacterium has a higher affinity for mucus than ''S. aureus'' and ''S. aureus'' has a higher affinity for than ''S. epidermidis''. Corynebacterium specifically inhibts the colonization of ''S. aureus'' but not ''S. epidermidis''. (1) | ||
Competition for mucosal surface in the nasopharyngeal region exists between Streptococcus pneumoniae and Haemophilus influenza. These bacterial species compete for limited space in order to form stable colonies and propagate. Both will employ forms of microbial interference to exert their dominance over the opposition. S. pneumoniae, through neuramindase, has the ability to cleave terminal sialic acid residues. It will utilize this strategy to strip off sialic acid from the lipopolysaccharide component of H. | Competition for mucosal surface in the nasopharyngeal region exists between ''Streptococcus pneumoniae'' and ''Haemophilus influenza''. These bacterial species compete for limited space in order to form stable colonies and propagate. Both will employ forms of microbial interference to exert their dominance over the opposition. ''S. pneumoniae'', through neuramindase, has the ability to cleave terminal sialic acid residues. It will utilize this strategy to strip off sialic acid from the lipopolysaccharide component of ''H. infuenzae''’s outer membrane thereby compromising its ability to withstand chemical attack. During the weakened state of its rival, ''S. pneumoniae'' will deliver the final blow by generating high levels of hydrogen peroxide via aerobic metabolism, which on contact, is lethal to ''H. influenza''. However, even in the face of such awesome firepower, it is ''H. influenzae'' that wins out. ''H. influenza'' relies on the inflammatory response of the local host to get rid the competition. Although exact details are still being researched, ''H. influenzae'' has the ability to recruit the host responder, neutrophils. Neutrophils are a type of white blood cell that is capable of getting rid of ''S. pneumoniae'' and other microorganisms via phagocytosis. Due to its capsule, ''H. influenzae'' is able to avoid suffering the same fate as its rival. Once the competition is eliminated, ''H. influenzae'' is free to proliferate and infect the upper respiratory tract of its host. Conversely, when taking into consideration the application of vaccines and antimicrobials, these factors can also influence bacterial interspecies behavior and the outcome of the competition between them. (26) | ||
===Do the microbes change their environment?=== | ===Do the microbes change their environment?=== | ||
The simple presence of a bacteria can change the environment in the nasal passages if it is identified by the host's immune system. The peptidoglycan of the bacterial cell wall in a | The simple presence of a bacteria can change the environment in the nasal passages if it is identified by the host's immune system. The peptidoglycan of the bacterial cell wall in a penicillin resistant pneumococci is an essential and immunologically important aspect of the bacterial structure, consisting of repeating N-acetylgucosamine and N-acetyl muramic acid. The insoluble network of peptidoglycan induces the production of cytokines, accumulation of edema fluid and recruitment of leukocytes. The breakdown of the cell wall, however, causes this bioactivity to decrease. It is suggested that a receptor (TLR-2 receptor) recognizes the cell wall (peptidoglycan) of the bacteria and initiates an inflammatory response. An enormous response by various cells including macrophages, astrocytes, microglia, epithelial cell and endothelial cells have been noted by the presence alone of a bacterial cell wall. (18) | ||
Staphylococcus aureus produces an enzyme called coagulase that changes fibrinogen to fibrin, thus clotting blood. Coagulase is bound tightly to the microbe's surface and reacts upon encountering blood. The fibrin is then coated around S. aureaus. It is believed that it helps the microbe resist phagocytosis, allowing it to become more virulent. | ''Staphylococcus aureus'' produces an enzyme called coagulase that changes fibrinogen to fibrin, thus clotting blood. Coagulase is bound tightly to the microbe's surface and reacts upon encountering blood. The fibrin is then coated around S. aureaus. It is believed that it helps the microbe resist phagocytosis, allowing it to become more virulent. | ||
Streptococcus pneumoniae also has the ability of binding to epithelial cells by use of enzymes. They secrete an enzyme called pneumolysin which is thiol activated. Evidence suggests that in large quantity, this enzyme is toxic for epithelial ciliated epithelium and results in ciliostaticity in lower doses. This enzyme can also render bacteriocidal activity of phagocytes creating an extension of stay in the host for the bacteria. (21) | ''Streptococcus pneumoniae'' also has the ability of binding to epithelial cells by use of enzymes. They secrete an enzyme called pneumolysin which is thiol activated. Evidence suggests that in large quantity, this enzyme is toxic for epithelial ciliated epithelium and results in ciliostaticity in lower doses. This enzyme can also render bacteriocidal activity of phagocytes creating an extension of stay in the host for the bacteria. (21) | ||
===Do the microbes carry out any metabolism that affects their environment?=== | ===Do the microbes carry out any metabolism that affects their environment?=== | ||
S. pneumoniae obtains energy through fermentation of sugars producing lactic acid as a side product. It breaks down large carbohydrate molecules in order to obtain the energy required for growth. Moreover, S. pneumonia produces hydrogen peroxide during pyruvate metabolism in aerobic growth. Hydrogen peroxide in high concentration is lethal towards competing bacteria in the surrounding area. For instance, hydrogen peroxide can hinder the growth of M. catarrhalis as well as H. influenzae. It is believed that S. pneumonia employs this type of microbial interference in order to out-compete other microbes for the limited mucousal surface necessary to form stable colonies. (26) | All bacteria listed in the table above that reside in the nasal passages conduct some degree of metabolism in order to obtain nutrients, intermediates for biosynthesis, and energy, all of which is necessary to sustain itself. For example, ''S. pneumoniae'' obtains energy through fermentation of sugars producing lactic acid as a side product. It breaks down large carbohydrate molecules in order to obtain the energy required for growth. Moreover, ''S. pneumonia'' produces hydrogen peroxide during pyruvate metabolism in aerobic growth. Hydrogen peroxide in high concentration is lethal towards competing bacteria in the surrounding area. For instance, hydrogen peroxide can hinder the growth of ''M. catarrhalis'' as well as ''H. influenzae''. It is believed that ''S. pneumonia'' employs this type of microbial interference in order to out-compete other microbes for the limited mucousal surface necessary to form stable colonies. (26) | ||
==Current Research== | ==Current Research== | ||
===A Nitric Oxide–Inducible Lactate Dehydrogenase Enables Staphylococcus aureus to Resist Innate Immunity=== | ===A Nitric Oxide–Inducible Lactate Dehydrogenase Enables ''Staphylococcus aureus'' to Resist Innate Immunity=== | ||
