Adeno-Associated Viruses as Gene Therapy Vectors: Difference between revisions
No edit summary |
|||
| Line 21: | Line 21: | ||
==Gene Therapy of Cystic Fibrosis Using AAV== | ==Gene Therapy of Cystic Fibrosis Using AAV== | ||
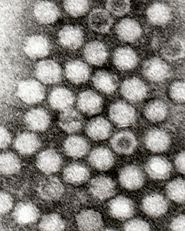
[[Image:CF Specificity.gif|thumb|325px|right|Genome of AAV.]] | |||
<br>Cystic fibrosis, a hereditary genetic disorder of the CFTR gene that produces chloride ion channels in the epithelium of airway tissue, which are important for the proper production of mucus, sweat, and digestive juices. In the lungs, defective CFTR genes often result in mucus that is too thick to be efficiently moved out of the system. This means that pathogens in the respiratory system aren’t removed from quickly enough and the person is more susceptible to infection. <br> | <br>Cystic fibrosis, a hereditary genetic disorder of the CFTR gene that produces chloride ion channels in the epithelium of airway tissue, which are important for the proper production of mucus, sweat, and digestive juices. In the lungs, defective CFTR genes often result in mucus that is too thick to be efficiently moved out of the system. This means that pathogens in the respiratory system aren’t removed from quickly enough and the person is more susceptible to infection. <br> | ||
<br>Previously, gene therapy using viruses in the respiratory tract has been difficult as respiratory viruses typically have low infection rates. Respiratory viruses have low rates of infection because there is a precarious evolutionary balance that viruses have to tiptoe between virulence and infectivity. If they are too virulent, they will kill all the host cells, if they are too infective and not virulent enough, they will exhaust the number of host cells. In either case, the virus particles will be eliminated from the system. For this reason, if scientists want to utilize respiratory viruses as gene transfer vectors, they must find a way to increases the infectivity. Scientists at the University of Iowa and University of California, Berkeley have done this using natural, evolutionary, techniques of introducing a variety of virus phenotypes into the system and selecting for the virus that is most infective. In the first stage of this search they shifted around the capsid genes from two different serotypes of the AAV, AAV2 and AAV5, to see whether they could increase the infectivity of the virus to the host cells. They optimized the viral capsid by subjecting the capisid coding genes to DNA shuffling and error-prone PCR so that extensive variation was observed. They then selected AAV mutants that were effective at gaining entry to the nucleus by having those particles amplified by helper adenoviruses in the cell. They did multiple rounds of this selection and encountered increasing amounts of new serotypes relative to AAV2. After five rounds of this selection, they found a variant that was a combination of AAV2 and AAV5, which they named AAV2.5T. When host cells were treated with this “chimera,” transduction and binding both increased when compared to the original AAVs, which indicated that this new variant would be able to efficiently transduce genes into the airway epithelial cells and act as an effective therapeutic agent.<br> | <br>Previously, gene therapy using viruses in the respiratory tract has been difficult as respiratory viruses typically have low infection rates. Respiratory viruses have low rates of infection because there is a precarious evolutionary balance that viruses have to tiptoe between virulence and infectivity. If they are too virulent, they will kill all the host cells, if they are too infective and not virulent enough, they will exhaust the number of host cells. In either case, the virus particles will be eliminated from the system. For this reason, if scientists want to utilize respiratory viruses as gene transfer vectors, they must find a way to increases the infectivity. Scientists at the University of Iowa and University of California, Berkeley have done this using natural, evolutionary, techniques of introducing a variety of virus phenotypes into the system and selecting for the virus that is most infective. In the first stage of this search they shifted around the capsid genes from two different serotypes of the AAV, AAV2 and AAV5, to see whether they could increase the infectivity of the virus to the host cells. They optimized the viral capsid by subjecting the capisid coding genes to DNA shuffling and error-prone PCR so that extensive variation was observed. They then selected AAV mutants that were effective at gaining entry to the nucleus by having those particles amplified by helper adenoviruses in the cell. They did multiple rounds of this selection and encountered increasing amounts of new serotypes relative to AAV2. After five rounds of this selection, they found a variant that was a combination of AAV2 and AAV5, which they named AAV2.5T. When host cells were treated with this “chimera,” transduction and binding both increased when compared to the original AAVs, which indicated that this new variant would be able to efficiently transduce genes into the airway epithelial cells and act as an effective therapeutic agent.<br> | ||
