Vagina

Introduction to the Vagina Niche
When one first thinks of a vagina, one simply thinks of it as being a passageway for conception, birth, and menstruation. It is the site of deposition of a male's sperm for the purpose of fertilizing a female's egg. When a fetus finally completes gestation, or growth and development inside the mother, the baby must travel through the vagina to reach a new world. When a female reaches reproductive age and starts to ovulate, an unfertilized egg will be disposed of and sloughed out through the vagina. All of this knowledge seems sufficient to fully understand the vagina. However, the vagina is not as simple as one may think. Different conditions in a female's life may give rise to different environmental changes inside the vagina. And during these environmental changes, various microbes, innate and foreign, have the ability to be altered. These alterations have the potential to create adverse effects on the female host. Continue reading to find out more... !
The vagina is located directly anterior to the anus and below the urethral opening. It is a muscular passageway which connects the uterus to the exterior genitals. The vagina is typically 2.5 cm wide and 7 to 9 cm long [1]. Externally surrounding the vaginal opening is the labia minora, which is also known as the inner lips, which then leads into the labia majora, the outer lips. Typically after puberty, the labia majora is covered with hair, otherwise known as mons pubis. All together, the labia minora, labia majora, clitoris, mons pubis, and vestibule is called the vulva. Neighboring parts surrounding the vagina also include the clitoris, urethral orifice, vestibule, and hymen. The clitoris is a hard round organ directly on top of the vulva and encircles and extends into the vagina. This organ is to supply pleasure during sexual intercourse and is at the anterior end joining the labia minora. The urethral orifice lies above the vagina and below the clitoris and functions to excrete urine stored in the urinary bladder. The hymen is a membrane which acts like a flap partially covering the opening of the vagina. Internally the vaginal passageway leads up towards the cervix and connects to the uterus [2].
Physical Conditions of a Healthy Vagina
With an approximate pH value ranging from 3.8 to 4.5, the vagina functions in a relatively acidic environment. The acidity is due to the production of lactic acid by Lactobacillus in the vagina [3]. This pH range is required for a healthy vagina for protection purposes. Any pH value higher than 4.5 potentially leads to serious problems [4]. The vagina is typically at or slightly above normal body temperature. This acidic environment is important to maintain so that certain pathogens can not cultivate in that area. But usually this is not an issue because the acidic environment makes it impossible for the pathogens to survive. It is important to maintain moisture to prevent dryness and irritation [5]. Normal vaginal discharge is needed to serve as a natural protection for the vagina. Mucous secretions from the cervix and vagina, and shedding vaginal cells comprise the normal vaginal discharge [6]. The consistency and amount of vaginal discharge may differ at certain times in a woman's life. Depending on the moment of the menstrual cycle, vaginal discharge may be very fluid or very sticky. The amount of vaginal discharge can also decrease and increase depending on where a woman is in her menstrual cycle [3]. To the left and right of the vaginal opening are two oval shaped vestibular glands, otherwise known as Bartholin glands, which secrete mucous for lubrication purposes. During sexual arousal, these glands also secrete addition lubricants to prevent pain during intercourse [5].
Influence by Adjacent Communities
Anus
For most women, the anus is less than one inch away from the vagina and therefore can create major problems to the vaginal area if a problem occurs. The vagina is a very sensitive area for a woman since it is open to various types of infections. Surrounding communities, such as the anus, can contribute to the infection of a normal vaginal environment and here are the two most common problems:
| Problem | Description |
| Anal Abscess | A tightly packed accumulation of pus near the anus which can be extremely painful. This type of anal infection most commonly arises from bacterial or intestinal debris contaminate the anal gland which creates an infection underneath the skin. Moreover, Anal Abscess can spread bacteria and unwanted microbes to the vagina because of their close proximity's and can infections around or inside the vagina [7]. |
| Anal Fissure | A linear crack or tear in the skin of the anus which can spread all the way to the vagina if serious. This most commonly occurs when a massive, hard stool over-stretches the anal opening and tears the delicate skin between the anus and vagina. Anal Fissures also exposure the underlying muscles between the anus and vagina and unwanted microbes can enter open wounds and increase the chances of infections around the vagina [7]. |
On a more scientific level, since the vagina is in close proximity to the anus, microbes from the anus can easily affect vaginal conditions. Under normal conditions, Lactobacillus is responsible for contributing to the acidity of the vagina. The acidic conditions of the vagina help ward off certain microbes and keep a constant balance of normal vaginal flora. Cocci from the bowel is usually present inside the vagina, but must be kept at a certain ratio compared with the normal vaginal flora. When the vagina lacks Lactobacillus, the now basic environment of the vagina is good for the overgrowth of the cocci bacteria from the anus. This phenomenon is also known Bacterial Vaginosis (BV) [3].
