Newborn baby digestive tract
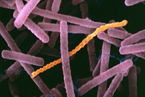
Before birth, the digestive tract of the fetus is sterile, but within hours of birth, the baby acquires a complex collection of microorganisms which populate the mouth—then eventually the full length of the tract will be colonized. The development of specific microorganisms is influenced by the exposure to certain factors such as maternal microbiota, environmental contact, mode of delivery and the infant’s diet.
The Niche: Newborn Baby Digestive Tract
The newborn baby digestive tract includes the esophagus, stomach, small intestine, large intestine, and rectum. Although the mouth is not considered part of the digestive tract, it plays a critical role in food breakdown and provides access for microbes to enter and colonize the infant’s digestive tract. Beyond the mouth, the esophagus serves as a passage for the microbes to progress further down the digestive tract, pass the stomach and into the intestines where the microbes can establish and initiate colonization. The intestinal layer consists of a protective mucus layer, which is made up of glycoproteins that serve as potential attachment sites for the microbes. It is the surface of the mucus at the entrance of the villi, where the microbes are normally found (1). Of all the parts of the digestive tract, the intestines are where the majority of the microflora resides. The microbes can exit the digestive tract through the rectum and the anus via feces.
Physical Conditions
The pH of an infant’s stomach ranges approximately from 2 to 5. Initially the pH of the stomach is less acidic, but the presence of microbes, such as Streptococcus and Lactobacillus, and their metabolic activities create a more acidic environment. However, further down the digestive tract the acidity of the environment decreases (2).
The infant’s stomach is a well-oxygenated area because air swallowed with food arrives in the stomach within moments of ingestion. The facultative anaerobes established in the stomach utilize the available oxygen, resulting in an oxygen-reduced environment for the obligate anaerobic microbes in the intestines (3,4).
Factors Affecting the Microflora Composition
The mode of delivery determines the nature of microbes ingested by the infant. Through normal vaginal birth, an infant is exposed to the mother’s vaginal and fecal flora, which results in the colonization of Lactobacillus, Bifidobacterium, Escherichia coli, and Enterococcus. However, an infant delivered by Caesarian section is exposed to a different assortment of microbes, such as Clostridium and Streptococcus, which are acquired from the tools used. These microbes can establish and colonize rapidly within the sterile digestive tract, because there are no pre-existing microbes to compete with (5,6). Microbes are able to communicate with their environment as well as others by quorum sensing. Quorum sensing serves as a defense mechanism against colonization by new strains of bacteria (1).
The microflora composition of the infant digestive tract is largely influenced by the dietary intake of the infant. For example, in breast-fed infants, Staphylococcus aureus colonies are found. S. aureus is normally transferred from the mother’s nipple during breast feeding as well as through mouth contact. Differences can be observed in the development of microflora between breast-fed and formula-fed infants, which are shown in the table below (7).
| Breast-Fed Infants | Formula-Fed Infants |
|---|---|
| The digestive tract is colonized by primarily Bifidobacteria. | The digestive tract is colonized predominantly of Bacteroides with some Bifidobacteria; but over time the difference in the number of colonies of the two genera decreases. |
| Human milk has antimicrobial factors that lower the growth of facultative anaerobes. | There exists a more complex flora consisting largely of facultative and obligate anaerobes, such as Enterobacteria, Streptococcus and Clostridium. |
| Intestinal lumen is acidified more easily because human milk does not serve as an efficient buffer. | Intestinal lumen is closer to a neutral pH. |
| Infants are less prone to infections due to a large amount of Bifidobacteria. | Infants are more prone to infections due to the lower amount of Bifidobacteria. This can result in a higher risk of diarrhea and allergies. |
Microbial Diversity
Bifidobacterium
Bifidobacterium species colonize in great numbers in the infant digestive tract, regardless if the infant is breast-fed or formula-fed (8). The most common Bifidobacterium species in infants are Bifidobacterium infantis, Bifidobacterium breve, and Bifidobacterium longum. However, Bifidobacterium infantis is specifically unique to the infant’s digestive tract (9). They are gram-positive microbes and are oxygen intolerant; hence, they colonize within the intestines rather than the stomach since the intestines are not well-oxygenated regions like the stomach. Being Gram-positive bacteria, Bifidobacterium infantis have a thick cell wall for extra protection from other residing microbes within the intestines.
