Borrelia burgdorferi Survival Mechanisms Against the Mammalian Immune System
Borrelia burgdorferi is a Gram-negative spirochete bacterium and is the most studied cause of Lyme disease, the most widespread vector-borne infection in the United States and Europe. It is spread by Ixodes tick bites. The disease causes a wide variety of symptoms and, if left unidentified and untreated, can lead to irreversible, chronic multisystem damage. For this reason, research into the transmission and behavior of B. burgdorferi has been crucial to improved diagnostic techniques and treatment of the disease.
One aspect that has been highly examined is the bacteria’s ability to evade the immune system and medical tests, which allows it to remain and spread within the host causing catastrophic long-term damage. It has been found that the bacteria can elude the immune system in multiple ways including by directly inhibiting the host’s immune system, changing their outer membrane antigens to avoid recognition and physically hiding within the host’s tissues.
Interaction with the Innate Immune System
The first defense against foreign bodies within mammals is the innate immune system. This system is comprised of a number of signal molecules, to activate an immune response, and phagocytes, to quickly engulf and decompose any thing that is not the individual’s own cells (self-cells). For this reason, Borrelia burgdorferi, and other pathogens, have had to develop ways to avoid these defensive mechanisms.
The Complement System
The complement system in mammals uses factor H and factor H-like protein 1(FHL-1), soluble glycoproteins residing in the circulatory system, to alert the immune system when there are cells that are not identified as self-cells. B. burgdorferi have found a way to minimize this activation of the immune response by binding to factor H and FHL-1 to prevent it from signaling. Complement regulator-acquiring surface protein A (CspA or CRASP1) binds to factor H and FHL-1 and can inactivate the formation of C3b, the start of the pathway for activation of the immune response, and the terminal complement complex, the signal for the immune system that a foreign cell is present. CspA is a protein that has two subunits. This structure is thought to give CspA increased access to the binding site of factor H and FHL-1, allowing it to firmly attach. Although, the binding region is located inside the unbound protein complexes of factor H and FHL-1, the region is exposed when the C-terminal region of the proteins are bound to another molecule. Erp, a family of B. burgdorferi surface proteins, will bind to this C-terminal region and may allow for the binding of CspA (Caesar et al. 2013).
Phagocytes
Phagocytes are a non-discriminatory method of immediately neutralizing any possible harmful non-self cells. There are a variety of these cells in the innate immune system, but most work by engulfing a foreign cell it into a vesicle, which then fuses to a lysosome containing enzymes and molecules to degrade the foreign cell by oxidation and lysis. To prevent this, B. burgdorferi use outer surface protein (Osp) B to attenuate oxidative bursts, making their digestion less likely (Hartiala et al. 2008).
The bacteria also contain similar proteins, OspA and OspC, which are thought to play a more important role in release from the tick. Although little is known about their direct affect on the host, the bacteria cannot survive the immune system without these proteins, thus it is thought that they may aide in immune evasion (Grimm et al 2004).
Interaction with the Adaptive Immune System

The adaptive immune system consists of cells that recognize specific foreign bodies as pathanogenic and thus target and destroy these elements. This system works by creating antibodies on memory cells that correspond to antigens on known pathogens. Antigens can consist of any outer membrane substances displayed by the pathogen. Borrelia burgdorferi has many outer membrane substances that could be recognized, so this is a potential problem for the bacteria if they want to stay alive.
B. burgdorferi uses variable lipoprotein surface-exposed (VlsE) to cause interactions with the immune system so that none of its other, more important proteins are identified and remembered as antigens. VlsE is B. burgdorferi’s only known adapting protein and consists of a crystal structure with six variable regions. These regions are localized at the surface of the molecule so they can interact with and trick the immune system (Eicken et al. 2002). The highly selective environment inside the mammalian host encourages the rapid changing of VlsE. To accomplish this, silent cassettes (mobile elements), and donor sequences are used to manipulate the genes in addition to single base pair changes (Coutte et al. 2009).
The rapid changes in VlsE have been identified as crucial to immune system evasion. This is because the host quickly develops immunity to one VlsE and would be able to identify and kill the bacteria if they continued to express it. Changing the VlsE continuously ensures that the bacteria is always one step ahead of the immune system and is able to live indefinitely within the host (Rogovskyy and Brankhead 2013).
Physical Evasion from the Immune System
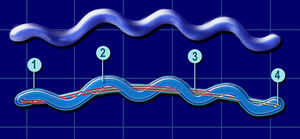
Borrelia burgdorferi is spread through tick bites, thus the first point of entry for the bacteria is the bloodstream. This is the primary place where the immune system response operates, thus leaving the vessels and residing inside the host tissue is a very effective way for bacteria to avoid the immune system entirely. The bacteria have an ideal structure for accomplishing this. B. burgdorferi is a spirochete bacterium with a flagella running through the middle of its body. This configuration allows the bacteria to move very quickly, penetrate cells like a corkscrew, and adhere to surfaces due its large surface area.