How does the Environment Change?
There are many different conditions in which a vaginal environment changes. Since we have seen the physical conditions of a normal vagina, lets take a look at certain stages and conditions in a woman's life in which these changes occur.
The vagina normally contains different kinds of bacteria that are summed up to be called, normal vaginal flora. Under normal conditions, these flora are in some kind of balance and thus do not create problems for the woman. However, if the balance is disturbed, harmful bacteria will be able to take over [8]. Under normal conditions, the vagina is also constantly an acidic environment. If the environment and pH were to change, consequences occur [3].
| Environmental Changes | Description |
| During Menstrual Cycle | At the beginning of a woman's menstrual cycle, vaginal discharge will seem sticky. Prior to ovulation, the amount of discharge increases and becomes very wet or runny. On the day of ovulation, the most discharge is being produced and secreted. After ovulation, the discharge becomes thicker and the amount gradually decreases [9]. |
| During Pregnancy | During pregnancy, a woman's body will produce more estrogen and progesterone than normal and will trigger an increase in vaginal secretions. A woman's body's blood volume will also rise by 50%. Most of this increase in volume is geared toward the growing fetus in the uterus. This causes the vaginal tissue to be filled with more blood and seem more swollen and tender. A woman may develop vaginal acne due to how swollen and moist the vagina has become [10]. Increase of pH in the vagina is a common cause of vaginal itching during pregnancy [11]. |
| During Menopause | Between the ages of 45 to 55, women experience menopause. During this time, there are fluctuations in the amount of estrogen produced in the body. Also, the pH begins to fluctuate back and forth causing an imbalance [5]. However, the pH levels tend to increase more than decrease meaning the environment becomes more alkaline. Glycogen and lactic acid production also begins to dwindle. Estrogen production assures that the tissues surrounding the vagina retains elasticity and retains moisture. However, when the body stops menstruating, estrogen levels decreases dramatically which ultimately leads to vaginal dryness and irritation especially during intercourse. The pubic hair loses density and volume while the tissues lining the vagina become thinner and loses elasticity. At the same time the labia majora and minora decreases in size as well [4]. |
Microbes Present
Now we will look at some of the microbes that are present in the vagina. Lactobacillus is found in a normal, healthy vaginal environment, whereas Gardenerella vaginalis and Streptococcus can be found in an infected vaginal environment. These are only a few of the many microbes that can be present.