Oligosaccharides such as N-acetylglucosamine, glucose, galactose, and certain glycoproteins composing human milk are potential growth factors for Bifidobacterium. A rough range of 50%-90% of human milk oligosaccharides pass through infants undigested. Bifidobacterium is able to break down these undigested sugars and obtain energy and nutrients for growth (10). Bifidobacterium infantis prefer glucose over other oligosaccharides due to the availability and abundance of glucose as well as the lower level of difficulty for them to metabolize glucose. They situate themselves by associating with the intestinal wall, either directly attaching to the epithelium or entrapping themselves in the mucous layer of the epithelium. By situating themselves here, they are able to be in an environment that can help in their metabolic activities. With the assistance of intestinal peptidases such as alpha-glutamyl transpeptidase, aminopeptidase, oligoaminopeptidase, and carboxypeptidase, the food ingested by the infant can be broken down further for the microbe to access and utilize essential components more effectively (2). Effective digestion by the intestinal peptides and hormones within the environment, allows for the microbe to lower their energy expenditure by down-sizing the load and complexity of the essential components.
Increased colonization of Bifidobacterium in the large intestine, and its interaction with Lactobacilli, results in enhanced carbohydrate fermentation (11). Fermentation results in an increased production of acetic acid, butyric acid, and lactic acid, which creates an acidic barrier against pathogenic bacteria. Bifidobacterium infantis interacts with Lactobacillus salivarius to exert immunomodulatory effects on intestinal immune cells that mediate host responses to flagellin and pathogens. They are able to modulate the intestinal epithelium by making Salmonella typhimurium less virulent as well as weakening flagellin-induced pro-inflammatory responses (12). Both species interact to down-regulate the secretion of basal IL-8, but Bifidobacterium infantis specifically inhibits flagellin-induced IL-8 secretion. Flagellin serves as a key activator of pro-inflammatory responses to specifically Salmonella intestinal epithelial cell responses (12). The major point to understand from this is that Bifidobacterium infantis interacts with Lactobacillus salivarius to modulate intestinal epithelial cell responses by limiting IL-8 secretion. While they are interacting to weaken pro-inflammatory responses, they may encounter other microbes such as Bacteroides vulgatus that activate pro-inflammatory gene expression in intestinal epithelial cells (12).
Lactobacillus
Lactobacilli are Gram-positive rods that can be found throughout the digestive tract, but is predominantly present in the large intestine (13). They can infiltrate an infant’s sterile digestive tract by means of contact with the mucosal surface of the mother’s vagina or from the mother’s breast milk (14). Lactobacilli are second only to Bifidobacteria in dominating the microbiota of breast-fed infants. The most common species of Lactobacillus found in infants is Lactobacillus acidophilus (11). Lactobacilli contribute to digestion, stimulate the immune system, and inhibit the growth of pathogens (15). They live in habitats rich in carbohydrates, such as an infant’s digestive tract. Lactobacilli, a member of the lactic acid bacteria group, break down sugars, mainly lactose, into lactic acid using the enzyme β-galactosidase. Sugar metabolism provides nutrients and energy for its growth and survival (3, 13). The accumulation of lactic acid lowers the environmental pH, which inhibits the growth of pathogenic bacteria, such as Helicobacter pylori. Lactobacilli can regulate their enzymatic activity to achieve a more suitable or optimal living condition. They can also inhibit growth of other bacteria by competing with them for nutrients and adhesion sites on the epithelial lining of the intestinal wall (3). Lactobacilli are commonly used as probiotics, supplements containing bacteria that are beneficial to humans (11, 13).