<br>The next stage of this experiment was to determine whether or not this new particle could effectively express the CFTR gene, the defective gene that causes cystic fibrosis, and fix the problematic chloride ion channel. They inserted an effective CFTR gene into the viral genome and saw that the vector was effectively able to bind the target host cells and restore appropriate levels of chloride ion flow in the previously defective cells. Before the introduction of this vector to the system, the CFTR protein product was not visible to the researchers using immunocytochemistry. After the treatment, however, CFTR protein is easily visible and is being produced in the correct location on the epithelial cells<br> | |||
==Conclusion== | ==Conclusion== | ||
Revision as of 01:40, 16 April 2009
Adeno-Associated Viruses
Adeno-associated viruses (AAV) small viruses that affect humans and other members of the primate species. They belong to the parovirus family and require a helper virus, such as adenovirus, herpes simplex virus, vaccina virus, or CMV, to replicate. For this particular reason they are also part of the dependovirus genus. If no helper virus is present, they are able to incorporate themselves into the host cell’s genome and latently replicate as the host cell replicates. When a helper virus infects the cells that the AAV has latently incorporated itself into, it is able to engage in lytic replication and release itself from the cell.
The AAV genome is made up of ssDNA, is very small (4.7kbp), and is flanked by two 145 nucleotide-long inverted terminal repeats. It codes for two different types of proteins, the first being Rep, which is responsible for replication and rescue of the virus. The second protein, Cap, is a structural protein that is the chief constituent of the icosahedral capsid that houses the viral genome. Furthermore, the AAV genome contains three promoters, p5, p19, and p40, and two open reading frames. The mRNA transcripts produced in conjunction with each of the promoters is able to code for seven different Rep and Cap proteins due to alternate splicing. AAV’s genome doesn’t code for a DNA polymerase and is consequently dependent on that provided by the host cell. AAV are very simple viruses, but as we will see, they have an extremely wide variety of medicinal applications.
AAV Vector Production (2 Transfection Method)
The first step in producing AAV vectors is finding helper viruses that will aid in replicating the AAV. Many times this helper virus is an adenovirus, which needs a minimum of its E2A, E4, and VA1/II gene regions in order to be effective at replicating the AAV. Then, two plasmids are created, one containing the AAV rep and cap genes plus the adenoviral helper genes prescribed above. The other plasmi containins an expression cassette composed of a CMV promoter, multiple cloning site, and SV40 polyA. This expression cassette on the second plasmid is also flanked by AAV inverted terminal repeats. This concoction is then transfected into a large quantity of 150mm dishes that contain the 293 line of human embryonic kidney cells, which encode the E1 region of the Ad5 genome. After the transfection, the cells are harvested and purified using ultracentrifugation. Another advantage of the AAV system is that large number of AAV can be harvested using these techniques (>10^8vp/ml).
The only portions of the AAV that are absolutely necessary in cis to the vector are the inverted terminal repeats and the therapeutic gene. The packaging and structural genes, rep and cap, are able to be provided in trans. This means that the genome of the AAV can essentially be wiped out to make room for recombinant genes.
Using AAV Vectors to Treat Diseases
AAV vectors have been shown to be capable or targeting a wide variety of diseases and malignancies. Common diseases targeted include various types of cancer, neurodegenerative diseases, arthritis, muscular dystrophy, cystic fibrosis, hemophilia B, and many more.