| Microbes | Description |
Lactobacillus
 A picture of the microbe, Lactobacillus, which helps keep a healthy vaginal environment through the production of lactic acid. [2]. |
Lactobacillus is one of the main microorganisms responsible for maintaining a healthy vaginal flora. Its production of Lactic acid contribute to the vaginal acidic environment. There are different strains of Lactobacillus able to colonize the vaginal flora, however, those with maximal adherence to the epithelium such as Lactobacillus acidophilus help against bacterial vaginosis (BV) due to their hydrogen peroxide producing capabilities [12]. Bacterial Vaginosis is caused when there is a lack of Lactobacillus in the vaginal flora, allowing various types of microbes to inhabit the environment leading to complications such as pelvic inflammatory disease and sexually transmitted diseases like HIV. Current research is identifying the best strain of Lactobacillus in order to recolonize a healthy vaginal flora. McLean and Rosenstein studied several Lactobacillus strain in order to identify the best strain able to re-colonize the vaginal flora of women with BV. This strain should be able to produce sufficient hydrogen peroxide, be able to inhibitory activity against BV bacteria, acid production, and have strong adherence ability to the vaginal epithelial cell (VEC). They found two strains of the Lactobacillus acidophilus (61701 and 48101) to have such characteristics [13]. Sha et al. show a correlation between Lactobacillus and BV, however, an inverse correlation with HIV [14]. Furthermore, BV bacteria have been shown to upregulate HIV expression. Therefore, by suntanning a healthy vaginal flora by preventing BV infections, Lactobacillus acidophilus can help combat sexually transmitted diseases. Also, Lactobacillus Hydrogen Peroxide has been shown to have virucidal effects allowing the vaginal flora to have protection against pathogens [13]. |
| Gardenerella vaginalis |
Gardenerella vaginalis is one of the microorganisms that causes an infection of the vagina known as bacterial vaginosis. The infection is thought to be transmitted through sexual activity, but can also be found in women with no cases of sexually transmitted diseases. Douching and using intrauterine devices (IUDs) can also help lead to the cause of BV. When infected, the vagina secrets a gray or yellow discharge, which is often accompanied with a “fishy” smell [15]. Gardenerella vaginalis, along with other bacteria, inhabit the vagina and cause a chemical imbalance. These bacteria outnumber the amount of Lactobacillus found in the vagina, which are beneficial and essential to the vagina [16]. |
Streptococcus agalactiae
 Streptococcus colonizes a healthy woman's vaginal and gastrointestinal tract, which may lead to complications during pregnancy. [4]. |
Group B(Beta) Streptococcus Streptococcus agalactiae is a Gram-positive, beta-hemolytic, opportunistic pathogen which colonizes the vaginal and gastrointestinal/rectal tract of healthy adults by adherence to surfaces of vaginal epithelial cells. The vagina is more frequently colonized than rectal sites in both pregnant and non-pregnant adults. It binds maximally onto vaginal epithelial cells in the acidic pH levels of vaginal mucosa where attachment does not depend on capsular serotype or bacterial viability [17]. Streptococcus agalactiae is acquired by infants born to colonized mothers via vertical transmission in 29-72% of cases by a process involving the bacterium undergoing adherence to vaginal epithelial cells, hemolysis and resistance to mucosal immune defenses such as immunoglobulin A (IgA). Once thought to be pathogens of domestic animals, Streptococcus agalactiae is the leading cause of neonatal sepsis in humans resulting in early-onset infections of pneumonia, septicemia and late-onset infections of meningitis or bacteremia in neonates.[18] Streptococcus agalactiae has a evolutionary relationship between the bacterium and the host. There exists selective pressures for Streptococcus agalactiae interaction with host to establish colonization and ensure transmission to newly susceptible hosts(neonates). Host factors play a significant role in determining the pathogenic potentials of Streptococcus agalactiae [18]. |
Microbe Interaction
Certain microbes like to work together and some like to compete. Here we find microbe interaction with a strain of Lactobacillus known as Lactobacillus acidophilus, which inhibits the growth of the harmful microbe, Gardenerella vaginalis.
Lactobacillus not only helps maintain the acidic environment in the vagina, but also helps prevent infections by competing with pathogenic microbes such as Gardenerella vaginalis and Streptococcus agalactiae. Current research shows inhibition of pathogenic microbes, specifically Streptococcus agalactiae and Gardenerella vaginalis, by vaginal epithelial cell adherence of three strains of human vaginal lactobacilli: ( Lactobacillus acidophilus, Lactobacillus gasseri, and Lactobacillus jensenii) in vitro via receptor competition and co-aggregation to inhibit growth when antimicrobial compounds, such as lactic acid and hydrogen peroxide, are produced [19]. Researchers at the Universidad de Oviedo, Spain postulated that Lactobacillus acidophilus, Streptococcus agalactiae and Gardenerella vaginalis possibly bind the the same receptor molecule with Lactobacillus acidophilus having a higher affinity for the receptor , therefore, displacing Gardenerella vaginalis and Streptococcus agalactiae.
