Free Fatty Acids as antibacterial agents against several super pathogens including MRSA
Introduction
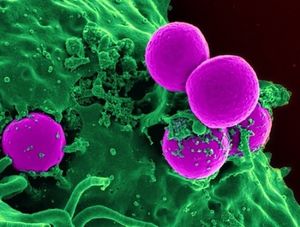
Over the past century, modern science has been overusing and misusing antibiotics, leading to the evolution of many “super pathogens”, or microbes that are resistant to most of the common antibiotics and other methods normally used to treat them. Bacteria and viruses that evade modern treatment through mutation and resistance are health dangers to hospital patients as well as community members. Staphylococcus aureus is a bacterium that colonizes the human nose and skin that is an opportunistic pathogen, meaning that it can live peacefully on a body until the opportunity presents itself where it can initiate an infection in the host. However, overuse of antibiotics has led to the mutation of this pestering bacteria to the super pathogen that is MRSA, Methicillin Resistant Staphylococcus aureus . MRSA cannot be treated with an entire class of common antibiotics called beta-lactams (which include penicillin and methicillin among others) [5], and now, even the most potent “last line of defense” antibiotic, vancomycin, is ineffective on some strains of MRSA (VRSA, for vancomycin resistant Staphylococcus aureus). There are many of these pathogens-named super pathogens-that have developed resistance, including Clostridium difficile, several Enterococcus species including E. avium, along with many others.
These super pathogens demand alternate treatments from the scientific community, preferably treatments that pathogens cannot mutate around by developing resistance. Another solution might be to find treatments that would be used instead of antibiotics for non-threatening pathogens, and therefore prevent mutation/resistance in all bacteria. This would reduce the need for more potent antibiotics because super-pathogens would not evolve as quickly. A promising lead is surprisingly, something that is already in high abundance on our own skin: fatty acids. The fatty acids found in abundance in human sebum are essential for defense against pathogens, and in healthy individuals, are a sufficient barrier to gram positive harmful bacteria. Commercially, fatty acids are used to treat acne (which is also caused by bacteria) and some companies even claim they prevent aging. Other fatty acids that do not naturally occur on our skin, are in many of the foods we eat, such as coconuts. Surprisingly, the potential benefits to using fatty acids as antimicrobials have been hinted at and studied for decades, but they have not achieved wide usage in the medical field.
At right is a sample image insertion. It works for any image uploaded anywhere to MicrobeWiki. The insertion code consists of:
Double brackets: [[
Filename: Ebola_virus2.jpg
Thumbnail status: |thumb|
Pixel size: |300px|
Placement on page: |right|
Legend/credit: Electron micrograph of the Ebola Zaire virus. This was the first photo ever taken of the virus, on 10/13/1976. By Dr. F.A. Murphy, now at U.C. Davis, then at the CDC.
Closed double brackets: ]]
Other examples:
Bold
Italic
Subscript: H2O
Superscript: Fe3+
About Free Fatty Acids
Include some current research, with at least one figure showing data.
History of Fatty Acids as Antimicrobial Agents
Include some current research, with at least one figure showing data.
Bactericidal Effects of Fatty Acids on Methicillin Resistant and Susceptible Staphylococcus aureus
Include some current research, with at least one figure showing data.

Conclusion
References
[1] Wikimedia. NIH.
[6] http://www.niaid.nih.gov/topics/antimicrobialResistance/Examples/mrsa/
Authored for BIOL 291.00 Health Service and Biomedical Analysis, taught by Joan Slonczewski, 2016, Kenyon College.