As previously mentioned, Staphylococcus aureus is found in the nose of about 25% - 30% of the human population. Researchers from the University of Washington were interested in finding out why this bacterium is able to survive the human's natural production of nitric oxide in the nasal passages. This production of nitric oxide in the nose and nasal passages usually protects against disease causing bacteria by preventing their respiration process. These researchers found out that | As previously mentioned, ''Staphylococcus aureus'' is found in the nose of about 25% - 30% of the human population. Researchers from the University of Washington were interested in finding out why this bacterium is able to survive the human's natural production of nitric oxide in the nasal passages. This production of nitric oxide in the nose and nasal passages usually protects against disease causing bacteria by preventing their respiration process. These researchers found out that ''S. aureus'' produces lactic acid in the presence of nitric oxide,making a chemical balance, allowing it to continue to grow in this type of environment. The researchers then found a way to remove the lactic acid production by ''Staphylococcus aureus'' and found that it was then not able to survive in the presence of nitric oxide. This was tested in mice and the researchers also found that there were no diseases caused by the modified bacterium. The researchers hope to use this type of modification to find new ways to prevent the survival of such bacteria without the use of antibiotics.(3) | ||
===Differential Roles of Surface Polysaccharide and Extracellular DNA in Staphylococcus aureus and Staphylococcus epidermidis Biofilms=== | ===Differential Roles of Surface Polysaccharide and Extracellular DNA in ''Staphylococcus aureus'' and ''Staphylococcus epidermidis'' Biofilms=== | ||
Scientists researched the "functions of two staphylo9coccal biofilm matrix polymers: poly-N-acetylglucosamine surface polysaccharide (PNAG) and extracellular DNA (ecDNA)" and how the "PNAG-degrading enzyme, dispersin B, and DNase I inhibit biofilm formation, detach preformed biofilms, and sensitize biofilms to killing by the cationic detergent cetylpyridinium chloride (CPC)." The biofilms will help protect the bacteria from being nullified by antibiotics and host defenses. The scientists found that both dispersin B and DNase I will inhibit biofilm formation in S. aureus and PNAG-positive S. epidermidis strains. Dispersin B will efficiently and rapidly detach S. epidermidis biofilms, but not S. aureus. On the other hand, DNase I will cause separation of the biofilm and the surface in S. aureus, but not S. epidermidis. PNAG is a major matrix component of only S. epidermidis biofilm cells, but it is produced by both bacteria. The PNAG performs different functions in the biofilms of the two bacteria. The PNAG protects the S. epidermidis cells from CPC killing, while the PNAG works in early stages of S. aureus biofilms, which makes it resistant to the detachment of dispersin B. Overall, ecDNA and PNAG can be "general diffusion barriers" that stop detergents from killing the bacteria.(7) | Scientists researched the "functions of two staphylo9coccal biofilm matrix polymers: poly-N-acetylglucosamine surface polysaccharide (PNAG) and extracellular DNA (ecDNA)" and how the "PNAG-degrading enzyme, dispersin B, and DNase I inhibit biofilm formation, detach preformed biofilms, and sensitize biofilms to killing by the cationic detergent cetylpyridinium chloride (CPC)." The biofilms will help protect the bacteria from being nullified by antibiotics and host defenses. The scientists found that both dispersin B and DNase I will inhibit biofilm formation in ''S. aureus'' and PNAG-positive ''S. epidermidis'' strains. Dispersin B will efficiently and rapidly detach ''S. epidermidis'' biofilms, but not ''S. aureus''. On the other hand, DNase I will cause separation of the biofilm and the surface in ''S. aureus'', but not ''S. epidermidis''. PNAG is a major matrix component of only ''S. epidermidis'' biofilm cells, but it is produced by both bacteria. The PNAG performs different functions in the biofilms of the two bacteria. The PNAG protects the ''S. epidermidis'' cells from CPC killing, while the PNAG works in early stages of ''S. aureus'' biofilms, which makes it resistant to the detachment of dispersin B. Overall, ecDNA and PNAG can be "general diffusion barriers" that stop detergents from killing the bacteria.(7) | ||
===Isolation and Molecular Characterization of Methicillin-Resistant Coagulase-Negative Staphylococci from Nasal Flora of Healthy Humans=== | ===Isolation and Molecular Characterization of Methicillin-Resistant Coagulase-Negative ''Staphylococci'' from Nasal Flora of Healthy Humans=== | ||
Researchers form Cambridge University have isolated "methicillin-resistant coagulase negative staphylcocci (MRCNS) from the nasal flora of healthy humans" from three places in Rio de Janeiro City. They obtained swaps from the nares of the adults at two military quarters and students from a public school. Staphylcocci were isolated and "tested for the presence of the mecA gene" by hybridizing the gene with a specific probe. S. epidermidis was the most common MRCNS; it accounted for 38 out of the 45 total. The SmaI-digested DNA was also put through pulsed-field gel electrophoresis in order to study the | Researchers form Cambridge University have isolated "methicillin-resistant coagulase negative staphylcocci (MRCNS) from the nasal flora of healthy humans" from three places in Rio de Janeiro City. They obtained swaps from the nares of the adults at two military quarters and students from a public school. ''Staphylcocci'' were isolated and "tested for the presence of the mecA gene" by hybridizing the gene with a specific probe. ''S. epidermidis'' was the most common MRCNS; it accounted for 38 out of the 45 total. The SmaI-digested DNA was also put through pulsed-field gel electrophoresis in order to study the clonality of the MRSE ''S. epidermidis''. It appears that the cross-colonization contributed to the spread of the methicillin-resistance. The wide and diverse genome suggests that the spread of the mecA gene among the isolates were probably through horizontal transmission. It was concluded that though it was researched with only three institutions, it reflects how other communities in Rio may have gained methicillin resistance. (17) | ||
===Evaluation of Alternaria alternata for Biological Control of Amaranthus retroflexus=== | ===Evaluation of Alternaria alternata for Biological Control of ''Amaranthus retroflexus''=== | ||
Researchers from Aberdeen University in Scotland found promising evidence that Alternaria alternata, a fungal allergen that can be found in the nasal passages, can hinder the growth of herbicide-resistant Amaranthus retroflexus, a weed known to hinder the yield of various crops in agriculture. Working in a controlled setting, these scientists were able to garner 100% mortality rate in A. | Researchers from Aberdeen University in Scotland found promising evidence that Alternaria alternata, a fungal allergen that can be found in the nasal passages, can hinder the growth of herbicide-resistant ''Amaranthus retroflexus'', a weed known to hinder the yield of various crops in agriculture. Working in a controlled setting, these scientists were able to garner 100% mortality rate in ''A. retroflexus'' upon exposure to an ''A. alternata'' spore concentration of 10^7 spores ml^-1. The scientist prepared the spores by culturing ''A. alternata'' in a V-8 agar media that was allowed to incubate for 2-3 weeks. The harvested spores that were formulated in an oil emulsion produced the highest ''A. retroflexus'' mortality rate when inoculated at the four-leaf stage under the optimum post-dew temperature of 20-30 degrees for a 24 hour dew period. Furthermore, linear regression analysis showed rapid disease development and necrosis of the leaf area in ''A. retroflexus'' within 12 hours of exposure to the ''A. alternata spores''. However, using ''A. alternata'' as a mycoherbicide requires further study due to the variability in actual field conditions. Regardless, the result of this study opens the door for safer and more effective alternatives for weed control, especially with the growing concerns over the environment and the health effects of consuming foods with herbicide residue. (16) | ||