Current research has shown that a type of Lactobacillus, Lactobacillus acidophilus, inhibits the growth of the bacteria Gardenerella vaginalis. Aroutcheva, Simoes, and Faro performed experiments using two different methods in order to determine the effect of Lactobacillus acidophilus on Gardenerella vaginalis. Lactobacillus, an important microbe essential to keeping a healthy vaginal environment. Microbes such as Gardenerella vaginalis, are detrimental to the vaginal environment and could cause infections such as bacterial vaginosis. Lactobacillus acidophilus 160 was isolated from a healthy vaginal microflora, purified, and was then used differently in each experiment. One method required the inoculation of the Lactobacillus acidophilus into defined media, and the other required the growth of the strain in MRS agar. The defined media method showed that the growth of Gardenerella vaginalis was inhibited by substances found in the media in which the Lactobacillus acidophilus was added to. The agar method showed that the growth of Gardenerella vaginalis was inhibited by the bacteriocin, a protein produced by bacteria, that was released from the Lactobacillus acidophilus 160 strain [20].
Effects of Microbes on the Environment
Microbes can be harmful to the vaginal environment, with the exception of the microbe, Lactobacillus. Here we will look at the effects that each microbe has on the environment.
| Microbe | Effect |
| Lactobacillus | Does not change the environment of the vagina, but it does interact with the environment to maintain normal conditions. Lactobacillus produce lactic acid, which help the vagina maintain a normal acidic pH. It works to try and prevent any other microbes from altering its pH by producing a balance of lactic acid to counter any intruding microbes. It also helps secrete a normal vaginal discharge, which mainly helps to keep a clean vaginal environment [21]. |
| Gardenerella vaginalis | Changes the vaginal environment by elevating the pH levels of the vagina. Since Lactobacillus produces lactic acid, which keeps the vagina at a natural pH, the mass amounts of Gardenerella vaginalis outnumber those of the lactic acid, therefore increasing the pH [22]. Gardenerella vaginalis also secretes a gray or yellow discharge from the vagina, which often times has a fishy odor [16]. |
| Streptococcus agalactiae | Regularly inhabit healthy vaginas but under conditions of weak immune systems where there are less antibodies against the bacteriums pathogenicity, harmful effects on the environment and host are exhibited. Streptococcus agalactiae ferment carbohydrates into non-gas products such as acetate. Also, Streptococcus agalactiae are hemolytic meaning that the bacteria lyses red blood cells around colonies. This characteristic makes the bacteria especially harmful to neonates born to colonized women. Streptococcus agalactiae cAMP factor aids hemolysis of red blood cell membranes [18]. In addition, it has been documented that high genital colonization of Streptococcus reported no association between genital symptoms or signs [23]. |
Other Non-Microbes Present
Microbes are not the only things found in a vaginal environment. There are other non-microbes present such as bacteria, fungi, and viruses that can also cause problems to the vagina.