Clostridium
Clostridia are Gram-positive, spore-forming, obligate anaerobes. Many species of Clostridium are potentially pathogenic, due to their ability to form toxins and spores (16). Birth by Caesarian section and a formula-based diet increases colonization of Clostridia in an infant’s gut. Clostridia thrive in the anaerobic environment of the intestines, where they can multiply in great numbers and produce toxins (16). However, if the environment becomes unfavorable, such as when nutrient availability is low, they can often survive by sporulating. Forming spores is beneficial for the microbes, because by forming them, the microbes can withstand harsh conditions for long periods of time. Then, when the surrounding becomes more favorable, they can proceed into germination and start reproducing again (17).
The most common Clostridium species found in an infant’s gut is Clostridium difficile. Clostridium difficile can colonize in large numbers in the intestines, increasing the production of toxins. These toxins are what causes diarrhea in infants (18). Mass colonization of Clostridium difficile can be life-threatening to especially infants who are taking antibiotics, because the antibiotics can target potential C. difficile competitors, reducing their colonies. A reduction in their competitors can increase their chances of producing toxins as well as other activities. Another species, Clostridium botulinum, can also be found in the infant digestive tract, but only in infants with botulism (17).
Streptococcus
Streptococci are spherical, Gram-positive, facultative anaerobic bacteria found in the neonatal intestinal tract. It is one of the initial microbes that colonize the digestive tract after birth. This anaerobe utilizes the oxygen present creating a reduced environment which allows for growth of obligate anaerobic bacteria (3). Streptococci also ferment sugars into lactic acid. Streptococcus agalactiae is known as Group B Streptococci (GBS) and is known to cause meningitis and sepsis in infants (19).
Escherichia coli
Escherichia coli is a Gram-negative, facultative anaerobic, and non-sporulating bacterium that generally reside in the infant's intestines (20). E. coli is one of the first and most abundant bacteria that colonize the intestines. The growth of E. coli is suppressed when human milk is present in the digestive tract, because the proteins present in the human milk create a hostile environment for E. coli. The majority of E. coli produces K- and B-complex vitamins in the intestines, which are absorbed by the infant's body as essential nutrients (20). However, different E. coli strains have different functions. Some E. coli strains collaborate with other bacteria to breakdown and obtain nutrients. In specific, the E. coli strain Nissle 1971, stimulates lymphocytes to secret IgA, which protects the intestinal epithelial cells from enteroinvasive bacterial pathogens (21). In contrast, E. coli strain O157:H7, which is normally not found in healthy infants, is incapable of surviving in the intestines due to the intestines' concentration of bile salts. However, this specific strain can modify its surrounding by inducing the reduction of water and salt present within the intestines. Such reduction can cause severe damage in the intestinal epithelial cells, resulting in death of bacteria that reside in the intestinal epithelium as well (22).
Bacteroides
Little is known of the function of Bacteroides; however, their way of establishment is somewhat evident. It has been studied that the presence of Bifidobacteria stimulates the diversity of sugars that the Bacteroides can degrade for nutrient and energy. Several host genes that are involved in innate immune response of the infant was induced by Bacteroides. A specific species of Bacteroides, Bacteroides fragilis, is able to enhance the function of various T cells, which are involved in immune response (23).
Current Research
To define the microbial ecology within the infant digestive tract that exists today involved many years of research. Studies have shown that human adults have specific microbes living in their digestive tract, but one question remained unanswered- how did the microbes get there? In order to answer this question, a long journey of studying the infant digestive tract began. Even today, establishing the microbial make-up of the infant digestive tract is ongoing. Various microbes have been found, but their specific activities and influences on the infant are not fully known. It has been evident that microbes within the digestive tract are essential for neonatal nutrition, metabolism, and health; however, how the microbes are doing this as well as what they are using is still a mystery. Fortunately, more molecular biological methods are being developed as well as dietary supplements that are increasingly being applied to study the microbial ecology of the infant digestive tract. Below are some of many ongoing researches on newborn baby digestive tract.
Probiotics and Prebiotics
Differences in adult digestive tract microflora and that of the infant are evident, but what factors are involved in causing the change are still being studied. The possibility that dietary supplements may influence the microflora composition in the infant's digestive tract has been raised, and probiotics and prebiotics are helpful for conducting such research.
What are probiotics and prebiotics?
