Candida Krusei: Difference between revisions
| Line 34: | Line 34: | ||
=6. Ecology= | =6. Ecology= | ||
<i>C. krusei </i> is found in many places around the world [[#References |[14]]]. Strains of <i>C. krusei </i> have been isolated in North America, Europe, Latin America, and the Asia-Pacific region from patient samples from over 142 hospitals [[#References |[14]]]. In Europe, the prevalence of <i>C. krusei </i> is the highest among geographic regions around the world with isolates of <i>C. krusei </i> most common in the Czech Republic, Poland and Slovakia. In contrast, <i>C. krusei </i> is more uncommon in the Asia-Pacific and Latin America regions of the world [[#References |[14]]]. | |||
Additionally, <i>C. krusei </i> can be isolated from a variety of food sources such as Japanese sake, Ginger Beer, and Baker’s Yeast [[#References |[9]]]. However, <i>C. krusei </i> is most commonly found in patients with hematologic malignancies and recipients of blood and bone marrow transplants [[#References |[14]]]. | |||
<i>C. krusei </i> susceptibility to voriconazole, a strong anti-fungal used to treat <i>C. krusei </i> infections, varies based on the region the <i>C. krusei </i> strain is localized [[#References |[14]]]. Overall, North American strains of <i>C. krusei </i> had the highest rates of susceptibility to voriconazole, over 90% susceptibility. In contrast, Latin American countries had the lowest rates of susceptibility to voriconazole, with under 70% susceptibility in some countries [[#References |[14]]].There are no clear mechanism behind these differences known but there is speculation that it could be the geographic differences in the ecology of <i>C. krusei </i> or the in the use of cytotoxic drugs and antimicrobial agents. [[#References |[14]]] | |||
=7. Pathology= | =7. Pathology= | ||
How does this organism cause disease? Human, animal, plant hosts? Virulence factors, as well as patient symptoms. | How does this organism cause disease? Human, animal, plant hosts? Virulence factors, as well as patient symptoms. | ||
Revision as of 15:19, 12 December 2016
1. Classification
a. Higher order taxa
Domain: Eukarya
Kingdom: Fungi
Phylum: Ascomycota
Class: Saccharomycetes
Order: Saccharomycetales
Family: Saccharomycetaceae
Genus: Candida
Species: Krusei
[1]
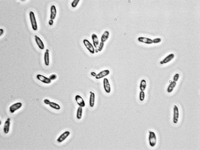
2. Description and significance
Candida krusei is a yeast species that does not produce spores that is usually found growing as a single cell or as pseudohyphae [1]. In the single cell form, the cells of C. krusei are round or ovoid and can be easily separated while in the pseudohyphae form the cells are more elongated and attached to neighboring cells [2]. C. krusei is considered a relatively uncommon, emerging opportunistic human pathogen [3] that infects mainly immunocompromised patients, especially those that have some form of leukemia or other deficiencies in white blood cells [4]. C. krusei is gaining recognition in the world today since it is a multidrug resistant pathogen due to its ability to rapidly adapt to antifungal treatments and its complex susceptibility profile [5]. C. krusei is most often found in the human microbiome in immunocompromised patients [4], in some foods, and it is used extensively in chocolate production from West African cocoa beans.
Before the 1960s, C. krusei was regarded as a species with low pathogenicity and virulence in humans compared to other species in the genus Candida [4]; however, since 1960, C. krusei infections have increased alarmingly. C. krusei is inherently resistant to the triazole antifungal, fluconazole which allows it to persist and cause infection in humans being treated with antifungals where other fungi cannot survive [6]. Of particular note is the high presence of C. krusei in the human microbiome in immunocompromised patients due to selection by prophylactic oral rinse therapy [2]. The increased use of fluconazole and other traizole antifungals to treat and quell fungal infections has thus led to a marked increase in infections by C. krusei , making it increasingly relevant in the world today [1]. However, although much is now known about C. krusei because of its status as an emerging pathogen, its genome has yet to be characterized and sequenced [7]. Additionally, a point of contention in the scientific community is whether or not C. krusei should be re-classified into a genus of its own since srRNA analysis and analysis of various ubiquinone systems in related species reveals C. krusei diverged much earlier than other Candida species [3].