| Non-Microbes | Description |
| Bacteria |
Bacteria consist of only a single cell but are amazingly complex. Bacteria have also been found that can live in temperatures above boiling point and well below freezing temperatures. They "eat" everything from sugar and starch to sunlight, sulfur, and iron. Bacteria have fallen into a category of life known as the Prokaryotes. Moreover, Prokaryotes' genetic material, or DNA, is not enclosed in a cellular compartment called the nucleus. Bacteria along with their microbial cousins the archaea were the earliest forms of life on Earth. They have played a vital role in shaping our planet into one that could support the larger forms of life through the process of photosynthesis. A great example of bacteria in the vagina is Bacterial vaginitis which results in a vaginal discharge. Bacterial vaginitis is caused by bacteria and treatment is usually with antibiotics [24]. |
Fungi
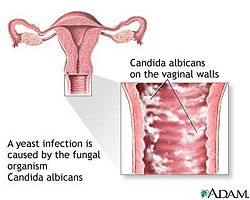 One of the main fungi present in the vagina, known as Candida Albicans, leads to a vaginal infection known as a yeast infection.[5]. |
Fungi are eukaryotic organisms and their DNA is enclosed in a nucleus. Fungi are said to be "plant like", but fungi do not make their own food from sunlight like plants do. Fungi are very useful to humans as they have helped make antibiotics to fight bacterial infections. but can also be deadly that cause diseases and infections. Fungi come in a variety of shapes, sizes, and different types. They can range from enormous chains of cells that can stretch for miles or single individual cells. An example of a fungal infection to the vagina would be a Fungal Yeast Infection [24]. |
| Viruses |
A virus is a small bundle of genetic material (DNA or RNA) that is carried in a shell called the viral coat, or capsid, which is made up of bits of protein called capsomeres. However, viruses cannot metabolize nutrients, produce and excrete wastes, move around their own, or even reproduce unless they are inside another organism's cells. Ultimately, viruses are not even cells yet they have played key roles in shaping the history of life on our planet by shuffling and redistributing genes in and among organisms and by causing diseases in animals and plants. A perfect example of viruses in the vagina is Viral vaginitis that can be caused by herpes simplex virus that is spread by sexual intercourse [24]. |
Wrapping up the Vagina
Now do you have a better understanding of how complex the vagina can be? Conditions of the human vagina differ with changes in life stages (menstrual cycle, pregnancy, and menopause). As conditions change, colonization by microbes commonly found in the vagina also change which can lead to harmful diseases such as bacterial vaginosis and B-streptococcus infections. As you can see, altering the vaginal environment can lead to certain consequences. Thus, it is very important to keep pro-biotic microbes such as Lactobacillus acidophilus present in the vaginal environment because they act to inhibit other microbes that may be harmful to us and even our babies. So remember to eat lots of pro-biotic foods such as yogurts and cheeses to help keep a healthy and infection fighting vagina!
Current Research
Research is still being done to try and figure out more about this microbe niche. Below are a few articles that include: the differing compositions of the vagina in Caucasian and African American women, antibiotic effects on microbes, vaginal conditions during pregnancy, and more.
1. Antibiotic Susceptibility of Atobium vaginae (2006)
Prior studies have shown that anaerobic bacterium, Atopobium vaginae had been closely related with Bacterial vaginosis. There have only been four isolates of this fastidious organism that were found to be highly resistant to metroniadazole and susceptible for clindamycin, two antibiotics preferred for the treatment of Bacterial vaginosis. The research group studied the susceptibility of nine other A. vaginae isolates for 15 antimicrobial agents by using the Etest and for comparison that included a limited number of other important vaginal bacteria such as lactobacilli, Gardenerella vaginalis, bifidobacteria and compared results from previously published articles. The decided method for this particular research involved nine strains of Atopobium vagina, four strains of Gardenerella vaginalis, two strains of Lactobacillus iners and one strain each of Bifidobacterium breve, B. Longum, L. Crispatus, L.gasseri and L. jensenii which were tested against 15 antimicrobial agents using the Etest. The conclusion of this research had shown Clindamycin had a higher activity against Gardenerella vaginalis and A. vaginae than metronidazole, but not all A. vaginae isolates are metronidazole resistant, that seemed to be an apparent conclusion from previous studies on a more limited number of strains. In addition, the research group had concluded Bacterial vaginosis as a polymicrobial disease and the organisms that were involved were likely to be in a symbiotic relationship to each other for various metabolic requirements. In conclusion, clindamycin was shown to dimish the vaginal colonisation resistancere. However, resistance to clindamycin seems to develop more readily than resistance to metronidazole which becomes apparent from clinical studies comparing both antibiotics.
Future studies will focus on determining the antibiotic suseptibility of the vaginal specie that will shed light to develop new regimens for treatment of recurrent bacterial vaginosis. An important note is to make clear whther this metronidazole resistance might be acquired by the presence and activation of nim-genes [25].