Probiotics are live microbial food supplements that beneficially affect the host by improving its intestinal microbial balance. Probiotics are useful and effective in conducting research only if the following conditions are met (3):
- must exert a beneficial effect on the host
- must be non-pathogenic and non-toxic.
- must have large number of viable cells
- must be able to survive and metabolize in the digestive tract, especially the intestines
- must stay viable during storage and use
- must be capable to isolate from the same species as its intended host
Prebiotics are non-digestible food ingredient that beneficially affect the host by selectively stimulating the growth and the activity of specific number of bacterial species already residing in the intestines. Prebiotics are useful and effective in conducting research only if the following conditions are met (3):
- not hydrolyzed or absorbed in the upper part of the digestive tract
- must be a selective substrate for microbes present in the intestines
- selective substrate must stimulate growth of microbes and provide energy for microbes
- must be able to alter microflora composition to that of a healthier one
Probiotics Used for Bacteriotherapy
Several studies have been conducted using probiotics. The main question in this study is to see if probiotics given to infants can be utilized as bacteriotherapy. For example, will probiotics of specific bacterial strain be effective in reducing or preventing activities of other bacterial species? In other words, can probiotics modulate or influence microbial ecology of the infant's digestive tract?
Several factors were established and were used as the baseline for this study. Robinson and Thompson showed in their study that Lactobacillus acidophilus supplement given to formula-fed infants was thought to improve weight gain (24,25). Another study showed that Lactobacillus casei promoted recovery from acute diarrhea in children (24,25). With these two results as well as the fact that infantile diarrhea is caused by Escherichia coli, Salmonella, and Shigella, Gonzalez et al used a mixture of both Lactobacillus species. This mixture would be used as bacteriotherapy against the three diarrhea-causing microbes (26).
The results showed that Lactobacillus casei in conjunction with live oral rotavirus vaccine to infants, resulted in an elevated response in rotavirus-specific immunoglobulin M-secreting cells as well as an improvement in function of antirotavirus immunoglobulin A seroconversion (24,25). The other strain, Lactobacillus acidophilus, was involved in immune response, of which it was effective against bacterially induced gastroenteritis. The compilation of all the observations made throughout the study, as well as the results above, shows that the probiotics containing the two Lactobacillus strains (L. acidophilus and L. casei), definitely helped modulate the infant microflora. This can be seen by the probiotics reducing gastroenteritis; thus, decreasing the number and their activities of the diarrhea-causing microbes in infants (E.coli, Salmonella, and Shigella). Overall, the probiotics reduced diarrhea and gastroenteritis in infants (24-26).
Prebiotic Supplemented Infant Formula
A study was done to compare a standard formula with prebiotics and one without prebiotics. The purpose of this comparison was to see if prebiotics can influence the microflora of infant digestive tract. It is known that probiotics influence the infant's microecology, but this study will determine whether or not prebiotics will do so as well. Using prebiotics differs from using probiotics because prebiotics are non-digestible whereas probiotics are metabolized. The prebiotics used in this study contained a combination of long-chain fructo-oligosaccharides and trans galacto-oligosaccharides (GOS/lcFOS). The formula with the prebiotics serves as the variable, and the standard formula without the prebiotics serves as the control. Any resulting changes from the two can be potential evidence for prebiotic influence (27).
The results show that prebiotic supplemented formula is responsible for an increase in Bifidobacteria and a decrease in Clostridia. Observations show that the enhanced formula reduces the pH of infants’ stool, compared to formulas without prebiotics. The pH observed in the infants given the prebiotic supplemented formula is similar to that of breast-fed infants. This similarity in stool pH indicates that there is an increased growth of bifidobacteria as well as other beneficial bacteria. The increased growth of bacteria leads to the conclusion that prebiotics do influence the microflora of the infant digestive tract (27).