Functionally, AAV are well suited as gene vectors. One important aspect of their function is that they are able to transduce a wide variety of cells regardless of their stage in the cell cycle. This is extremely important because it allows them to target cells that are differentiated, and also cells that are rapidly dividing, such as cancer cells. Furthermore, AAV are desirable as gene vectors because when they infect host cells, they elicit little immune response. If any response is elicited, it is little more than the generation of neutralizing antibodies. No cytotoxic effect is caused, and the host system is relatively unaffected other than the intended, therapeutic, infection. All of these aspects of AAV are important, but probably the greatest advantage of the AAV vector system is that it allows for permanent genetic implantations to occur. Unlike the adenovirus, AAV is able to permanently implant its genes into the genome of the host, which creates a relatively-long term effect on the host as opposed to a powerful, transient, effect like that typically produced by adenoviral vectors. AAV are also extremely reliable and predictable when inserting their genes into the host cell’s genome. They always implant their genes into a particular spot on the 19th chromosome of humans, while retroviruses are extremely unpredictable and prone to mutating DNA during implantation. If mutations or misplaced insertions occur at this stage of the therapy, malignancies and adverse effects may be observed, compromising the efficacy of the treatment. There are also 11 different serotypes of AAV that are all different in their structure. Certain serotypes, such as AVV2, are specific to particular receptors in the host. This aids researchers to mix and match the genomes of these serotypes to find a vector that is specific to a particular receptor in the host. All of these are advantages make using AAV very desirable for a wide variety of gene therapy treatments.
While there are a great amount of advantages to using the AAV vector system, there are also a few drawbacks. The main drawback of using AAV as vectors is that the small size of their genome (4kbp) significantly limits the amount of genetic material that it can carry. Oftentimes, almost the entire genome must be replaced in order for the required genes to be placed onto the AAV. By comparing the size of the AAV genome to other types of vectors it becomes evident as to why it is so disadvantageous. Adenoviruses, for example, can carry roughly twice as much material and retroviruses usually hold between 8-10kbp. While the AAV is unable to carry large genes, steps are being taken to discover ways to expand the carrying capacity of AAV vectors by annealing the two inverted terminal repeats (ITR).
Gene Therapy of Cystic Fibrosis Using AAV
Cystic fibrosis, a hereditary genetic disorder of the CFTR gene that produces chloride ion channels in the epithelium of airway tissue, which are important for the proper production of mucus, sweat, and digestive juices. In the lungs, defective CFTR genes often result in mucus that is too thick to be efficiently moved out of the system. This means that pathogens in the respiratory system aren’t removed from quickly enough and the person is more susceptible to infection.
Previously, gene therapy using viruses in the respiratory tract has been difficult as respiratory viruses typically have low infection rates. Respiratory viruses have low rates of infection because there is a precarious evolutionary balance that viruses have to tiptoe between virulence and infectivity. If they are too virulent, they will kill all the host cells, if they are too infective and not virulent enough, they will exhaust the number of host cells. In either case, the virus particles will be eliminated from the system. For this reason, if scientists want to utilize respiratory viruses as gene transfer vectors, they must find a way to increases the infectivity. Scientists at the University of Iowa and University of California, Berkeley have done this using natural, evolutionary, techniques of introducing a variety of virus phenotypes into the system and selecting for the virus that is most infective. In the first stage of this search they shifted around the capsid genes from two different serotypes of the AAV, AAV2 and AAV5, to see whether they could increase the infectivity of the virus to the host cells. They optimized the viral capsid by subjecting the capisid coding genes to DNA shuffling and error-prone PCR so that extensive variation was observed. They then selected AAV mutants that were effective at gaining entry to the nucleus by having those particles amplified by helper adenoviruses in the cell. They did multiple rounds of this selection and encountered increasing amounts of new serotypes relative to AAV2. After five rounds of this selection, they found a variant that was a combination of AAV2 and AAV5, which they named AAV2.5T. When host cells were treated with this “chimera,” transduction and binding both increased when compared to the original AAVs, which indicated that this new variant would be able to efficiently transduce genes into the airway epithelial cells and act as an effective therapeutic agent.
The next stage of this experiment was to determine whether or not this new particle could effectively express the CFTR gene, the defective gene that causes cystic fibrosis, and fix the problematic chloride ion channel. They inserted an effective CFTR gene into the viral genome and saw that the vector was effectively able to bind the target host cells and restore appropriate levels of chloride ion flow in the previously defective cells. Before the introduction of this vector to the system, the CFTR protein product was not visible to the researchers using immunocytochemistry. After the treatment, however, CFTR protein is easily visible and is being produced in the correct location on the epithelial cells
Conclusion
Overall paper length should be 3,000 words, with at least 3 figures.
References
Edited by student of Chad Kurylo for BIOL 238 Microbiology, 2009, Kenyon College.