2. Differences in the Composition of Vaginal Communities of Caucasian and Black Women (2007)
In essence, all females vagina have the same construct. But the question is whether or not race plays a role. In 2007, researchers from the Department of Biological Sciences at University of Idaho conducted a study to see if and how differences in bacterial communities in the vagina differ from Caucasian and Black women; and how these variations could lead to possible infections. The hypothesis was that there indeed are differences in the composition as well as structure of bacterial colonies the vaginas of Caucasian and Black North Americans.
In this study, 144 Caucasian and Black women from North America who were healthy, menstruating, not pregnant but are capable of becoming pregnant, and are within the reproductive age, had samples taken near the middle of their vaginas with a sterile swab. These samples were then analyzed. The differences in the vaginal communities between the two races were found by investigating the T-RFLPs of 16S rRNA genes. Depending on the similarities of the composition of the communities, different bacteria were divided into groups called supergroups. After much condensing, the researches finally limited the number of supergroups down to 8 which accounted for 94% of the women sampled. The results from this experiment concluded that the kinds of microbes found in the vaginas of Caucasian women and Black women were very different. Lactobacillus was significantly less prevalent in Black women at 68% than those of Caucasian women at 91%. While certain types of anaerobic bacteria was higher for Black women at 32% compared to Caucasian women at only 8%. They found it super suprising that supergroup III, which included communities of Atopobium sp and other anaerobes, were four times as common in Black women as Caucasian. Overall, the hypothesis that there are differences in the composition as well as structure of bacterial colonies the vaginas of Caucasian and Black North Americans proved true. Researches did not stop after they adequately proved this hypothesis.
Recently, studies have been conducted on the appearance of Atopobium in the vaginal of women in their reproductive age and postmenopausal women. From their findings, it suggests that Atopobium is a common vaginal microbe in all healthy women [26].
3. Genome Sequence of Lactobacillus helveticus, an Organism Distinguished by Selective Gene Loss and Insertion Sequence Element Expansion. (2008, January)[13]
Scientists isolated Lactobacillus helveticus, strain DPC4571, from swiss cheese and explored its relationship and similarities with non-dairy lactobacillus strains found in the human GI tract,; specifically Lactobacillus acidophilus strain NCFN. Examination of the complete gene sequences of DPC4571 and NCFN showed conservation of 65-75% of genes and 98.4% of 16S rRNA revealing significant insight for future identification of niche-specific genes [13]. In addition, DPC4571 genome comprised of up to ten times more 213 IS elements in comparison to NCFN indicating the significance of gene loss for colonization in the GI tract. NCFN also has half the amount of PTS system, membrane protiens (cell wall adherence proteins), and sugar metabolism compared to DPC4571 due to selective deletions in the genome.
Sources of such deletions are results of point mutations, horizontal gene transfers and transposons. Such genome differences between the strains provide significant scientific insight into gene roles in pro-biotic genomes and identification of niche-specific genes [27].
4. Changes in the Predominant Human Lactobacillus flora during in vitro fertilisation (2008)
The research done by these Swedish scientists was to characterize the normal cultivable vaginal Lactobacillus flora at varying estradiol levels in plasma. The use of signature matching of nucleotide sequences in the V1 and V3 regions 16S rRNA genes using pyrosequencing technology is a great way for locating vaginal Lactobacilli on the species level and learning more about the vaginal microbial niche. The study was comprised of 17 patients who unerwent ovarian stimulation for In Vitro Fertilization (IVF) whose vaginal status was determined "normal" according to the Ansel and Nugent criteria.
The results of this study showed that 7 out of 10 patients had traces of L. Crispatus, L. Gasseri and/or L. Jensenii. In addition, the remaining 3 women's flora were dominated by L. Rhamnosus or L. Reuteri. However, as their estrogen levels began to rise their flora composition was altered and became dominated by one of the three species that were most common in a healthy vagina.
Future studies on this topic should focus on signature matching of nucleotide sequences in the V1 and V3 regions of 16S rRNA genes. This is a discriminative tool for the study of vaginal lactobacilli and can be used to track the Lactobacillus flora under a wide range of physiological conditions [28].
