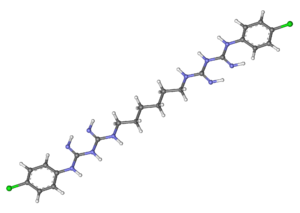
Chlorhexidine
Chlorhexidine is used as a prescription mouthwash to fight gingivitis and periodontists. Chlorhexidine is the most thoroughly researched antimicrobial agent used in dentistry in terms of ability to control cariogenic activity. It is effective in reducing plaque and gingivitis in teeth and gums but can causes an alteration in taste and some discoloration of teeth. Originally Listerine was the most commonly used mouthwash to prevent plaque buildup, but research into other types of mouthwashes lead to the use of chlorhexidine as a form of treating periodontist and gingivitis, as it was found to be the most effective in reducing plaque and gingivitis [1].
Mechanism of Action
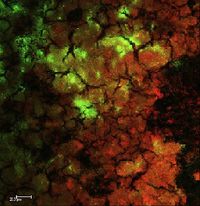
Chlorhexidine is an antimicrobial agent that alters the composition of microorganisms. Chlorhexidine reduces the proportions of some microorganisms which are especially sensitive to this substance. Chlorhexidine works by altering the metabolic activity of bacteria. In lower concentrations Chlorhexidine is bacteriostatic, essentially preventing bacteria from reproducing, and prompts both changes in functioning of the cell membrane as well as leakage of the intracellular components. In high concentrations Chlorhexidine acts as a bactericide causing precipitation of the cellular content and inhibits the action of the glycosyltransferase enzyme which is responsible for the accumulation of bacteria on the dental surface and has effects on sugar transport and acid production in oral bacteria.
In one study the effect of chlorhexidine on transport of methyl-β-D-thiogalactoside (TMG) was tested. They tested the effects of different concentrations of chlorhexidine and measured the levels of TMG in Escherichia coli at ten minutes. It was found that as the concentration of chlorhexidine increased so did the inhibition of TMG and the viability of the cells decreased. Never-the-less it was found that 50% of cells survived even after 24 hours of contact with chlorhexidine so the inhibition of transport was not lethal but it does show that chlorhexidine effects the permiability of the membrane.
Effects of Different Forms of Chlorhexidine
Chlorhexidine comes in various forms: solutions (0.12% and 0.2%), gels (1%), and varnishes (1%, 10%, 20%, and 35%).
Solutions
Rinsing with 0.12% and 0.2% Chlorhexidine solutions showed a significant decrease in Streptococci mutans after 24 hours. On the other hand rinsing with Chlorhexidine mouthwash solution did not produce any long term effects on Streptococci mutans. Only one of the solutions, 0.12% Chlorhexidine, had a lasting effect on salivary Streptococci mutans levels after six weeks of treatment. Treatments using 0.12% Chlorhexidine solutions for 1 or 2 weeks, with 1 or 2 rinsings each day, did not produce any significant long-term reduction in salivary Streptococci mutans. Neither did increasing the Chlorhexidine concentration to 0.2% and the treatment period to 4 weeks. The randomized and controlled studies showed that rinsing with a Chlorhexidine mouthwash solution had no long-term effect on salivary Streptococci mutans.
Gel
Chlorhexidine gel at 0.2%, 0.5%, 1% , and 5% were studied. Of these gels 0.2%, 0.5%, and 1% were applied with a toothbrush, while 1% and 5% gels are applied through professional prophylaxis and trays. Chlorhexidine gel significantly decreased Streptococci mutanslevels for a period of 4-26 weeks after intense treatment which included 3-4 daily applications for 2 days or through daily applications for periods of 10 and 14 days.
Varnish
Chlorhexidine varnish displayed large variations in the level and length of decreased Streptococci mutans. Depending on the subject the decrease in Streptococci mutans could last for 3 days to 2 weeks. Also the greater the concentration the greater the decease level in Streptococci mutans.
Varnish vs Gel
Chlorhexidine varnish and gel were the most effective out of the three types of chlorhexidine studied. Out of the two chlorhexidine varnish was found to be more effective than the gel.
Alternatives to Chlorhexidine
Though chlorhexidine is an effective way of treating periodontal diseases it does have negative side effects namely bad odor and a slight staining in teeth. There have studies that found alternatives which work just as well as chlorhexidine without the negative effects.
Triphala mouthwash
Triphala is a combination of three different plant extracts used in a mouthwash to treat diseases because of its antimicrobial and antioxidant properties. Triphala was found to be as effective as 2% chlorhexidine in treating plaque.
Terminalia chebula
The plant extract of Terminalia chebula was compared with chlorhexidine to see if it would be a good alternative to treat dental caries, gingivitis and stomatitis. There was a significant decrease in plaque in both the chlorhexidine group and Terminalia chebula. There was no significant difference between both group and both reduced plaque buildup and gingivitis. <br
References
1 Adams, D., and M. Addy. "Mouthrinses." Advances in Dental Research 8.2 (1994): 291. Web.
2Gupta, Devanand, et al. "Effect of Terminalia Chebula Extract and Chlorhexidine on Salivary pH and Periodontal Health: 2 Weeks Randomized Control Trial." Phytotherapy Research 28.7 (2014): 992-8. Web.
3 Naiktari, RS, et al. "A Randomized Clinical Trial to Evaluate and Compare the Efficacy of Triphala Mouthwash with 0.2% Chlorhexidine in Hospitalized Patients with Periodontal Diseases." JOURNAL OF PERIODONTAL AND IMPLANT SCIENCE 44.3 (2014): 134-40. Web.
4 Ribeiro, Luciana Gazaniga Maia, Lina Naomi Hashizume, and Marisa Maltz. "The Effect of Different Formulations of Chlorhexidine in Reducing Levels of Mutans Streptococci in the Oral Cavity: A Systematic Review of the Literature." Journal of dentistry 35.5 (2007): 359-70. Web.
Edited by (Martha Serrano), a student of Nora Sullivan in BIOL168L (Microbiology) in The Keck Science Department of the Claremont Colleges Spring 2015.