Probiotics Administered to Expecting Mothers
Many researchers are interested in finding out whether giving probiotics to pregnant women would have an effect on their infant’s gut microflora. It is noted that maternal microflora are a major factor in the establishment of the infant gut microflora. Genera found in the maternal feces, such as bifidobacteria, enterobacteria, and lactobacilli, were also found in the infant feces. In their research, they found that mothers who consumed a probiotic product containing Lactobacillus rhamnosus strain GG, passed on this strain to their infant through exposure to maternal feces during vaginal delivery. Using pulsed field gel electrophoresis (PFGE) to examine DNA digests, researchers were able to differentiate between the different Lactobacillus strains in both the mother's and infant’s feces. They observed only a small amount of Lactobacillus rhamnosus strain GG in the infant’s feces compared to other lactobacilli species. Researchers also noted that Bifidobacteria remained a dominant and important factor in the infant’s digestive tract. They concluded that probiotics can be transferred from the mother to infant, and they may be a healthy boost to an infant’s microflora. This study leads to the conclusion that probiotics given to mothers are important, but they will be more effective if a different strain is used. Since Bifidobacteria play an important role in infants as well as are present in great numbers, they are potential species of many, to further the research of probiotic affect on infant digestive tract microflora (28).
Nutritional Modulation in Infant Formula
The health of the microflora plays an important role in the overall health of the infant’s digestive tract; therefore, nutritional modulation has been the foundation for recent studies. Human milk has many nutritional components essential to the infant. The role of compounds such as human milk oligosaccharides, protein, peptides and nucleotides have yet to be fully discovered. However, it is known that proteins such as lactoferrin, have shown bifidogenic properties which are beneficial to the infant. Scientists are trying to develop formulas that closely resemble human breast milk by isolating the important molecules present in the milk. It is also important to take note that adding nucleotides and other proteins to the formula changes its amino acid composition; therefore, testing the product is crucial (7).
Nucleotides are the building blocks of life, and they play an important role in many biological processes. In the early stages of infant development, introducing nucleotide supplements can be beneficial, especially to the intestinal microflora. Although the exact processes on how the nucleotides affect the individual microbes is not known, there has been evidence that introducing nucleotide supplements results in a higher number of Bifiobacteria, but a lower number of enterobacteria in the infant intestines. (7)
Concluding Thoughts
Although there are many questions that need to be answered regarding the microflora of the infant digestive tract, the resources that are present today limit our abilities to further extend necessary research. The problem with studying the microflora in the infant digestive tract is that the tract is composed of a large number of diverse anaerobic bacteria that cannot be cultivated in lab, whether the media is selective or non-selective for certain species. The fact that the majority of the microbes present in the tract are anaerobic makes it even more challenging for extensive research. Culturing anaerobic bacteria is a slow process, and this limits studies of population dynamics (6). Various molecular biological methods are being developed and used to study the microbial ecology of the infant’s digestive tract. An example of a method is denaturing gradient gel electrophoresis analysis (DGGE), which is used to study complex bacterial communities in various environments. DGGE is very useful because it makes it possible for researchers to identify microbes that represent even the smallest percentage (~1%) of the total population in the human gut (6). However, DGGE cannot cover every aspect of studying microbial ecology of the infant’s gut. Although colonization of microbes of the infant’s digestive tract at birth have been established through a great amount of research, little is known about bacterial stability from day to day, as well as their possible involvement in causing or preventing an illness or death. Even with the established microbes, there are more to be discovered about them--their functions, their interactions, their metabolism, their roles in diseases, and so forth. In other words, the microbial ecology of the infant digestive tract is yet to be unraveled!
References
(1) Neu J, Douglas-Escobar M, Lopez M. (2007) Microbes and the Developing Gastrointestinal Tract. Nutrition in Clinical Practice, 22:174-182.
(2) Berseth CL, Thureen PJ, Hay WW. (2006) Development of the gastrointestinal tract. Neonatal Nutrition and Metabolism. 2:67-73.
(3) Parracho H, McCartney A, Gibson G (2007) Probiotics and prebiotics in infant nutrition. Proceedings of the Nutrition Society, 66:405–411.
(4) Penders J, Thijs C, Vink C, Stelma F F, Snijders B, Kummeling I, van den Brandt P A, Stobberingh E E. (2006) Factors Influencing the Composition of the Intestinal Microbiota in Early Infancy. Pediatrics, 118:511-521.