===Local Pathogenic Bacteria in Allergic Rhinitis=== | ===Local Pathogenic Bacteria in Allergic Rhinitis=== | ||
Swiss scientists examined whether subjects’ allergic reactions affected the presence of potential pathogenic bacteria (PPB) that could be found in the nasal cavity. There is a variety of PPB which may include Staphylococcus aureus and Haemophilus influenzae among many. The researchers took a group of random men and women and took swabs from their nasal passageways. Skin tests for numerous allergens along with control tests were run for these subjects. They found that 15% of the subjects tested positive for skin tests for being allergic, ranging from high sensitivity to moderate sensitivity including sneezing, nasal itching, running nose, and increased nasal airflow resistance. Furthermore, the scientists found that about 90% of the positive subjects had PPB in their nasal passageways! On the other hand, only 36% of the negative subjects (who were not allergic) had PPB in their nasal cavities. In addition, it was found that the sensitized patients had more chance of having more than one PPB species in their nasal cavity. Although there is still much to be examined, the conclusion of this study is that subjects who test positive to aeroallergen skin tests have a higher chance of having nasal PPB, which indicates that PPB may be involved in allergic rhinitis. (19) | Swiss scientists examined whether subjects’ allergic reactions affected the presence of potential pathogenic bacteria (PPB) that could be found in the nasal cavity. There is a variety of PPB which may include ''Staphylococcus aureus'' and ''Haemophilus influenzae'' among many. The researchers took a group of random men and women and took swabs from their nasal passageways. Skin tests for numerous allergens along with control tests were run for these subjects. They found that 15% of the subjects tested positive for skin tests for being allergic, ranging from high sensitivity to moderate sensitivity including sneezing, nasal itching, running nose, and increased nasal airflow resistance. Furthermore, the scientists found that about 90% of the positive subjects had PPB in their nasal passageways! On the other hand, only 36% of the negative subjects (who were not allergic) had PPB in their nasal cavities. In addition, it was found that the sensitized patients had more chance of having more than one PPB species in their nasal cavity. Although there is still much to be examined, the conclusion of this study is that subjects who test positive to aeroallergen skin tests have a higher chance of having nasal PPB, which indicates that PPB may be involved in allergic rhinitis. (19) | ||
===Staph Bacteria are Prolific Gene Swappers | ===Staph Bacteria are Prolific Gene Swappers=== | ||
According to scientists from the National Institute of Allergy and Infectious Diseases (NIAID), “when some disease-causing bacteria encounter a new obstacle, they simply readily swap DNA with their relatives to acquire the genes needed to overcome it. Staphylococcus aureus is the common “staph” bacterium responsible for several human diseases and had adapted itself to many different environments.” This research gives a new approach to antibiotics and vaccine design as it gives the solution to the problem of toxic shock syndrome and antibiotic- resistance infections. “Bacteria can easily become dangerous. S. aureus is a common microbe that often causes no illness. Some strains can cause diseases, however, including TSS, food poisoning and impetigo. The bacteria can infect the skin, blood, urinary tract and wounds, and are a common source of infections acquired in hospitals. Most people are unknowing S. aureus carriers, intermittently harboring the bacteria on their skin or in their nose and throat, even in the absence of illness. A technique called DNA microarray analysis was used to rapidly screen their samples. Upon analyzing the results, the researchers discovered nearly a fourth of the genome was dispensable, consisting of genes that were not required for the bacteria's basic life processes. These so-called contingency genes provide flexibility in the bacterium's ability to cause disease in humans, cows and other organisms.” These bacteria are very rapid in adapting to the changes by picking up other genes which helps them spread through a large population.(22) | According to scientists from the National Institute of Allergy and Infectious Diseases (NIAID), “when some disease-causing bacteria encounter a new obstacle, they simply readily swap DNA with their relatives to acquire the genes needed to overcome it. ''Staphylococcus aureus'' is the common “staph” bacterium responsible for several human diseases and had adapted itself to many different environments.” This research gives a new approach to antibiotics and vaccine design as it gives the solution to the problem of toxic shock syndrome and antibiotic- resistance infections. “Bacteria can easily become dangerous. ''S. aureus'' is a common microbe that often causes no illness. Some strains can cause diseases, however, including TSS, food poisoning and impetigo. The bacteria can infect the skin, blood, urinary tract and wounds, and are a common source of infections acquired in hospitals. Most people are unknowing S. aureus carriers, intermittently harboring the bacteria on their skin or in their nose and throat, even in the absence of illness. A technique called DNA microarray analysis was used to rapidly screen their samples. Upon analyzing the results, the researchers discovered nearly a fourth of the genome was dispensable, consisting of genes that were not required for the bacteria's basic life processes. These so-called contingency genes provide flexibility in the bacterium's ability to cause disease in humans, cows and other organisms.” These bacteria are very rapid in adapting to the changes by picking up other genes which helps them spread through a large population.(22) | ||
==Conclusion== | ==Conclusion== | ||
Although the nose is a very small part of our body, it is still very important for us to function and stay healthy. It plays some major roles in protecting our body from microbes that might be infectious to us. On the other hand, it can also be the starting point of some allergies or major diseases like asthama which are very difficult to treat especially if it reaches its chronic state. We don't always remember to protect our airways when we work in the garden, use aerosols in the kitchen or even when pollen levels are high, but we must understand that a little effort to protect our nasal passages can go a long way. We must remember to take care of our nasal passageways in order to live a long healthy life, full of love and happiness. | |||
==References== | ==References== | ||
| Line 202: | Line 205: | ||