3. Genome structure
C. krusei has eight chromosomes, in contrast to most members of the genus Candida, such as C. albicans, which has sixteen [1]. This difference, in addition to differences in cell structure and cell wall structure as compared to other Candida species, form the basis of the argument that C. krusei should be re-classified into a different genus [3]. While it is known how many chromosomes C. krusei has, the genome of C. krusei has yet to be sequenced [8], so the genome has not been fully characterized. However, increased infection rates of Candida species other than C. albicans [7] have generated more interest in the species and work is being done to sequence and characterize the genome of C. krusei [8].
4. Cell structure
C. krusei is usually found in one of two basic morphologies, single cell yeast or pseudohyphae; however, both forms are usually present at the same time in any growing culture [1]. In contrast to most members of the genus Candida, the cells of C. krusei are not shaped like ovals, but rather are elongated and closely resemble long grain rice when in the single-cell morphology [1]. This cell morphology is shared only with C. kejyr in the Candida genus [1]. On the other hand, when in the pseudohyphal morphology, the cells of C. krusei are elongated and attached to neighboring cells [1]. Both cell morphologies are pictured in Figure 1. The cells of C. krusei contain a cell wall that is made up of six layers that contain high concentrations of the polysaccharide alpha-D-mannan with a backbone made up of (1-6) linkages and side chains consisting of (1-2) or (1-3) linkages. These polysaccharides act as antigens on the cell surface that differentiate it from other Candida species that have different types of mannan in their cell walls [1]. Also, the C. krusei cell membrane is strongly hydrophobic which allows stronger attachment to non-polar surfaces compared to other members in the Candida genus [5]. Finally, as with most other eukaryotic cells, C. krusei cells contain organelles including ribosomes and small vesicles [1].
5. Metabolic processes
Describe important sources of energy, electrons, and carbon (i.e. trophy) for the organism/organisms you are focusing on, as well as important molecules it/they synthesize(s).

6. Ecology
C. krusei is found in many places around the world [14]. Strains of C. krusei have been isolated in North America, Europe, Latin America, and the Asia-Pacific region from patient samples from over 142 hospitals [14]. In Europe, the prevalence of C. krusei is the highest among geographic regions around the world with isolates of C. krusei most common in the Czech Republic, Poland and Slovakia. In contrast, C. krusei is more uncommon in the Asia-Pacific and Latin America regions of the world [14]. Additionally, C. krusei can be isolated from a variety of food sources such as Japanese sake, Ginger Beer, and Baker’s Yeast [9]. However, C. krusei is most commonly found in patients with hematologic malignancies and recipients of blood and bone marrow transplants [14]. C. krusei susceptibility to voriconazole, a strong anti-fungal used to treat C. krusei infections, varies based on the region the C. krusei strain is localized [14]. Overall, North American strains of C. krusei had the highest rates of susceptibility to voriconazole, over 90% susceptibility. In contrast, Latin American countries had the lowest rates of susceptibility to voriconazole, with under 70% susceptibility in some countries [14].There are no clear mechanism behind these differences known but there is speculation that it could be the geographic differences in the ecology of C. krusei or the in the use of cytotoxic drugs and antimicrobial agents. [14]
7. Pathology
How does this organism cause disease? Human, animal, plant hosts? Virulence factors, as well as patient symptoms.
7. Key microorganisms
Include this section if your Wiki page focuses on a microbial process, rather than a specific taxon/group of organisms
8. Current Research
Include information about how this microbe (or related microbes) are currently being studied and for what purpose
9. References
It is required that you add at least five primary research articles (in same format as the sample reference below) that corresponds to the info that you added to this page. [Sample reference] Faller, A., and Schleifer, K. "Modified Oxidase and Benzidine Tests for Separation of Staphylococci from Micrococci". Journal of Clinical Microbiology. 1981. Volume 13. p. 1031-1035.
Edited by Kailyn Doiron, Beth Grinkevich, Alvaro Dafonte Imedio, and Puja Patel students of Jennifer Talbot for BI 311 General Microbiology, 2016, Boston University.
