Pneumococcal meningitis and the role of Streptococcus pneumoniae
Introduction
By Avery Anderson
At right is a sample image insertion. It works for any image uploaded anywhere to MicrobeWiki. The insertion code consists of:
Double brackets: [[
Filename: PHIL_1181_lores.jpg
Thumbnail status: |thumb|
Pixel size: |300px|
Placement on page: |right|
Legend/credit: Electron micrograph of the Ebola Zaire virus. This was the first photo ever taken of the virus, on 10/13/1976. By Dr. F.A. Murphy, now at U.C. Davis, then at the CDC.
Closed double brackets: ]]
Other examples:
Bold
Italic
Subscript: H2O
Superscript: Fe3+
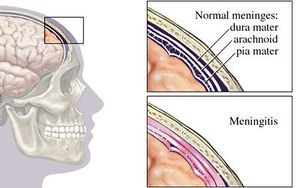
Bacterial meningitis is a potentially life-threatening disease of the central nervous system (CNS). It is characterized by inflammation of the membranes surrounding the brain and spinal cord, known as the meninges. The meninges include the pia mater, the arachnoid and the dura mater that encase and protect the brain and spinal cord. Figure 1 demonstrates the location of the meninges and shows a visual representation of inflammation that occurs during meningitis. The two leading causes of bacterial meningitis are Streptococcus pneumonia and Neisseria meningitidis [27]. Bacterial meningitis caused by Neisseria meningitidis is known as meningococcal meningitis while bacterial meningitis caused by Streptococcus pneumoniae is referred to as pneumococcal meningitis. Streptococcus pneumoniae accounts for two-thirds of all meningitis cases in the United States and Western Europe [1] and has the highest mortality rate of all other microorganisms causing meningitis [26]. In regions of the world where resources are scarce, fatality rates of pneumococcal meningitis near 51% and even in developed countries the rates are as high as 37% [7].
Streptococcus pneumoniae
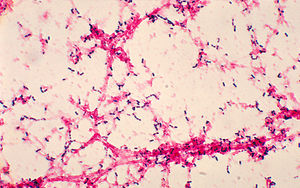
Streptococcus pneumoniae, also referred to as pneumococcus, is a gram-positive bacteria that belongs to the Firmicutes phylum. Figure 2 shows gram-stained S. pneumoniae grown on blood agar which is the frequent medium used in laboratories when researching this microorganism. It is a non-spore forming and non-motile bacteria [32]. Streptococcus pneumoniae most frequently are diplococci in structure, meaning they prefer to associate in pairs, but they can also be found individually or in short chains. Each individual cell measures between 0.5 and 1.25 micrometers in diameter [33]. Its optimal growth environment is 35-37 degrees Celsius [10]. This microorganism contains a circular genome with over 2 million base pairs [35]. Different strains of the bacteria can vary up to 10% in genetic information, but are consistent with a reoccurring set of 1553 genes [35]. Pneumococci are facultative anaerobes having the flexibility to ferment glucose into lactic acid for energy or utilize aerobic respiration for energy depending on the amount of oxygen available in its environment [32]. S. pneumoniae has the ability to oxidize hemoglobin characterizing it as an alpha-hemolytic bacteria. Its alpha-hemolytic property lends itself to laboratory identification of the microorganism since it can induce hemolysis on blood agar and, thus, appears green [33].
Streptococcus pneumoniae can live naturally in the human nasopharynx without causing disease. However, commensal carriage rates directly affect the transmission of S. pneumoniae [31] within any given population. Meningitis is sometimes said to be community-acquired because the carriage rates of S. pneumoniae increase in crowded situations. For example, children, who typically have the highest carriage rates nearing 37%, in crowded environments like that of day care centers have carriage rates that can reach as high as 58% [27]. Likewise, 50-60% of adult service personnel on military bases are likely to be carriers compared to the 5-10% of all healthy adults without children [11].
Pathogenic S. pneumoniae are encapsulated in polysaccharides whereas commensal S. pneumoniae do not have the same capsule. This capsule proves to be important to the virulence of the microorganism [11] in evading the human immune responses. When pathogenic, S. pneumoniae is responsible for pneumococcal disease, which includes meningitis, pneumonia, parapneumonic empyema, occult bacteremia, sepsis, arthritis, peritonitis, and endophthalmitis [3]. Transmission of S. pneumoniae most often occurs through respiratory droplets, in other words coughing or sneezing [11], making the means of contracting pneumococcal disease dangerously easy.
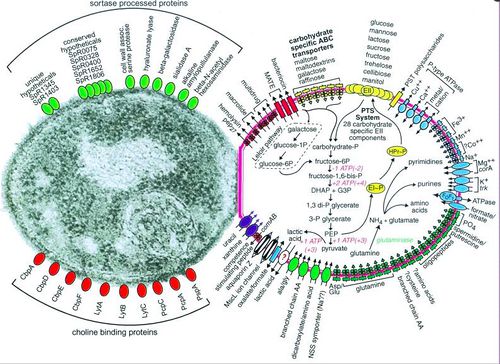
Pneumococci has over 93 known serotypes that are differentiated based on the composition of capsular polysaccharide [9]. Only a few of these serotypes account for the majority of disease causing agents worldwide including serotypes 1, 5, 6A, 6B, 14, 19F, and 23F [20]. The serotype responsible for pneumococcal meningitis outbreaks in the African meningitis belt is serotype 1 [20].
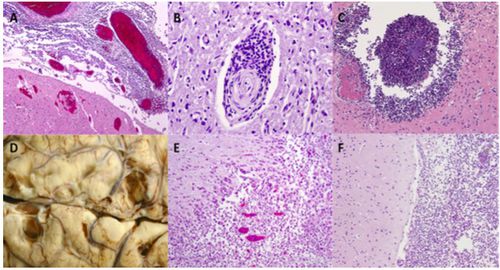
Pneumococcal Meningitis Pathogenesis
Include some current research, with at least one figure showing data.
Interaction with other microbial species
Include some current research, with at least one figure showing data.
Symptoms & Diagnosis
Include some current research, with at least one figure showing data.
Risk Factors
Neurological sequelae
Treatment & Adjunctive Therapies
Conclusion
References
[1] Hodgkin, J. and Partridge, F.A. "Caenorhabditis elegans meets microsporidia: the nematode killers from Paris." 2008. PLoS Biology 6:2634-2637.
Authored for BIOL 238 Microbiology, taught by Joan Slonczewski, 2015, Kenyon College.