5. Early Pregnancy Threshold Vaginal pH and Gram Stain Scores Predictive of Subsequent Preterm Birth in Asymptomatic Women (2002)
The purpose of this study was to determine what vaginal characteristics could lead to premature delivery of infants. The vaginal pH and Gram Stain Score was determined and recorded for all women leading to a recorded birth. To determine vaginal pH, ColorpHast Indicator Strips were used. To determine vaginal Gram Stain Score of 0-10, the scientists utilized the Nugent Criteria.
Results showed that women with a pH of 5.0 or higher significantly showed an increased incidence of preterm birth at <37, <35, or <32 weeks of gestation. They also found that there was fewer spontaneous preterm births in women whose pH was 5.0 or lower. Also with the women with pH 5.0 or lower, there was a marked lower incidence of newborns weighing less than 2500g or 1500g at birth.
The results of the Gram Stain Scores supported the results shown by the vaginal pH experiments. Women with a pH of 4.5 or higher acquired a Gram Stain Score of 9 to 10 and were shown to be at a higher risk of preterm delivery. Those with Gram Stain Scores of 0 to 8 were at a lower risk of preterm birth.
Another conclusion pointed out in this study concluded that making alterations to normal vaginal flora is associated with a 2-fold increase in a woman's risk of premature delivery. In summary, disruptions of the normal vaginal flora were able to be determined by looking at a pregnant woman's vaginal pH and Gram Stain Score changes.
Further studies related to this topic can help us reach a firm conclusion of how we can utilize Gram Stain Scores to help diagnose Bacterial Vaginosis. It is said that women afflicted with Bacterial Vaginosis show Gram Stain Scores ranging from 0 all the way to 10. Although Gram Stain Scores and vaginal pH are reliable indicators of a woman's risk for preterm birth, they are not for Bacterial Vaginosis [29].
References
(1) “Female Internal Genital Anatomy.” Gynae Online. http://www.gynaeonline.com/internal_anatomy.htm
(2)“Female External Genital Anatomy.” Gynae Online. http://www.gynaeonline.com/anatomy.htm
(3) "The Vagina." Passion For Life Healthcare Ltd. http://www.biofem.co.uk/vagina.cfm
(4) Gonzaga Florante P. “Symptoms and Treatments of The Menopause.” Geneva Foundation for Medical Education and Research. http://www.gfmer.ch/Books/bookmp/40.htm
(5) Winston, Sheri. “Vaginal Ecology.” Child and Mothering. Volume 4 Number 4. http://www.susunweed.com/herbal_ezine/april04/childbearing.htm. April 2004
(6) "Vaginal Health." Slippery Rock University. http://www.sru.edu/print/13001.asp
(7) "Anal Disorders." Intelihealth. http://www.intelihealth.com/IH/ihtIH/WSIHW000/9339/9396.html
(8) Silverman, Andrew Y. "Minor Vaginal Infections And Bacterial Vaginosis (BV)." HolisticGYN. http://www.holisticgyn.com/vaginal.html
(9) "Ovulation: Signs of Ovulation." Meredith Corporation. http://www.parents.com/getting-pregnant/how-to/ovulation/signs-of-ovulation/
(10) Warnick, Melody. "Vaginal Issues During Pregnancy." Meredith Corporation. http://www.parents.com/pregnancy/my-body/changing/vaginal-issues-during-pregnancy/
(11) Cornfort, Tracee. "Vaginal Itching During Pregnancy." New York Times Company. http://womenshealth.about.com/cs/pregnancy/a/vagitchpregnanc.htm
(12) May A. D. Antonio, Stephen E. Hawes, and Sharon L. Hillier. The Identification of Vaginal Lactobacillus Species and the Demographic and Microbiologic Characteristics of Women Colonized by These Species. The Journal of Infectious Diseases 1999 180:6, 1950-1956.
(13) McLean, N. W., and I. J. Rosenstein. 2000. Characterisation and selection of a Lactobacillus species to re-colonise the vagina of women with recurrent bacterial vaginosis J. Med. Microbiol. 49 543–552.
