HIV/AIDs in the U.S.: Difference between revisions
Chavezerazoj (talk | contribs) No edit summary |
Chavezerazoj (talk | contribs) No edit summary |
||
| Line 42: | Line 42: | ||
[1] [https://www.aids.gov/= aids.gov. "HIV AIDS 101".] | [1] [https://www.aids.gov/= aids.gov. "HIV AIDS 101".] | ||
[2] [http:// | [2] [http://www.myvmc.com/treatments/antiretroviral-therapy-anti-hiv-drugs/#c2= Virtual Medical Center. "Antiretroviral Therapy (Anti-HIV Drugs)"] | ||
[3] [http://cid.oxfordjournals.org/content/60/suppl_3/ | [3] [http://cid.oxfordjournals.org/content/60/suppl_3/S187.short= Blashill AJ, Ehlinger PP, Mayer KH, and Safren SA. "Optimizing adherence to preexposure and postexposure prophylaxis: the need for an integrated biobehavioral Approach. 2015. Clinical Infectious Diseases 60(S3):S187-90.] | ||
[4] [http:// | [4] [http://cid.oxfordjournals.org/content/60/suppl_3/S200.short= Jain S, Krakower DS, Mayer KH. "The transition from postexposure prophylaxis to preexposure prophylaxis: an emerging opportunity for biobehavioral HIV prevention. 2015. Clinical Infectious Diseases. 60(S3):S2000-4.] | ||
[5] [http://jid.oxfordjournals.org/content/ | [5] [http://jid.oxfordjournals.org/content/203/10/1484.short= Brown KC. et. al. (9 coauthors). "Single and multiple dose pharmacokinetics of maraviroc in saliva, semen, and rectal tissue of healthy HIV-negative Men. 2010. Journal of Infectious Diseases. 203:1484-90.] | ||
[6] [http:// | [6] [http://jid.oxfordjournals.org/content/211/8/1202.short= Grant RM, Liegler T. Weighing the Risk of Drug Resistance With the Benefits of HIV Preexposure Prophylaxis. 2015. Journal of Infectious Diseases. 211:1202-4.] | ||
[7] [http:// | [7] [http://journals.lww.com/jaids/Abstract/2008/02010/Limited_Knowledge_and_Use_of_HIV_Post__and.15.aspx= Liu AY, et. al. (eight coauthors). 2008. Limited Knowledge and Use of HIV Post- and Pre-Exposure Prophylaxis Among Gay and Bisexual Men. Epidemiology and Social Science. 47:241-7.] | ||
[8] [http:// | [8] [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2862268/= Dumond JB. et. al. (ten coauthors). 2007. Antiretroviral drug exposure in the female genital tract: implications for oral pre- and post-exposure prophylaxis. AIDS 21(14): 1899-1907] | ||
[9] | [9] [http://journals.lww.com/aidsonline/Abstract/2015/04240/State_level_structural_sexual_stigma_and_HIV.11.aspx= Oldenburg CE, et. al. (seven coauthors). 2015. State-level structural sexual stigma and HIV prevention in a national online sample of HIV-uninfected MSM in the United States. Official Journal of International AIDS Society. 29(7):837-45.] | ||
[10] | [10] | ||
[11] | |||
<br><br>Authored for BIOL 291.00 Health Service and Biomedical Analysis, taught by [mailto:slonczewski@kenyon.edu Joan Slonczewski], 2016, [http://www.kenyon.edu/index.xml Kenyon College]. | <br><br>Authored for BIOL 291.00 Health Service and Biomedical Analysis, taught by [mailto:slonczewski@kenyon.edu Joan Slonczewski], 2016, [http://www.kenyon.edu/index.xml Kenyon College]. | ||
Revision as of 16:46, 18 December 2015
By J. Sebastian Chavez-Erazo
An Introduction to HIV/AIDs
Human Immunodeficiency Virus (HIV) is a harmful retrovirus that, if left untreated, will lead to Acquired Immunodeficiency Syndrome (AIDS) in humans. HIV works by attacking specific cells in the immune system: CD4 cells or T cells1[2]. HIV destroys these immune system cells enough over time that the body can not protect itself against infections and disease. The final stage of HIV infections is characterized by AIDS where the immune system is damaged enough that it becomes vulnerable to opportunistic infections. An opportunistic infection or a combination of them which then finally are the most likely cause of death in AIDS patients. If left untreated, individuals living with AIDS who are diagnosed with an opportunistic illness have a life expectancy of about one year1[3].
