THE DIAGNOSIS OF SYPHILIS
Introduction
By [Heather Fantry]
Syphilis is a sexually transmitted infection that has been rising in prevalence since 2000 (CDC, 2013). It is caused by the spirochete
Treponema pallidum.
T. pallidum is a thin, tightly coiled spirochete that is microaerophilic (Tramont, 2005). Unlike most bacteria that infect humans, it cannot be cultured in the laboratory. It can only be cultured in laboratory animals, usually rabbits, which are not readily available in hospitals or medical clinics. Hence the diagnosis of syphilis is extremely difficult.
Bold
Italic
Clincial Signs and Symptons

Before understand how to diagnose syphilis, it is important to know about the stages of disease since different methods may be used for different stages. Primary syphilis h occurs 9-90 days after contact with T. pallidum (Tramont, 2005). It is manifested by a skin lesion called a chancre Figure 1) (CDC, 2013). It starts out as flat area of redness that develops into a bump and then into a swallowing opening in the skin. The chancre occurs at any place on the body in which an individual has had contact with T. pallidum. This is usually on the penis in a man or external genitalia in a woman but can be in the mouth or even on a finger.
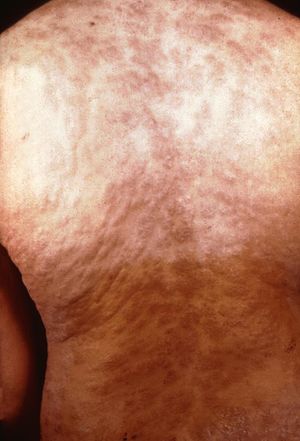
The next stage is secondary syphilis. This occurs 3-10 weeks after the initial lesion if a person is not treated with antibiotics (Tramont, 2005). This means that T. pallidum has spread throughout the body. The most common symptom is a non-itchy rash that is not raised and often is on all parts of the body (Figure 2). Other manifestations can include fever, headache, weight loss, lymph node swelling, loss of hair, and eye disease. Individuals also may develop condyloma latum which are flat bumps in the genital area which have lots of T. pallidum and are very infectious. In addition, individuals can get flat patches in their mouth called mucous patches.
The third stage is latent syphilis (CDC, 2013). It has no signs or symptoms and the only manifestation of the disease is a positive blood test.
The final stage is tertiary syphilis which only occurs in 35% of untreated patients (Tramont 2005). It occurs 10-25 years after primary syphilis. Most commonly it causes disease of the nervous system but it also can cause heart disease or deposits in the skin, soft tissue, or bones called gummas. The neurological manifestations are meningitis, strokes, dysfunction of cranial nerves, dementia, difficulty walking, visual or auditory problems, and loss of vibration sense.
T. pallidum can be transmitted from a mother to her unborn child which is called congenital syphilis (CDC, 2013). Although rare in the United States, it is of great concern because it can cause deafness, neurological problems, bone deformities, and even death (CDC, 2013).
Who Should be Tested for Syphilis?
Individuals with any of the signs and symptoms of syphilis should be tested for syphilis (CDC, 2014). In addition, persons with no symptoms but are at risk for syphilis should be tested. This includes persons whose have multiple sexual partners, use illegal drugs, use alcohol, have unprotected sex, and are prostitutes. It also includes men who have sex with men, prisoners, and HIV-infected patients. In addition, anyone who has a sexual partner that has syphilis should be tested. Finally, women who are pregnant should also be tested because of the risk of transmission to their infant.
Knowledge of the syphilis epidemic also is helpful (Figure 3). Syphilis is most common in urban areas and the south so any sexually active person should be tested in these areas. The state with the highest rate is Maryland.
Direct Diagonsis
Microscopy
The most sensitive and quickest method to diagnose primary syphilis is microscopy (Tramont 2005). A swab is place in the chancre and T. pallidum attaches to the swab and can be viewed under a microscope. However, T. pallidum is so thin (0.1 µm) that it cannot resolve light and can only be detected by light scattering which requires a special darkfield microscope. Under darkfield microscopy, T. pallidum will look like a corkscrew rapidly turning around its midpoint (Slonczewski and Foster, 2014 and Tramont, 1995) (Figure 4). However, a dark field microscope requires skilled technicians and is so expensive that it is not readily available at hospitals or other medical facilities (Tramont, 1995).

Polymerase Chain Reaction (PCR)
Another direct method that is available to diagnose syphilis is PCR. PCR is used to amplify sections of T. pallidum DNA which was fully sequenced in 1998 (Fraser et al, 1998). It can be used to diagnose primary syphilis by taking a swab from the chancre. This method has been showed to be 82% sensitive and 95% specific (Grange et al, 2012). It can also be used to diagnose secondary syphilis using a blood sample and to diagnose congenital syphilis using frozen or formalin fixed placental tissue (Genest et al, 1996 and Heymans et al, 2010). However, T. pallidum PCR is not readily available in the United States and specimens have to be shipped to the CDC (CDC, 2015) Submission requires special approval by the local health department and the turnaround time is two weeks.
References
[1] Hodgkin, J. and Partridge, F.A. "Caenorhabditis elegans meets microsporidia: the nematode killers from Paris." 2008. PLoS Biology 6:2634-2637.
Authored for BIOL 238 Microbiology, taught by Joan Slonczewski, 2015, Kenyon College.