24. [http://mmbr.asm.org/cgi/reprint/49/2/126?view=long&pmid=2989672 Parisi, Joseph. “Coagulase-Negative Staphylococci and the Epidemiological Typing of Staphylococcus epidermidis”. Microbiological Reviews. 1985. Volume 49. p. 126-139. ] | 24. [http://mmbr.asm.org/cgi/reprint/49/2/126?view=long&pmid=2989672 Parisi, Joseph. “Coagulase-Negative Staphylococci and the Epidemiological Typing of Staphylococcus epidermidis”. Microbiological Reviews. 1985. Volume 49. p. 126-139. ] | ||
[http://www.ncbi.nlm.nih.gov/pubmed/16201010 | [http://www.ncbi.nlm.nih.gov/pubmed/16201010 25. Lysenko, Elena S, et al. "The Role of Innate Immune Responses in the Outcome of Interspecies Competition for Colonization of Mucosal Surfaces". "PLoS Pathogens". 2005. Vol.1 is.1 p.e1] | ||
26. [http://mmbr.asm.org/cgi/reprint/34/4/378?maxtoshow=&HITS=10&hits=10&RESULTFORMAT=&fulltext=corynebacterium&searchid=1&FIRSTINDEX=0&resourcetype=HWCIT Barksdale, Lane. "Corynebacterium diphtheriae and Its Relatives". Microbiological Reviews. 1970. Volume 34. No. 4. p 383, 395-397.] | |||
27. [http://mmbr.asm.org/cgi/content/full/63/1/174?maxtoshow=&HITS=10&hits=10&RESULTFORMAT=&fulltext=Staphylococcus+aureus+&searchid=1&FIRSTINDEX=10&resourcetype=HWCIT#SEC9_14 Navarre, W., Schneewind, O. "Surface Proteins of Gram-Positive Bacteria and Mechanisms of Their Targeting to the Cell Wall Envelope". Microbiology and Molecular Biology Reviews. 1999. Vol. 63, No. 1. p. 205-6] | |||
28. Singleton, Paul. Diana Sainsbury. Dictionary of Microbiology and Molecular Biology. 3rd Edition Revised. West Sussex, England. John Wiley & Sons, Ltd. 2006. | |||
[http://www.jstor.org/stable/3148319 29. Bouchet, V., Hood, D., Li, J., Brisson, J, et al. “Host-Derived Sialic Acid Is Incorporated into Haemophilus influenzae Lipopolysaccharide and Is a Major Virulence Factor in Experimental Otitis Media”. Proceedings of the National Academy of Sciences of the United States of America. 2003. Vol. 100, No. 15 p. 8898-8903] | |||
Edited by Jacinda Chen , Wayne Chen , Josephe Dalidi , Jennifer Hao , Rutu Kothari , Nidhi Patel , Natividad Rodriguez , Prudencio Sy, students of [mailto:ralarsen@ucsd.edu Rachel Larsen] | Edited by Jacinda Chen , Wayne Chen , Josephe Dalidi , Jennifer Hao , Rutu Kothari , Nidhi Patel , Natividad Rodriguez , Prudencio Sy, students of [mailto:ralarsen@ucsd.edu Rachel Larsen] | ||
Latest revision as of 20:26, 2 September 2011
Introduction to the Nasal Passageway
The nose is one of the few openings that bacteria have direct access to get inside the body. The nasal passage is important for filtering the air that we breathe in and it also stops tiny foreign particles or microorganisms from entering the body. What many people do not know is that the nose and nasal passages are, or can be , the perfect environment for some bacteria, good and bad. This page will focus on describing what makes the nasal passages such a hospitable environment for the bacteria to grow and live inside the nose.
Description of Nasal Passageway
Location of the Nasal Passageway
The main entry to the nasal passageway is through the nostrils, inside the nose, which is located on the face. From there, the passageway extends to the throat. The nose is the organ of smell located in the middle of the face. The internal part of the nose lies above the roof of the mouth. It is supported by bone and cartilage. The bony part is formed mainly by the nasal bones on each side and the frontal process of the maxillary bone. The nasal cavity is the air passage starting at the nostril (opening of the nose) and ending at the back of the throat(4). Nasal Obstruction is a partial or complete blockage of one or both of these air passages. The nose is one of the few openings of the body for bacteria and microbes to go inside the body.
Physical Conditions of the Nasal Passageway
Normal:
The temperature of the nasal passageway in adults is 34°C. (9) The pressure of the normal passageway should be around 1 atm. There is little known about the pH of the human nasal cavity. The average pH in the anterior of the nose is 6.40. The pH in the posterior of the nasal cavity was 6.27. The overall range in pH was 5.17- 8.13 for the anterior cavity and 5.20 - 8.00 for the posterior cavity. The average baseline human nasal cavity pH is 6.3.(6)
In the nares, the air contains around 21% oxygen and 0.04% carbon dioxide. The oxygen is being absorbed by the epithelial cells which inhibits a gradient in the oxygen content through the mucus. The nares are predominantly an aerobic environment for bacteria to live in. (9)
The nasal passageway walls, and particularly the flap-like middle and inferior nasal conchae, are layered with respiratory mucous membranes secreted by goblet cells. These membranes have many small hair-like cells, known as cilia, that move mucus in waves toward the throat area. Bacteria, along with dust and other particles inhaled from the outside environment are snared by the nasal mucus, carried back out, and dripped into the gastric juices to destroy any possible pathogens. The mucus contains many defensive substances including lysozymes that dissolve and kill the bacteria, lactroferrin, immunoglobulins, and defensins, although some bacteria are not killed by this defensive substance.
Diseased:
As with the normal nasal passageways, little is known about the pH of the diseased niche. But in the infected person, it is known that the pH of the person changes accordingly, due to the presence of the bacterial community.
The physical conditions of nasal passages vary according to the conditions in the nose. Under the infectious conditions like sinusitis the nose might be running or congested and produces a thick fluid. In polyps the airflow is blocked and mucus is not formed anymore. It is one of the causes of sinusitis and leads to the expansion of nasal membrane. This environment results in the secretion of other bacteria. The bacteria also grow due to the change in the atmosphere like dry climate or cold climate, swimming, and air pollution. Cold and flu are suitable atmosphere for the bacteria to grow as they cause congestion, called rhinitis and make it difficult to breathe. The immune system becomes weak and so the bacteria can move faster.
Influence by Adjacent Communities
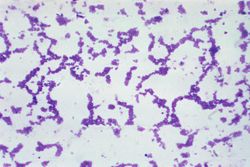
The nasal passageway is close to other niches like the lungs, mouth, and throat. The nasal passage is influenced by the bacteria colonies of Staphylococcus aureus. Other pathogens include such as Haemophilus influenzae, S. pneumonia, Nisseria meningitides, Moraxella catarrhalis and S. aureus. Successful colonization depends not only on the ability of S. aureus to survive host factors but also on coexistence with other bacteria. An airborne bacterium also causes allergies and irritation.
Sinuses: The diseased maxillary and ethmoid sinuses are most commonly associated with affecting the nasal passages by causing inflammation and congestion. One of the diseases caused by the communities of bacteria is sinusitis. The ability of bacteria to infect the sinuses must first be set up by conditions that create a favorable environment in the sinus cavities. The inflammation in the sinuses is chronic do begin with.(5) The causes for such chronic sinusitis cases are sometimes unclear. The Bacteria that causes the sinusitis are Streptococcus pneumonia, H. influenzae, Moraxella catarrhalis. The symptoms of this disease are severe headache, pain or pressure in the areas of the face, cough, and fever. It could also be damaging to the mucous membrane if left untreated. Bipolaris specifera is a fungus that also causes sinus. This fungus is very fast growing and they grow at 25 degrees Celcius. In their growing process they change their shape and color too (23).