Types of interactions
B. burgdorferi can interact with the endothelial cells lining blood vessels in four ways: transiently, dragging, adhering, and burrowing (Norman et al 2008). Most of the interaction (89%) is transient, where the bacteria rapidly cycle through attachment and detachment as they are swept along with the bloodstream. They also spend time dragging (10%), where the bacteria adhere along their length to the endothelium and move more slowly. These two interactions happen mostly along the endothelial cell surfaces, whereas adhesion and burrowing are more common at cell junctions. In adhesion, bacterial cells attach to different aspects of the extracellular matrix. In extravasation, or burrowing, the bacteria corkscrew themselves end first into the endothelium and burst out of the vessels into the surrounding tissue. This is the least common interaction but not only allows the bacteria to evade the immune system, but also gives them access to all other organ systems, including the nervous system and brain.
Specifics Interaction Molecules
Because there are a large number of extracellular molecules to interact with, B. burgdorferi makes many receptors and interaction molecules. Most commonly, the bacteria bind to proteins in the extracellular matrix that allow the host cells to adhere, grow, migrate and differentiate. This is because they are essential for the host and are guaranteed to be present. These molecules include: Fibronectin (Fn), Decorin, glycosaminoglycans (GAGs), and laminin (Antonara et al 2011). The bacteria can also bind to integrins, cation-dependent surface receptors present on the surface of all mammalian cells. There are many proteins on the host cells, but the bacteria make many more receptors than are necessary, and they often end up having redundant functions. This overproduction may help the bacteria stay in the cell longer and adhere to a wider variety of cells and animals.
The bacteria can also reside within the host cells. In epithelial cells, the bacteria have been observed living in compartments where they can multiply or remain dormant for many years while avoiding the affects of the immune system and synthetic drugs and tests (Ma et al. 1991).
Further Reading
References
Takai, Hammerschmidt C, Koenigs A, Siegel C, Haillström T, Skerka C, Wallich R, Zipfel F, Kraiczy P. “Versatile Roles of CspA Orthologs in Complement Inactivation of Serum-Resistant Lyme Disease Spirochetes.” Infection and Immunology. 82(1): 380-392.
Caesar J, Wallich R, Kraiczy P, Zipfel P, Lea S. “Further Structural Insights into the Binding of Complement Factor H by Complement Regulator-Acquireing Surface Protien 1 (CspA) of “Borrelia burgdorferi”.” Structural Biology and Crystallization Communications. 69: 629-633.
Bhattacherjee A, Oeemig J, Kolodziejczyk R, Meri T, Kajander T, Lehtinen M, Iwai H, Jokiranta T, Goldman A. 2013. “Structural Basis for Complement Evasion by Lyme Disease Pathogen “Borrelia burgdorferi”.” The Journal of Biological Chemistry. 288(26): 18685-18695.
Hartiala P, Hytönen J, Suhonen J, Leppäranta O, Tuominen-Gustafsson H, Viljanen M. “”Borrelia burgdorferi” Inhibits Human Neurtophil Functions.” Microbes and Infection. 10(1):60-68.
Grimm D, Tilly K, Byram R, Stewart P, Krum J, Bueschel D, Schwan T, Policastro P, Elias A, Rosa P. “Outer-Surface Protein C of the Lyme Disease Spirochete: A Protein Induced in Ticks for Infection of Mammals.” Proceedings of the National Academy of Sciences of the USA. 101(9): 3142-3147.
Eicken C, Sharma V, Klabunde T, Lawrenz M, Hardham J, Norris S, Sacchettini J. “Crystal Structure of Lyme Disease Variable Surface Antigen VlsE of “Borrelia burgdorferi”.” The Journal of Biological Chemistry. 277: 21691-21696
Rogovskyy A, Bankhead T. “Variable VlsE Is Critical for Host Reinfection by the Lyme Disease Spirochete.” PLOS ONE. 8(4).
Couttle L, Botkin D, Gao L, Norris S. “Detailed Analysis of Sequence Changes Occurring during vlsE Antigenic Variation in the Mouse Model of “Borrelia burgdorferi” Infection.” PLOS Pathogens. 5(2).
Antonara S, Ristow L, Coburn J. 2011. “Adhesion Mechanisms of “Borrelia burgdorferi”.” In: Linke D, Goldman A, editors. Bacterial Adhesion: Chemistry, Biology, and Physics. Springer Netherlands. p. 35-49.
Ma Y, Sturrock A, Weis J. 1991. “Intracellular-Localization of “Borrelia burgdorferi” within Human Endothelial Cells.” Infection and Immunology. 59(2): 671-678.
Norman MU, Moriarty T, Dresser A, Millen B, Kubes P, Chaconas G. 2008. “Molecular Mechanisms Involved in Vascular Interactions of Lyme Disease Pathogen in a Living Host.” PLOS Pathogens. 4(10): 1-10.
Edited by (Mia Farago-Iwamasa), a student of Nora Sullivan in BIOL168L (Microbiology) in The Keck Science Department of the Claremont Colleges Spring 2014.


