Microbial Infection of Burn Wounds
Erin Pienciak
Overview of Burns
Burns are damage to the skin caused by chemicals, electricity, heat, sunlight or nuclear radiation [ ]. Overall burn severity is determined based on the degree of tissue damage and the size of the area affected.
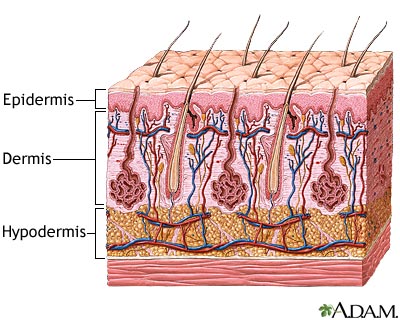
The tissue damage incurred is classified into three categories: first, second and third-degree burns [ ]. First-degree burns involve only damage to the topmost layer of the skin, the epidermis. Second-degree burns contain damage to the epidermis as well the dermis, the underlying layer of the skin. Third-degree burns refer to damage or destruction of the entire depth of the skin as well as tissues that lie beneath it. These are three-dimensional injuries with damage extending in all direction from the center of the injury.
The area of a burn is often determined using the “Rule of Nines,” which divides the body up into sections that correspond with approximately 9% of the body’s surface area [ ]. For example, an arm, the abdomen and the entire head each account for 9%. If all three of these body parts were burned, it would be estimated that the patient sustains injuries to 27% of his body.
Burns wounds have three separate zones of concern. The zone of coagulation is located where the skin came in contact with the burn source, at the center of the wound. It is made up of dead, leathery tissue that forms the burn eschar, or scab. The zone of stasis surrounds the zone of coagulation; tissue is this zone is alive but at a high risk of infection and necrosis due to decreased perfusion to the area. Lastly, the zone of hyperemia surrounds the zone of stasis and contains healthy skin though vasodilatation in this area is common as a result of the injury [Church].
Infection of burns is common because the skin, a physical barrier against microbes, has been compromised. Furthermore, in moderate and severe burns the underlying vasculature of the skin has been damaged or destroyed and so immunity agents, such as T cells, cannot reach sites of infection. Accordingly, the risk of infection increases proportionately with the size of the burn [Church].
Burn Infections
Bacteria and fungi are the most common pathogens of burn wounds. The majority of these microbes come from the patient’s own skin, gut and respiratory flora, as well as from contact with contaminated hospital services and health workers (Church et al, 2006; Murray et al, 2008). Two bacterial species, methicillin-resistant Staphylococcus aureus (MRSA) and Pseudomonas areuginosas will be examined most in depth in this page as they are two of the most prevalent infective agents.
methicillin-resistant Staphylococcus aureus
Pseudomonas areuginosas
Treatment
Include some current research in each topic, with at least one figure showing data.
Conclusion
Overall paper length should be 3,000 words, with at least 3 figures.
References
Church, D., Elsayed, S., Reid, O., Winston, B., Lindsay, R. (2006) Burn Wound Infections. Clinical Microbiology Reviews, 19 (2), 403–434.
McVay, C.S., Velasquez, M., Fralick, J.A. (2007). Phage therapy of Pseudomonas aeruginosa infection in a mouse burn wound model. Antimicrobial Agents and Chemotherapy 51 (6), 1934–1938.
Murray, C., Hospenthal, D.R. (2008). "Burn Wound Infections" emedicine 16 Apr 2008. http://emedicine.medscape.com/article/213595-overview (Accessed 6 Apr 2009).
Vorvick, L. (2008). Medical encyclopedia: Skin layers. Medline Plus: a service of the U.S. National Library of Medicine and the National Institutes of Health. http://www.nlm.nih.gov/MEDLINEPLUS/ency/imagepages/8912.htm (Accessed 14 Apr 2009).
Edited by student of Joan Slonczewski for BIOL 238 Microbiology, 2009, Kenyon College.