Throat: The throat is connected to the nasal passageway and contains aerobic, gram-positive bacteria which are characterized by hemolysis. An example of a pathogenic bacteria in the throat is Streptococcus pyogenes, which can infect when the immune system is down and cause diseases such as scarlet fever and pharyngitis (strep throat) among others. An example of nonpathogenic bacteria in the throat is Streptococcus salivarius which may enter the bloodstream and may cause diseases such as septicemia although not very often. These diseases mostly affect the throat, but may move upwards to cause nasal passageway infections. Sore throat also affects the conditions in the nose by causing post nasal drip.
Bipolaris Specifera: Polyps and fungal diseases have made their way through dura and extended far intracranially, especially in the frontal recess region and the roof of the anterior ethmoid. They obstruct both the nostrils with glassy polyps. Hemotoxylin and eosin (H&E) and Gomoris methenamine silver (GMS) both affect the mucus lining of nasal sinuses. This is a very rare combination of two commonly different diseases found in the same location and caused by the same pathogen, Bipolaris Specifera (23)”.
Conditions under which the environment changes
The environment in which bacteria live varies on the condition of the body temperature and also depends on other bacteria as different bacteria's also affect each other's growth. Anything that might irritate a human's nose, like air pollution, allergies, birth control pills, etc., may cause swelling and blockage of the nasal passageways which will lead to bacterial growth and infection. The trapped mucus within the nasal will create a breeding ground for bacteria. (8)
The temperature of the air will also affect the nasal cavity. The cold air will stimulate an increase in mucus production and thicken the mucus. Sometimes the hot temperature might cause allergies and irritation due to lot of atmospheric pressure. During an infection, inflammation makes the pH of the mucus similar to that of plasma, 7.4. (10)
Sleeping will also affect the nasal cavity by clogging one side of the nasal passageway. When sleeping, one side of the nose is always clogged because of the nasal cycle, which is "normal physiological phenomenon." The nose alternates between phases of congestion and decongestion and it varies between people. The blockage is caused by the swelling and shrinkage of the blood vessels lining inside the nose. (8)
Who lives in the Nasal Passageway?
Which microbes are present in the Nasal Passageway?
Even though we cannot see them with our naked eye, microscopic organisms are living inside our nasal passageways. Although most of these bacteria are non-pathogenic, some may induce illness if they successfully break through the bodies defense systems. Some examples of these non-pathogenic bacteria are Streptococcus, Neisseria, Haemophilus, and Micrococcus. Some of the pathogenic examples include Staphylococcus aureus, Corynebacterium diphtheriae, Streptococcus pneumoniae, and Haemophilus influenzae among others. (15)
Normal:
Staphylococcus epidermidis with Corynebacteria predominantly colonizes the upper respiratory tract, especially the nostrils. S. epidermidis covers 90%-100% staphylococci from the nasal cavity when S. aureus is not present. When S. aureus is present, the amount of S. epidermidis dramatically decreases. It is also present on human skin and mucosa. It may form biofilms to attach securely to the epithelial cells in the nasal passageway. The S. epidermidis has lysostaphin in the peptidoglycan that can prevent it from lysis. The peptidoglycan is connected to the teichoic acids by covalent bonds. S. epidermidis has glycerol teichoic acid glucosyl residues which makes it differ from S. aureaus bacteria. S. epidermidis can use glucose anaerobically , but most strains make acetoin, phosphatase and reduce nitrate. All strains can produce acid when exposed to sugar, except a couple of sugars like mannitol, when oxygen is present.(25) The minimum water activity is .85 for growth. (19)

Corynebacterium is a Gram-positive normal flora in the nose. The Corynebacterial envelop is made up of peptidoglycan, arabinogalactan, corynemycloic and corynemycolenic acids, trehalose dimycolates, and phosphatides of mannose and inositol. The lipoidal antigens on the cell surface makes it invasive to the host's immune system, but it doesn't allow the bacteria to attach firmly to the surface of the nares. The Corynebacterial are facultatively aerobic organisms. They ferment glucose for energy, but they are unable to use maltose or galactose. They have granules of long-chain polyphosphate that stores phosphate and will be used as energy in stressful times.(27) Most species of Corynebacterium will not cause diseases in humans; however, there is a specific species that is highly infectious. The Corynebacterium diphtheriae causes infection in the upper respiratory tract, and can be deadly if untreated. (2)
Another Gram-positive bacterium that lives in the human nose is the Staphylococcus aureus, often referred to as staph. It is carried either on the skin or in the nose of healthy people, but 25% - 30% of the population is populated in the nose. The optimum pH for the Staphylococcus to live in is 7.0-7.5, and the optimum temperature is 30-37 degree Celsius. (19) The minimum water activity Staph needs to survive is .85. While Staph is growing, it will not cause any infection, until the bacteria can enter a wound. It cause an infection once it enters a wound because it has the ability to bind to fibrinogen, which is needed to form blood clots, just like Staphylococcus epidermidis.(28) Stap contains a high concentration of salt that inhibits other bacteria and it has the ability to ferment mannitol, a sugar, as a source of energy. (19)S. aureus did not attach to mucus-producing airway epithelium but to basolateral plasma membrane of columnar cells, to basal cells, and to the basement membrane. (1)
Micrococcus luteus is another Gram positive, spherical, bacterium that also resides in the nose as well as the mouth, skin and upper resipratory tract as an obligate aerobe. M. luteus is normally harmless except for those that have compromised immunities. M. luteus is resistant to reduced water potential that is found in mucus and can tolerate drying and high salt concentrations were the nasal cavity to dry up.