(5) Favier CF, De Vos WM, Akkermans AD. (2003) Development of bacterial and bifidobacterial communities in feces of newborn babies. Anaerobe, 9:219-229.
(6) Favier CF, Vaughan EE, De Vos WM, Akkermans AD. (2002) Molecular monitoring of succession of bacterial communities in human neonates. Applied and Environmental Microbiology, 68:219-226.
(7) Mountzouris K, McCartney A, Gibson G. (2002) Intestinal microflora of human infants and current trends for its nutritional modulation. British Journal of Nutrition, 87:405-420.
(8) Palmer C, Bik EM, DiGiulio DB, Relma DA, Brown PO. (2007) Development of the Human Infant Intestinal Microbiota. PLoS Biol, 5:1556-1568.
(9) Matsuki T, Watanake K, Tanaka R. (2003) Genus- and Species- specific PCR primers for the detection and indentification of Bifidobacteria. Current Issues Intestinal Microbiology, 4:61-69.
(10) Ward RE, Niñonuevo M, Mills DA, Lebrilla CB, German JB. (2006) In vitro fermentation of breast milk oligosaccharides by Bifidobacterium infantis and Lactobacillus gasseri. Applied and Environmental Microbiology, 72:4497-4499.
(11) Wall R, Hussey SG, Ryan CA, O’Neill M, Fitzgerald G, Stanton C, Ross RP. (2008) Presence of two Lactobacillus and Bifidobacterium probiotic strains in the neonatal ileum. The ISME Journal, 2:83-91.
(12) O’Hara AM, O’Regan P, Fanning A, O’Mahony C, Macsharry J, Lyons A, Bienenstock J, O’Mahony L, Shanahan F. (2006) Functional modulation of human intestinal epithelial cell responses by Bifidobacterium infantis and Lactobacillus salivarius. Immunology, 118:202-215.
(13) Tannock G W. (2004) A Special Fondness for Lactobacilli. Applied and Environmental Microbiolog, 70:3189-3194.
(14) Fanaro, S, Chierici R, Guerrini P, Vigi V. (2003) Intestinal microflora in early infancy: composition and development. Acta Paediatrica Supplement. 441:48-55
(15) Haarman M, Knol J. (2006) Quantitative Real-Time PCR Analysis of Fecal Lactobacillus Species in Infants Receiving a Prebiotic Infant Formula. Applied and Environmental Microbiology, 72:2359-2365.
(16) Nevas M, Lindstrom M, Virtanen A, Hielm S, Kuusi M, Arnon S S, Vuori E, Korkeala H. (2005) Infant Botulism Acquired from Household Dust Presenting as Sudden Infant Death Syndrome. 43:511-513.
(17) Goonetilleke A, Harris J B. (2004) Clostridial Neurotoxins. Journal of Neutology, Neurosurgery & Psychiatry, 75:iii35-iii39.
(18) Mutlu E, Wroe A, Sanchez-Hurtado K, Brazier J, Poxton I. (2007) Molecular characterization and antimicrobial susceptibility patterns of Clostridium difficile strains isolated from hospitals in south-east Scotland. J Med Microbiol, 56:929-929
(19) Bohnsack J, Whiting A, Gottschalk M, Dunn D, Weiss R, Azimi P, Philips III J, Weisman L, Rhoads G, Lin F. (2008) Population Structure of Invasive and Colonizing Strains of Streptococcus agalactiae from Neonates of Six U.S. Academic Centers from 1995 to 1999. JOURNAL OF CLINICAL MICROBIOLOGY, 46:1285–1291
(20) Park H, Shim SS, Kim SY, Park JH, Park SE, Kim HJ, Kang BC, Kim CM. (2005) Molecular analysis of colonized bacteria in a human newborn infant Gut. The Journal of Microbiology, 43:345-353.
(21) Henker J. (2008) Probiotic Escherichia coli Nissle 1917 versus placebo for treating diarrhea of greater than 4 days duration in infants and toddlers. The Pediatric Infectious Disease Journal, 27:494-498.