(14) Beverly E. Sha, M. Reza Zariffard, Qiong J. Wang, Hua Y. Chen, James Bremer, Mardge H. Cohen, and Gregory T. Spear. Female Genital-Tract HIV Load Correlates Inversely with Lactobacillus Species but Positively with Bacterial Vaginosis and Mycoplasma hominis. The Journal of Infectious Diseases 2005 191:1, 25-32.
(15) "Gardnerella, Overview, Causes, Symptoms, Diagnosis, Treatment." KOMO TV. http://ww3.komotv.com/global/story.asp?s=1230125
(16) "Bacterial Vaginosis." National Institute of Allergy and Infectious Diseases. http://www3.niaid.nih.gov/topics/bacterialVaginosis/
(17) Narayanan, S., Levy C. “Streptococcus Group B Infections." eMedicine. 2006, Mar 24.http://www.emedicine.com/med/topic2185.htm
(18) Streptococcal infections : clinical aspects, microbiology, and molecular pathogenesis / edited by De New York : Oxford University Press, 2000. P. 223-230, 183-186.
(19) Boris, S., J. E. Suárez, F. Vásquez, and C. Barbés. 1998 Adherence of human vaginal lactobacilli to vaginal epithelial cells and interaction with uropathogens Infect. Immun. 66 1985–1989.
(20) Aroutcheva, Alla A, Simoes, Jose A., and Faro Sebastian. 2001. "Antimicrobial protein produced by vaginal Lactobacillus acidophilus that inhibits Gardnerella vaginalis"
(21) Nissl, Jan. “Vaginal Wet Mount.” Women’s Health. http://women.webmd.com/vaginal-wet-mount?page=3. 2006.
(22) "Gardnerella, Overview, Causes, Symptoms, Diagnosis, Treatment". Urology Channel. [http://www.urologychannel.com/std/gardnerella.shtml
(23) J D Wilson, E F Monteiro, and G R Kinghorn . Group B streptococci and vaginal discharge. PubMed Central. http://www.pubmedcentral.nih.gov/pagerender.fcgi?artid=1194041&pageindex=1
(24) "Fungi, Bacteria, Viruses." American Society for Microbiology. http://www.microbeworld.org/microbes/
(25) Ellen De Backer, Rita Verhelst, Hans Verstraelen, Geert Claeys, Gerda Verschraegen, Marleen Temmerman, and Mario Vaneechoutte. Antibiotic susceptibility of Atopobium vaginae. BMC Infect Dis. 2006; 6: 51. Published online 2006 March 16. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=16542416
(26) Xia Zhou, Celeste J. Brown, Zaid Abdo, Catherine C. Davis, Melanie A. Hansmann, Paul Joyce, James A. Foster and Larry J. Forney. Differences in the Composition of vaginal microbial communities found in healthy Cacuasian and Black Women. The ISME Journal (2007) pp.121-132. http://www.nature.com/ismej/journal/v1/n2/full/ismej200712a.html
(27) Callanan, M., Kaleta, P., O'Callaghan, J., O'Sullivan, O., Jordan, K., McAuliffe, O., Sangrador-Vegas, A., Slattery, L., F. Fitzgerald, G., Beresford, T., and R. Paul Ross “Genome Sequence of Lactobacillus helveticus, an Organism Distinguished by Selective Gene Loss and Insertion Sequence Element Expansion. Journal of Bacteriology, January 2008, p. 727-735, Vol. 190, No. 2.
(28) Jakobsson T, Forsum U. Changes in the predominant human Lactobacillus flora during in vitro fertilisation. http://www.ncbi.nlm.nih.gov/pubmed/18590533
(29) Hauth J.C., MacPherson C., Carey J.C., Klebanoff M.A., Hillier S.L., Ernest J.M., Leveno K.J., Wapner R., Varner M., Trout W., Moawad A., Sibai B. Early pregnancy threshold vaginal pH and Gram stain scores predictive of subsequent preterm birth in asymptomatic women(2003) American Journal of Obstetrics and Gynecology, 188 (3), pp. 831-835.
Edited by Jason Wong, Yumi Honda, Elieth Martinez, Raymond Villar, Eunice Kim, Whitney La, students of Rachel Larsen