Diseased:
The nasal passages, being as large as it is (from a microbe's standpoint), can harbor many types of bacteria, viruses, and fungi which can often lead to infection. It is in fact the main site for different organisms to lodge and multiply. One very commonly found gram-positive bacteria is the Staphylococcus epidermidis which colonizes in the anterior naris. (11)It lives naturally on the skin and mucous membranes. Their grape-like appearance when viewed under the microscope only measures approximately 1-micrometer in diameter. This bacteria, if environmental conditions are optimal, will form biofilms to aggregate more securely. A three stage process of the exopolysaccharide casing of the biofilm provides excellent protection against the environment and phagocytosis by their host's immune system as they seek to mature and eventually dissolute from the colony. The slime (biofilm), mainly composed of teichoic acid and typically found on the cell wall of these microbes can also protect them against antibiotics making them very difficult to treat. This unique ability of the Staphylococcus epidermidis to form a biofilm in the nasal passages may be the reason for their strong virulence. A patient's inability to rid of S. epidermis due to its protective biofilm usually leads to infection.(13)
The Streptococcus pneumoniae bacteria is another Gram-positive bacteria that is commonly found in the nasal passages, primarily in a patient with acute sinusitis. This lancet-shaped bacteria, approximately 0.5 - 1.25 micrometers in diameter, is one of the primary causes of pneumonia. Although they are also found in the upper respiratory tract of healthy individuals, they are usually the cause of sinus infection when a small amount of this bacteria is lodged in the sinus cavities such as the ethmoid or maxillary sinuses, typically by the force of a sneeze or the blowing of the nose. They are mostly found in pairs (diplococci), but can sometimes be seen alone or in short chains. (12) The S. pneumoniae has an extremely thick cell wall, approximately six layers compose of peptidoglycan with teichoic acid. This teichoic acid has two choline residues that bind specifically to choline-binding receptors on human cells. Its capsule, composed of polysaccharides prevents phagocytosis of the bacteria. The pili structures on some strains of S. pneumoniae have been identified in the involvement of colonization in the nasal passages. (12) This allows them to gain a strong attachment to epithelial cells and sometimes leads to a challenging problem if left untreated.
Haemophilus_influenzae is a Gram-negative, rod-shaped bacterium that resides in the nasopharnyx region of the human nasal passage. They lack motility due to the absence of a flagella or pili. Its length is about 1.0 x 0.3 um. There are 6 strains of encapsulated H. influenzae, which are categorized based on the type of polysaccharide capsule. The differences are denoted a through f, with H. influenzae serotype b (Hib), as the most commonly vaccinated strain. This vaccination helps in the prevention of invasive H. influenzae disease in young children. However, there also exists a non-encapsulated strain referred to as non-typeable H. influenzae (NTHi) which is unaffected by the vaccine due to lacking an antigenic capsule. (14) Virulance of this bacterial strain is based in large part to the lipopolysaccharide (LPS) component of its outer membrane. (29) The LPS is an endotoxin and is composed of varying elements of monosaccharides, such as L-glycero-D-manno heptose, D-Glc, D-Gal, and sialic acid (Neu5Ac), which provide added protection against chemical attack and an increase the ability to cause disease. NThi usually infects the upper and lower respiratory tracts leading to pneumonia, sinusitis, and otitis media, which is an infection of the middle ear. Its encapsulated counterpart, specifically Hib and Hif, can cause meningitis and bacteremia, usually occurring in 3rd world countries where children are unvaccinated. (14)
There are many different microbes that either reside or just pass through the nasal passages, most of which impact the health of their host. Those microbes that have such an impact are listed and briefly described below.
| Microbial Species | Description of Microbe |
| Moraxella catarrhalis | (formerly Branhammella catarrhalis) Gram-negative bacteria which are found in mucous membranes, can be opportunistic. Cells are non-motile, short rods/cocci found individually or in pairs. Optimum at 33-36 degrees celsius |
| Eikenella corrodens | Gram-negative bacteria, anaerobic, faculatively aerobic, can be an opportunistic pathogen. Cells are non-motile, round-ended rods which may exhibit twitching motility. Reduces nitrate to nitrite. |
| Streptococcus pyogenes | Gram-positive bacteria, asporogenous, facultatively anaerobic. Cells are non-motile, typically 1-micrometer, generally found in pairs or chain. Fermentative with carbohydrates metabolized anaerogenically and homofermentatively. Optimum at 30-37 degrees Celsius. |
| Arcanobacterium | Genus of asporogenous bacteria, with wall type VI. They initially grow as irregular rod shapes and may eventually become granular and segmented. Growth primarily occurs through anaerobic or aerobic processes which can be enhanced by serum or blood and even increased pressures in CO2 |
| Chlamydia pneumoniae | Cause of acute respiratory infection, associated with subacute respiratory disease. Chronic infection and re-infection can lead to severe disease involving immunologically-based pathogenesis. |
| Rhinovirus | Genus of viruses from the family Picornaviridae, which infect the upper respiratory tract. They are the primary cause of the common cold as they can propagate in many types of human cells. Has the ability to withstand freezing temperatures, but is optimal at 33 degrees Celsius. |
(28)
Are there any other non-microbes present?
Normal: No plants, animals, or fungi live in the normal nasal passageway, although there is the presence of dust and other small particles which are inhaled from the outside environment.
Diseased: Fungal infection are not very common in the nasal passages, however, there have been cases in which patients that are immune-suppressed have experienced mycosis. Patients with uncontrolled diabetes or those with acquired immunodeficiency syndrome (AIDS) are typically a target for either Phycomycetes or Aspergillus. Other types of mycotic pathogens also infect humans, but are more uncommon. The fungal pathogens that usually invade the nasal passages are saprophytes which are found in soils and on plants, thriving in high glucose and acidic environments. As aspergillosis originates in the nose and paranasal sinuses it can invade the brain and vascular structures via arterial wall invasion causing tissue necrosis and arterial thrombosis. The aspergillus and bipolaris species can illicit an allergic response in the sinuses leading to chronic progressive inflammatory response which causes bone expansion and even bone destruction. Aeration and irrigation of the sinuses with a topical antifungal agent are treatments that may speed up the recovery process. (11)
Do the microbes that are present interact with each other?
The reason only 25% - 30% of the nasal passageway is populated by the S. aureus is beacuse S. epidermidis and Corynebacterium have a negative symbiosis behavior with the S. aureus. Some possible ways that the bacteria compete with one another is through the synthesis of bacteriocins, bacteriolytic enzymes, etc. or the competition of specific attachment to epithelial cells. There are S. aureus that produces some bactericiocin agains some Corynebacterium speices and S. epidermidis bacteriocin against S. aureus, but there is no bactericiocin produced by corynebacteria against the other two bacteria. Binding to the epithelial cells involves the carbohydrate portion of the human nasal mucin support. The Corynebacterium has a higher affinity for mucus than S. aureus and S. aureus has a higher affinity for than S. epidermidis. Corynebacterium specifically inhibts the colonization of S. aureus but not S. epidermidis. (1)
Competition for mucosal surface in the nasopharyngeal region exists between Streptococcus pneumoniae and Haemophilus influenza. These bacterial species compete for limited space in order to form stable colonies and propagate. Both will employ forms of microbial interference to exert their dominance over the opposition. S. pneumoniae, through neuramindase, has the ability to cleave terminal sialic acid residues. It will utilize this strategy to strip off sialic acid from the lipopolysaccharide component of H. infuenzae’s outer membrane thereby compromising its ability to withstand chemical attack. During the weakened state of its rival, S. pneumoniae will deliver the final blow by generating high levels of hydrogen peroxide via aerobic metabolism, which on contact, is lethal to H. influenza. However, even in the face of such awesome firepower, it is H. influenzae that wins out. H. influenza relies on the inflammatory response of the local host to get rid the competition. Although exact details are still being researched, H. influenzae has the ability to recruit the host responder, neutrophils. Neutrophils are a type of white blood cell that is capable of getting rid of S. pneumoniae and other microorganisms via phagocytosis. Due to its capsule, H. influenzae is able to avoid suffering the same fate as its rival. Once the competition is eliminated, H. influenzae is free to proliferate and infect the upper respiratory tract of its host. Conversely, when taking into consideration the application of vaccines and antimicrobials, these factors can also influence bacterial interspecies behavior and the outcome of the competition between them. (26)
Do the microbes change their environment?