(22) Phillips AD, Navabpour S, Hicks S, Dougans G, Wallas T, Frankel G. (2000) Enterohaemorrhagic Escherichia coli O157:H7 target Peyer's patches in humans and cause attaching/effacing lesions in both human and bovine intestine. Gut, 47:377-381.
(23) Turroni F, Ribbera A, Foroni E, van Sinderen D, Ventura M. (2008) Human gut microbiota and bifidobacteria: from composition to functionality. Antonie van Leeuwenhoek, 94:35-50.
(24) Isolauri E, Juntunen M, Rautanen T, Sillanaukee P, Koiula T. (1991) A human Lactobacillus strain (Lactobacillus casei sp. strain GG) promotes recovery from acute diarrhea in children. Pediatrics, 88:90-97.
(25) Isolauri E, Joensuu J, Suomalainen H, Luomala M, Vesikari T. (1995) Improved immunogenicity of oral D 3RRV reassortant rotavirus vaccine by Lactobacillus casei GG. Vaccine, 13:310-312.
(26) Gonzalez SN, Cardozo R, Apella MC, Oliver G. (1995) Biotherapeutic role of fermented milk. Biotheraphy, 8:126-134.
(27) Costalos C, Kapiki A, Apostolou M, Papathoma E. (2007) The effect of a prebiotic supplemented formula on growth and stool microbiology of term infants. Early Human Development, 84:45-49.
(28) Tannock G W. (2004) Can the Gut Microflora of Infants Be Modified by Giving Probiotics to Mothers? Journal of Pediatric Gastroenterology and Nutrition, 38:244-246
Additional Sources
[1] Bergseng H, Bevanger L, Rygg M, Bergh K. (2007) Real-time PCR targeting the sip gene for detection of group B streptococcus colonization in pregnant women at delivery. Journal of Medical Microbiology, 56:223–228.
[2] Bohnsack J, Whiting A, Gottschalk M, Dunn D, Weiss R, Azimi P, Philips III J, Weisman L, Rhoads G, Lin F. (2008) Population structure of invasive and colonizing strains of Streptococcus agalactiae from neonates of six U.S. Academic Centers from 1995 to 1999. Journal of Clinical Microbiology, 46:1285–1291.
[3] Byers, HL. (2000) Isolation and characterisation of sialidase from a strain of Streptococcus oralis. J Med Microbiology, 49:235–244.
[4] Colbourn T, Asseburg C, Bojke L, Philips Z, Welton N, Claxton K, Ades A, Gilbert R. (2007) Preventive strategies for group B Streptococcal and other bacterial infections in early infancy: cost effectiveness and value of information analyses. BMJ, 2-7.
[5] Gonzalez SN, Cardozo R, Apella MC, Oliver G. (1995) Biotherapeutic role of fermented milk. Biotheraphy, 8:126-134.
[6] Macfarlane GT, Gibson GR. (1994) Metabolic activites of the normal colonic flora. Springer-Verlag, 17-52.
[7] Robinson EL, Thompson WL. (1952) Effect on weight gain of the addition of Lactobacillus acidophilus to the formula of newborn infants. J Pediatrics, 41:395-398.
[8] Rotimi VO, Duerdan BI. (1981) The development of the bacterial flora in normal neonates. J Med Microbiology, 14:51-62.
[9] Stark PL, Lee A. (1982) The microbial ecology of the large bowel of breast-fed and formula-fed infants during the first year of life. J Med Microbiology, 15:189-203.
[10] Tojo M, Oikawa T, Morikawa Y. (1987) The effects of Bifidobacterium breve administration on Campylobacter eteritis. Acta Pae-diatr Jpn, 29:160-167.
[11] Thong K, Ling G, Kong L, Theam L, Ngeow Y. (2004) Macrorestriction analysis of Streptococcus agalactiae (group B Streptococcus) isolates from Malaysia. Journal of Medical Microbiology, 53:991–997.
Edited by Coco Chin, Jeremy Dayrit, Hanaah Fannin, Angela Ho, Chon Ieng, Min-jeong Suh, students of Rachel Larsen