Microbial Infection of Burn Wounds: Difference between revisions
| Line 11: | Line 11: | ||
==Burn Infections== | ==Burn Infections== | ||
<br>Bacteria and fungi are the most common pathogens of burn wounds. These microbes form multi-species biofilms on burn wounds within 48 – 72 hours of injury [Church]. Organisms originate from the patient’s own skin, gut and respiratory flora, as well as from contact with contaminated health care environments and workers [Church; Murray]. Gram-positive bacteria are some of the first to colonize burns, followed quickly by gram-negative . Fungal infection tends to occur in the later stages after the majority of bacteria have been eliminated by topical antibiotics [Church]. Two bacterial species, methicillin-resistant Staphylococcus aureus (MRSA) and Pseudomonas areuginosas will be examined in depth in this page as they are two of the most prevalent infective agents.<br> | Burn wound infection is problematic because it delays healing, encourages scarring and may result in bacteremia, sepsis or multiple-organ dysfunction syndrome (a.k.a. organ failure) whereby organs from several systems are unable to maintain homeostasis on their own, requiring immediate medical attention [Church].<br> | ||
<br>Bacteria and fungi are the most common pathogens of burn wounds. These microbes form multi-species biofilms on burn wounds within 48 – 72 hours of injury [Church]. Organisms originate from the patient’s own skin, gut and respiratory flora, as well as from contact with contaminated health care environments and workers [Church; Murray]. Gram-positive bacteria are some of the first to colonize burns, followed quickly by gram-negative . Fungal infection tends to occur in the later stages after the majority of bacteria have been eliminated by topical antibiotics [Church]. Two bacterial species, methicillin-resistant Staphylococcus aureus (MRSA) and Pseudomonas areuginosas will be examined in depth in this page as they are two of the most prevalent infective agents. These two species have proven particularly difficult to treat because they posses a large number of virulence factors and antimicrobial resistance genes.<br> | |||
===methicillin-resistant <i>Staphylococcus aureus</i>=== | ===methicillin-resistant <i>Staphylococcus aureus</i>=== | ||
<br> | MRSA are gram-positive, spherical microbes and some of the earliest colonizers of burn wounds. Their genome is contained on one circular chromosome, with antibiotic resistance encoded in transposons. MRSA dwell in the sweat glands, hair follicles and mucous membranes of humans.<br> | ||
===<i>Pseudomonas areuginosas</i>=== | ===<i>Pseudomonas areuginosas</i>=== | ||
<br> | <i>P. areuginosas</i> are the most common source of burn infections [Church]. They are gram-negative rod-shaped cells that possess a single supercoiled circular chromosome. <i> P areuginosas</i> are facultative aerobes capable of fermentation that originate in the human gut. These bacteria are known for their tendency to cause disease in immuno-compromised patients, such as those with AIDS or cystic fibrosis. <br> | ||
==Treatment== | ==Treatment== | ||
Revision as of 06:02, 15 April 2009
By Erin Pienciak
Overview of Burns
Burns are damage to the skin caused by chemicals, electricity, heat, sunlight or nuclear radiation [ ]. Overall burn severity is determined based on the degree of tissue damage and the size of the area affected.
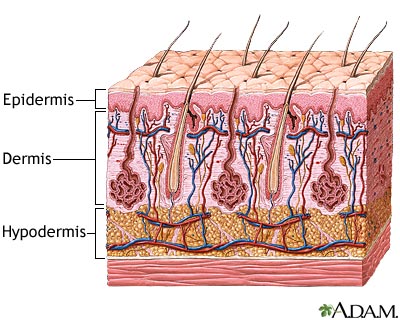
The tissue damage incurred is classified into three categories: first, second and third-degree burns [ ]. First-degree burns involve only damage to the topmost layer of the skin, the epidermis. Second-degree burns contain damage to the epidermis as well the dermis, the underlying layer of the skin. Third-degree burns refer to damage or destruction of the entire depth of the skin as well as tissues that lie beneath it. These are three-dimensional injuries with damage extending in all direction from the center of the injury.
The area of a burn is often determined using the “Rule of Nines,” which divides the body up into sections that correspond with approximately 9% of the body’s surface area [ ]. For example, an arm, the abdomen and the entire head each account for 9%. If all three of these body parts were burned, it would be estimated that the patient sustains injuries to 27% of his body.