The simple presence of a bacteria can change the environment in the nasal passages if it is identified by the host's immune system. The peptidoglycan of the bacterial cell wall in a penicillin resistant pneumococci is an essential and immunologically important aspect of the bacterial structure, consisting of repeating N-acetylgucosamine and N-acetyl muramic acid. The insoluble network of peptidoglycan induces the production of cytokines, accumulation of edema fluid and recruitment of leukocytes. The breakdown of the cell wall, however, causes this bioactivity to decrease. It is suggested that a receptor (TLR-2 receptor) recognizes the cell wall (peptidoglycan) of the bacteria and initiates an inflammatory response. An enormous response by various cells including macrophages, astrocytes, microglia, epithelial cell and endothelial cells have been noted by the presence alone of a bacterial cell wall. (18)
Staphylococcus aureus produces an enzyme called coagulase that changes fibrinogen to fibrin, thus clotting blood. Coagulase is bound tightly to the microbe's surface and reacts upon encountering blood. The fibrin is then coated around S. aureaus. It is believed that it helps the microbe resist phagocytosis, allowing it to become more virulent.
Streptococcus pneumoniae also has the ability of binding to epithelial cells by use of enzymes. They secrete an enzyme called pneumolysin which is thiol activated. Evidence suggests that in large quantity, this enzyme is toxic for epithelial ciliated epithelium and results in ciliostaticity in lower doses. This enzyme can also render bacteriocidal activity of phagocytes creating an extension of stay in the host for the bacteria. (21)
Do the microbes carry out any metabolism that affects their environment?
All bacteria listed in the table above that reside in the nasal passages conduct some degree of metabolism in order to obtain nutrients, intermediates for biosynthesis, and energy, all of which is necessary to sustain itself. For example, S. pneumoniae obtains energy through fermentation of sugars producing lactic acid as a side product. It breaks down large carbohydrate molecules in order to obtain the energy required for growth. Moreover, S. pneumonia produces hydrogen peroxide during pyruvate metabolism in aerobic growth. Hydrogen peroxide in high concentration is lethal towards competing bacteria in the surrounding area. For instance, hydrogen peroxide can hinder the growth of M. catarrhalis as well as H. influenzae. It is believed that S. pneumonia employs this type of microbial interference in order to out-compete other microbes for the limited mucousal surface necessary to form stable colonies. (26)
Current Research
A Nitric Oxide–Inducible Lactate Dehydrogenase Enables Staphylococcus aureus to Resist Innate Immunity
As previously mentioned, Staphylococcus aureus is found in the nose of about 25% - 30% of the human population. Researchers from the University of Washington were interested in finding out why this bacterium is able to survive the human's natural production of nitric oxide in the nasal passages. This production of nitric oxide in the nose and nasal passages usually protects against disease causing bacteria by preventing their respiration process. These researchers found out that S. aureus produces lactic acid in the presence of nitric oxide,making a chemical balance, allowing it to continue to grow in this type of environment. The researchers then found a way to remove the lactic acid production by Staphylococcus aureus and found that it was then not able to survive in the presence of nitric oxide. This was tested in mice and the researchers also found that there were no diseases caused by the modified bacterium. The researchers hope to use this type of modification to find new ways to prevent the survival of such bacteria without the use of antibiotics.(3)
Differential Roles of Surface Polysaccharide and Extracellular DNA in Staphylococcus aureus and Staphylococcus epidermidis Biofilms
Scientists researched the "functions of two staphylo9coccal biofilm matrix polymers: poly-N-acetylglucosamine surface polysaccharide (PNAG) and extracellular DNA (ecDNA)" and how the "PNAG-degrading enzyme, dispersin B, and DNase I inhibit biofilm formation, detach preformed biofilms, and sensitize biofilms to killing by the cationic detergent cetylpyridinium chloride (CPC)." The biofilms will help protect the bacteria from being nullified by antibiotics and host defenses. The scientists found that both dispersin B and DNase I will inhibit biofilm formation in S. aureus and PNAG-positive S. epidermidis strains. Dispersin B will efficiently and rapidly detach S. epidermidis biofilms, but not S. aureus. On the other hand, DNase I will cause separation of the biofilm and the surface in S. aureus, but not S. epidermidis. PNAG is a major matrix component of only S. epidermidis biofilm cells, but it is produced by both bacteria. The PNAG performs different functions in the biofilms of the two bacteria. The PNAG protects the S. epidermidis cells from CPC killing, while the PNAG works in early stages of S. aureus biofilms, which makes it resistant to the detachment of dispersin B. Overall, ecDNA and PNAG can be "general diffusion barriers" that stop detergents from killing the bacteria.(7)
Isolation and Molecular Characterization of Methicillin-Resistant Coagulase-Negative Staphylococci from Nasal Flora of Healthy Humans
Researchers form Cambridge University have isolated "methicillin-resistant coagulase negative staphylcocci (MRCNS) from the nasal flora of healthy humans" from three places in Rio de Janeiro City. They obtained swaps from the nares of the adults at two military quarters and students from a public school. Staphylcocci were isolated and "tested for the presence of the mecA gene" by hybridizing the gene with a specific probe. S. epidermidis was the most common MRCNS; it accounted for 38 out of the 45 total. The SmaI-digested DNA was also put through pulsed-field gel electrophoresis in order to study the clonality of the MRSE S. epidermidis. It appears that the cross-colonization contributed to the spread of the methicillin-resistance. The wide and diverse genome suggests that the spread of the mecA gene among the isolates were probably through horizontal transmission. It was concluded that though it was researched with only three institutions, it reflects how other communities in Rio may have gained methicillin resistance. (17)
Evaluation of Alternaria alternata for Biological Control of Amaranthus retroflexus