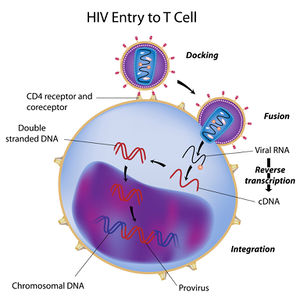
The origin of HIV has been identified as coming from a type of chimpanzee in West Africa where the simian immunodeficiency virus (SIV) was most likely transmitted to humans via contact with chimpanzee blood. SIV then mutated into HIV in human hosts and was transmitted from person to person via bodily fluids (blood, semen, rectal fluids, breast milk etc.) until the virus became spread worldwide over a couple decades. HIV is known to have existed in the United States as early as the 1970’s shortly before the AIDS epidemic of the 1980’s. The mechanism by which HIV infects T cells is similar to most retroviral infections: the virus inserts its viral RNA into the host white blood cell’s nucleus after attaching and has copies of itself made through a process called reverse transcription. In reverse transcription, an enzyme reverse transcriptase makes cDNA copies of the viral RNA using the host cell’s nucleotides which are then integrated into the genome of the host cell where the virus can become active or latent.
Over time, the continued production of HIV in CD4 cells causes AIDS to occur. AIDS is diagnosed in HIV positive individuals by a CD4 cell count. If an individual’s CD4 count falls below 200 cells per cubic millimeter of blood (200 cells/mm3) then they are considered to have AIDS. A typical CD4 count in noninfected adults is between 500 and 1600 cells/mm3. An individual may also be diagnosed with AIDS if they acquire one or several opportunistic infections, regardless of their CD4 count.
Treatment for HIV/AIDS has made leaps and bounds since the devastating AIDs epidemic of the 1980’s. Througout the 80’s and 90’s, an HIV/AIDS diagnosis meant certain death. This was especially true for HIV positive individuals in the queer community who faced not only a lack of medication and treatment but also varying levels of social stigma and discrimination. Among the queer community, those most often affected by HIV/AIDS have been men who have sex with men (MSM), a trend which remains true in the present day. In the 90’s the introduction of antiretroviral treatment (ART) drugs which targeted the enzymes that make the process of HIV replication became available, with varying levels of efficiency and toxicity. It was soon after found that these antiretroviral drugs which inhibit different steps in the HIV replication process, were most effective if used as a cocktail. The use of several ART’s together was found to be most effective because of HIV’s great likelihood to mutate and become drug resistant due to the inefficiency of reverse transcriptase to make exact cDNA copies of the viral RNA. Today, there are four general categories of ARV medications: Nucleoside and nucleotide reverse transcriptase inhibitors (NRTIs), non-Nucleoside reverse transcriptase inhibitors (NNRTI’s), protease inhibitors (PI’s), and drugs that interfere with viral entry such as fusion inhibitors and CCR5 antagonists. While there is still no cure or vaccine for HIV, the main goal has moved from treatment to prevention with the emergence of pre- and post-exposure prophylactic treatments where a daily regimen of a three-drug pill can be taken to decrease risk if HIV infection by up to 90% in high risk individuals. While these drug treatments and preventative measures now exist that make living with HIV/AIDS more like a chronic illness, issues of availability and public education present challenges to the fight against HIV/AIDS.
A Basic explanation of Antiretroviral Treatments
Include some current research, with at least one figure showing data.
Pre-/Post-Exposure Prophylaxis
In recent years, pre-exposure and post exposure prophylactic treatments for populations at high risk for Human Immunodeficiency Virus (HIV) infection have become increasingly studied and emphasized as vital to the decreased transmission of HIV resulting in decreased rates of Advanced Immunodeficiency Syndrome (AIDS) development in differing world populations.
Pre-Exposure Prophylaxis
PrEP has given a specific population the opportunity to have a 90% reduction in the chance of contracting HIV with the use of the daily pill, Truvada (oral emtricitabine (FTC)/ tenofovir disoproxil fumarate (TDF)). The product is said to be available to any person regardless of their sexual and gender identity but in there lies the problem with PrEP, many people who are at high risk of contracting HIV are not receiving it.
.
Post-Exposure Prophylaxis
Include some current research, with at least one figure showing data.
Challenges to HIV/AIDs Prevention and Treatment
The product [PrEP] is said to be available to any person regardless of their sexual and gender identity but in there lies the problem with PrEP, many people who are at high risk of contracting HIV are not receiving it.
Conclusion
References
[2] Virtual Medical Center. "Antiretroviral Therapy (Anti-HIV Drugs)"
[10]
[11]
Authored for BIOL 291.00 Health Service and Biomedical Analysis, taught by Joan Slonczewski, 2016, Kenyon College.