Burns wounds have three separate zones of concern. The zone of coagulation is located where the skin came in contact with the burn source, at the center of the wound. It is made up of dead, leathery tissue that forms the burn eschar, or scab. The zone of stasis surrounds the zone of coagulation; tissue is this zone is alive but at a high risk of infection and necrosis due to decreased perfusion to the area. Lastly, the zone of hyperemia surrounds the zone of stasis and contains healthy skin though vasodilatation in this area is common as a result of the injury [Church].
Infection of burns is common because the skin, a physical barrier against microbes, has been compromised. Furthermore, in moderate and severe burns the underlying vasculature of the skin has been damaged or destroyed and so immunity agents, such as T cells, cannot reach sites of infection. Accordingly, the risk of infection increases proportionately with the size of the burn [Church].
Burn Infections
Burn wound infection is problematic because it delays healing, encourages scarring and may result in bacteremia, sepsis or multiple-organ dysfunction syndrome (a.k.a. organ failure) whereby organs from several systems are unable to maintain homeostasis on their own, requiring immediate medical attention [Church].
Bacteria and fungi are the most common pathogens of burn wounds. These microbes form multi-species biofilms on burn wounds within 48 – 72 hours of injury [Church]. Organisms originate from the patient’s own skin, gut and respiratory flora, as well as from contact with contaminated health care environments and workers [Church; Murray]. Gram-positive bacteria are some of the first to colonize burns, followed quickly by gram-negative . Fungal infection tends to occur in the later stages after the majority of bacteria have been eliminated by topical antibiotics [Church]. Two bacterial species, methicillin-resistant Staphylococcus aureus (MRSA) and Pseudomonas areuginosas will be examined in depth in this page as they are two of the most prevalent infective agents. These two species have proven particularly difficult to treat because they posses a large number of virulence factors and antimicrobial resistance genes.
methicillin-resistant Staphylococcus aureus
MRSA are gram-positive, spherical microbes and some of the earliest colonizers of burn wounds. Their genome is contained on one circular chromosome, with antibiotic resistance encoded in transposons. MRSA dwell in the sweat glands, hair follicles and mucous membranes of humans.
Pseudomonas areuginosas
P. areuginosas are the most common source of burn infections [Church]. They are gram-negative rod-shaped cells that possess a single supercoiled circular chromosome. P areuginosas are facultative aerobes capable of fermentation that originate in the human gut. These bacteria are known for their tendency to cause disease in immuno-compromised patients, such as those with AIDS or cystic fibrosis.
Treatment
Burn patients have a uniqe set of requirements when recovering from their trauma. Of the utmost importance is airway, breathing and circulation maintenance. Patients may have sustained inhalation injuries when they were burned and thus could require additional interventions. Hemodynamic homeostasis can also be problematic as a result of disrupted blood flow and fluid loss. Furthermore, the metabolism of burn victims actually increases in response to the injury and so nutritional intake must increase accordingly [Church]. These issues must be addressed before the burn itself can be treated.
Currently, the most widely accepted methods of treatment of moderate and severe burns include wound excision and the application of topical antimicrobial agents [Church]. The presence of the eschar tends to produce localized inflammation. The purpose of excision is to surgically remove the eschar, thereby reducing inflammation and minimizing scaring. The wound can then be debrided, cleansed and closed using a skin graft or a synthetic alternative.
Conclusion
Overall paper length should be 3,000 words, with at least 3 figures.
References
Church, D., Elsayed, S., Reid, O., Winston, B., Lindsay, R. (2006) Burn Wound Infections. Clinical Microbiology Reviews, 19 (2), 403–434.
McVay, C.S., Velasquez, M., Fralick, J.A. (2007). Phage therapy of Pseudomonas aeruginosa infection in a mouse burn wound model. Antimicrobial Agents and Chemotherapy 51 (6), 1934–1938.
Murray, C., Hospenthal, D.R. (2008). "Burn Wound Infections" emedicine 16 Apr 2008. http://emedicine.medscape.com/article/213595-overview (Accessed 6 Apr 2009).
Vorvick, L. (2008). Medical encyclopedia: Skin layers. Medline Plus: a service of the U.S. National Library of Medicine and the National Institutes of Health. http://www.nlm.nih.gov/MEDLINEPLUS/ency/imagepages/8912.htm (Accessed 14 Apr 2009).
Edited by student of Joan Slonczewski for BIOL 238 Microbiology, 2009, Kenyon College.