Researchers from Aberdeen University in Scotland found promising evidence that Alternaria alternata, a fungal allergen that can be found in the nasal passages, can hinder the growth of herbicide-resistant Amaranthus retroflexus, a weed known to hinder the yield of various crops in agriculture. Working in a controlled setting, these scientists were able to garner 100% mortality rate in A. retroflexus upon exposure to an A. alternata spore concentration of 10^7 spores ml^-1. The scientist prepared the spores by culturing A. alternata in a V-8 agar media that was allowed to incubate for 2-3 weeks. The harvested spores that were formulated in an oil emulsion produced the highest A. retroflexus mortality rate when inoculated at the four-leaf stage under the optimum post-dew temperature of 20-30 degrees for a 24 hour dew period. Furthermore, linear regression analysis showed rapid disease development and necrosis of the leaf area in A. retroflexus within 12 hours of exposure to the A. alternata spores. However, using A. alternata as a mycoherbicide requires further study due to the variability in actual field conditions. Regardless, the result of this study opens the door for safer and more effective alternatives for weed control, especially with the growing concerns over the environment and the health effects of consuming foods with herbicide residue. (16)
Local Pathogenic Bacteria in Allergic Rhinitis
Swiss scientists examined whether subjects’ allergic reactions affected the presence of potential pathogenic bacteria (PPB) that could be found in the nasal cavity. There is a variety of PPB which may include Staphylococcus aureus and Haemophilus influenzae among many. The researchers took a group of random men and women and took swabs from their nasal passageways. Skin tests for numerous allergens along with control tests were run for these subjects. They found that 15% of the subjects tested positive for skin tests for being allergic, ranging from high sensitivity to moderate sensitivity including sneezing, nasal itching, running nose, and increased nasal airflow resistance. Furthermore, the scientists found that about 90% of the positive subjects had PPB in their nasal passageways! On the other hand, only 36% of the negative subjects (who were not allergic) had PPB in their nasal cavities. In addition, it was found that the sensitized patients had more chance of having more than one PPB species in their nasal cavity. Although there is still much to be examined, the conclusion of this study is that subjects who test positive to aeroallergen skin tests have a higher chance of having nasal PPB, which indicates that PPB may be involved in allergic rhinitis. (19)
Staph Bacteria are Prolific Gene Swappers
According to scientists from the National Institute of Allergy and Infectious Diseases (NIAID), “when some disease-causing bacteria encounter a new obstacle, they simply readily swap DNA with their relatives to acquire the genes needed to overcome it. Staphylococcus aureus is the common “staph” bacterium responsible for several human diseases and had adapted itself to many different environments.” This research gives a new approach to antibiotics and vaccine design as it gives the solution to the problem of toxic shock syndrome and antibiotic- resistance infections. “Bacteria can easily become dangerous. S. aureus is a common microbe that often causes no illness. Some strains can cause diseases, however, including TSS, food poisoning and impetigo. The bacteria can infect the skin, blood, urinary tract and wounds, and are a common source of infections acquired in hospitals. Most people are unknowing S. aureus carriers, intermittently harboring the bacteria on their skin or in their nose and throat, even in the absence of illness. A technique called DNA microarray analysis was used to rapidly screen their samples. Upon analyzing the results, the researchers discovered nearly a fourth of the genome was dispensable, consisting of genes that were not required for the bacteria's basic life processes. These so-called contingency genes provide flexibility in the bacterium's ability to cause disease in humans, cows and other organisms.” These bacteria are very rapid in adapting to the changes by picking up other genes which helps them spread through a large population.(22)
Conclusion
Although the nose is a very small part of our body, it is still very important for us to function and stay healthy. It plays some major roles in protecting our body from microbes that might be infectious to us. On the other hand, it can also be the starting point of some allergies or major diseases like asthama which are very difficult to treat especially if it reaches its chronic state. We don't always remember to protect our airways when we work in the garden, use aerosols in the kitchen or even when pollen levels are high, but we must understand that a little effort to protect our nasal passages can go a long way. We must remember to take care of our nasal passageways in order to live a long healthy life, full of love and happiness.
References
4. Hall, Colman’s. Diseases of the Ear, .Nose and Throat. Harcourt Brace and Company, 2000.
5. Gest, Howard. Microbes an invisible Universe. Washington, D.C, 2003.
6. Washington N, Steeler, Jackson. “Determination of baseline human nasal PH and effect of intranasal administrative buffer.” Journal of Pharmaceutical 198 (2000): 139-146.
8. Rosin, Deborah. "Nasal Obstruction." "WebMD:'The Sinus Sourcebook.'" 1998.
9. Wilson, Michael. Microbial Inhabitants of Humans. Cambridge University Press. 2005. p. 140
10. Proctor, Donald F. The Nose: Upper Airway Physiology and the Atmospheric Environment. Elsevier Biomedical Press. 1982.
11. Donald, Paul J., Jack L. Gluckman, Dale H. Rice. The Sinuses. New York. 1995. pgs 57-60.
12. Todar's Online Textbook of Microbiology. Kenneth Todar. 2008. University of Wisconsin-Madison Department of Bacteriology. 24 August 2008. <http://www.textbookofbacteriology.net/S.pneumoniae.html>
13. M.U. Rasheed, Mohammed Awole: Staphylococcus epidermidis : A Commensal Emerging As A Pathogen With Increasing Clinical Significance Especially In Nosocomial Infections. The Internet Journal of Microbiology. 2007. Volume 3 Number 2.
18. Kimpen, Jan L.L. and Ramilo Octavio, eds. The Microbe-Host Interface in Respiratory Tract Infections. Norfolk United Kingdom. 2005.
19. Gluck, Ulrich and Gebbers, Jan-Olaf. "Local Pathogenic Bacteria in Allergic Rhinitis: A Novel Concept of Its Pathogenesis". Institute of Pathology and Environmental Medicine. 2003.
21. Niederman, Michael S., George A. Sarosi, Jeffrey Glassroth. Respiratory Infections. 1994. pg 50.
22. "Staph Bacteria are Prolific Gene Swappers, Researchers Show." National Institutes of Health 10 July,2001. 28 Aug 2008 <http://www3.niaid.nih.gov/news/newsreleases/2001/staphdna.htm>.
23. Buzina, Walter, Hannes Braun, Kerstin Schimpl and Heinz Stammberger. "Bipolaris spicifera Causes Fungus Balls of the Sinuses and Triggers Polypoid Chronic Rhinosinusitis in an Immunocompetent Patient ." Journal of clinical Microbiology 26 June 2003. 28 Aug 2008 <http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=254347>.
28. Singleton, Paul. Diana Sainsbury. Dictionary of Microbiology and Molecular Biology. 3rd Edition Revised. West Sussex, England. John Wiley & Sons, Ltd. 2006.
Edited by Jacinda Chen , Wayne Chen , Josephe Dalidi , Jennifer Hao , Rutu Kothari , Nidhi Patel , Natividad Rodriguez , Prudencio Sy, students of Rachel Larsen
