Gut-Brain Axis
Introduction
The gut-brain axis is the bidirectional and biochemical signaling system between the central nervous system (CNS) and the gastrointestinal tract (GI tract). (1) In broad terms, the gut-brain axis consists of the central nervous system, sympathetic and parasympathetic branches of the autonomic nervous system (including the enteric nervous system and the vagus nerve), neuroendocrine and neuroimmune systems (including the hypothalamic-pituitary-adrenal axis), and the gut microbiota. (3)
Historically, one of the first gut-brain interactions was observed by Ivan Pavlov when he demonstrated the cephalic phase (the gastric secretion before food enters the stomach) of digestion, showing the relationship between the sight and smell of food to physiological reactions. (10)
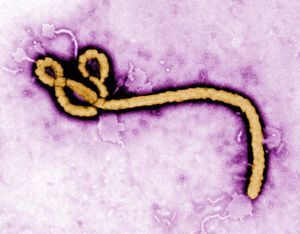
At right is a sample image insertion. It works for any image uploaded anywhere to MicrobeWiki. The insertion code consists of:
Double brackets: [[
Filename: PHIL_1181_lores.jpg
Thumbnail status: |thumb|
Pixel size: |300px|
Placement on page: |right|
Legend/credit: Electron micrograph of the Ebola Zaire virus. This was the first photo ever taken of the virus, on 10/13/1976. By Dr. F.A. Murphy, now at U.C. Davis, then at the CDC.
Closed double brackets: ]]
Other examples:
Bold
Italic
Subscript: H2O
Superscript: Fe3+
Gut Flora
Include some current research, with at least one image.
The gut flora is the aggregate community of microorganisms that live in the digestive tract of humans and other animals. In humans, the gut flora is established only one or two years after birth -- In fact, the gut flora is required for the maturation and development of the intestinal epithelium, the intestinal mucosal barrier, and the immune system of the host. The types of bacteria that develop in the GI tract affects the properties of the mucosal layer, promote the development of the lymphatic system, and regulates the activation and differentiation of various lymphocyte populations and balances the production of immunoglobulin A (IgA) and other peptides essential for their antimicrobial properties. (5)
There is a question of whether the microbiota in the gut is a result of parasitism, commensalism, or mutualism. Co-evolution of the microbiota and the human gut has predetermined that the relationship between the two is a long-term symbiotic relationship, rather than merely a commensal one. In the human gut, the host-microbiota relationship is a prime example of mutualism to the extent where humans are dependent on the bacteria that live in the gut. Because of this, the gut microbiome can be viewed as an extended organ of the host. (2) The human gut flora and GI tract have co-developed in a way that humans are not only tolerant to, but even supportive of these microbes enhancing humans’ digestive and immune systems. (5)
In the body, each specific area is dominated by a specific phyla of microbiota. In the GI tract, specifically, it is dominated by Bacteroidetes and Firmicutes. (2) In humans specifically, the gut microbiota has more species of microbes and a higher proportion of them than in any other area of the body. (4) There is an uneven concentration of microbiota within each specific part of the body. In the human GI tract, from the stomach to the small intestine to the colon, the types of microbiota and quantities of them increase. (2)
Traditionally, the gut microbiome has three major functions. First, it defends against any pathogen colonization by competing for nutrients the host consumes, and it also produces anti-microbial substances. Second, it fortifies the intestinal walls (intestinal epithelial) and induces secretory IgA (sIgA) to limit the bacteria from permeating into the tissues. Third, the gut microbiome facilitates nutrient absorption by metabolizing dietary compounds that the host cannot break down on its own. With this in mind, animals with no microbiome (germ-free) have an increased susceptibility to infection, reduced abilities to digest a wide variety of nutrients, and decreased muscle wall thickness. (2)
Sample citations: [1]
[2]
A citation code consists of a hyperlinked reference within "ref" begin and end codes.
Enteric Nervous System
Include some current research, with a second image.
The enteric nervous system is a subdivision of the autonomic nervous system, which is located in the GI tract. Many neurophysiologists call this a “second brain” because the enteric nervous system is able to endorse function on its own, and it also communicates with the central nervous system (CNS) through the parasympathetic and sympathetic branches of the nervous system. The enteric nervous system communicates with the parasympathetic branch through the vagus nerve and the sympathetic branch through the prevertebral ganglia. Studies have shown that when vertebrate vagus nerves are severed, the organism’s enteric nervous system still functions due to neuroplasticity and regeneration. (6)
The enteric nervous system includes the neurons that are embedded within the walls of the entire gut, ranging from the esophagus to the rectum. It is very important for regulating the function of the gut, some of which include: absorption, digestion, and peristalsis. The enteric nervous system consists of the same neurons as the other branches of the nervous system which include the afferent, efferent, and interneurons. (7)
Over 25 neurotransmitters have been identified to be used by enteric neurons. Only about seven of them are considered to be primary neurotransmitters. This means that they are highly conserved and that the same neurotransmitter will be equally as functional by the same neuron in different regions of the enteric nervous system. Among the seven primary neurotransmitters, acetylcholine is the primary neurotransmitter of the vagus nerve and the pelvic preganglionic neurons, interneurons, secretomotor neurons, and of the motor neurons in the enteric nervous system. Tachykinins and serotonin are another primary neurotransmitter in the enteric nervous system as they are primarily involved in the sensory neurons in the neuronal synapses. (9) In fact, over 90% of the body’s serotonin is found in the GI tract, and over 50% of the body’s dopamine lies throughout the enteric nervous system. (7)
In an experiment done with observing the types of neurons in guinea pig small intestines, here are the respective proportions of the specific ones found: 12% excitatory circular muscle, 16% inhibitory circular muscle, 25% excitatory longitudinal muscle, ~2% inhibitory longitudinal muscle, 5% ascending interneurons, 11% descending interneurons, 26% myenteric intrinsic primary afferent neurons, <1% intestinofungal neurons, and an unknown amount of neuroendocrine cells to the gut. (8) It is not quite clear what the specific proportions are in humans, and if guinea pigs are even an accurate model for what the human nerve proportion is. (8)
Associated Disorders
Include some current research, with a second image.
Conclusion
Overall text length should be at least 1,000 words (before counting references), with at least 2 images. Include at least 5 references under Reference section.
References
Edited by [Iris Tang], student of Joan Slonczewski for BIOL 116 Information in Living Systems, 2020, Kenyon College.
